Can an “old school” vaccine address global inequities in Covid-19 vaccination?

Scientists at Baylor College of Medicine developed a vaccine called Corbevax that, unlike mRNA vaccines, can be mass produced using technology already in place in low- and middle-income countries. It's now being administered in India to children aged 12-14.
When the COVID-19 pandemic began invading the world in late 2019, Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. The scientists, with their prior experience of developing inexpensive vaccines for the world’s poor, had anticipated that the global rollout of Covid-19 jabs would be marked with several inequities. They wanted to create a patent-free vaccine to bridge this gap, but the U.S. government did not seem impressed, forcing the researchers to turn to private philanthropies for funds.
Hotez and Bottazzi, both scientists at the Texas Children’s Hospital Center for Vaccine Development at Baylor College of Medicine, raised about $9 million in private funds. Meanwhile, the U.S. government’s contribution stood at $400,000.
“That was a very tough time early on in the pandemic, you know, trying to do the work and raise the money for it at the same time,” says Hotez, who was nominated in February for a Nobel Peace Prize with Bottazzi for their COVID-19 vaccine. He adds that at the beginning of the pandemic, governments emphasized speed, innovation and rapidly immunizing populations in North America and Europe with little consideration for poorer countries. “We knew this [vaccine] was going to be the answer to global vaccine inequality, but I just wish the policymakers had felt the same,” says Hotez.
Over the past two years, the world has witnessed 488 million COVID-19 infections and over 61 million deaths. Over 11 billion vaccine doses have been administered worldwide; however, the global rollout of COVID-19 vaccines is marked with alarming socio-economic inequities. For instance, 72 percent of the population in high-income countries has received at least one dose of the vaccine, whereas the number stands at 15 percent in low-income countries.
This inequity is worsening vulnerabilities across the world, says Lawrence Young, a virologist and co-lead of the Warwick Health Global Research Priority at the UK-based University of Warwick. “As long as the virus continues to spread and replicate, particularly in populations who are under-vaccinated, it will throw up new variants and these will remain a continual threat even to those countries with high rates of vaccination,” says Young, “Therefore, it is in all our interests to ensure that vaccines are distributed equitably across the world.”
“When your house is on fire, you don't call the patent attorney,” says Hotez. “We wanted to be the fire department.”
The vaccine developed by Hotez and Bottazzi recently received emergency use authorisation in India, which plans to manufacture 100 million doses every month. Dubbed ‘Corbevax’ by its Indian maker, Biological E Limited, the vaccine is now being administered in India to children aged 12-14. The patent-free arrangement means that other low- and middle-income countries could also produce and distribute the vaccine locally.
“When your house is on fire, you don't call the patent attorney, you call the fire department,” says Hotez, commenting on the intellectual property rights waiver. “We wanted to be the fire department.”
The Inequity
Vaccine equity simply means that all people, irrespective of their location, should have equal access to vaccines. However, data suggests that the global COVID-19 vaccine rollout has favoured those in richer countries. For instance, high-income countries like the UAE, Portugal, Chile, Singapore, Australia, Malta, Hong Kong and Canada have partially vaccinated over 85 percent of their populations. This percentage in poorer countries, meanwhile, is abysmally low – 2.1 percent in Yemen, 4.6 in South Sudan, 5 in Cameroon, 9.9 in Burkina Faso, 10 in Nigeria, 12 in Somalia, 12 in Congo, 13 in Afghanistan and 21 in Ethiopia.

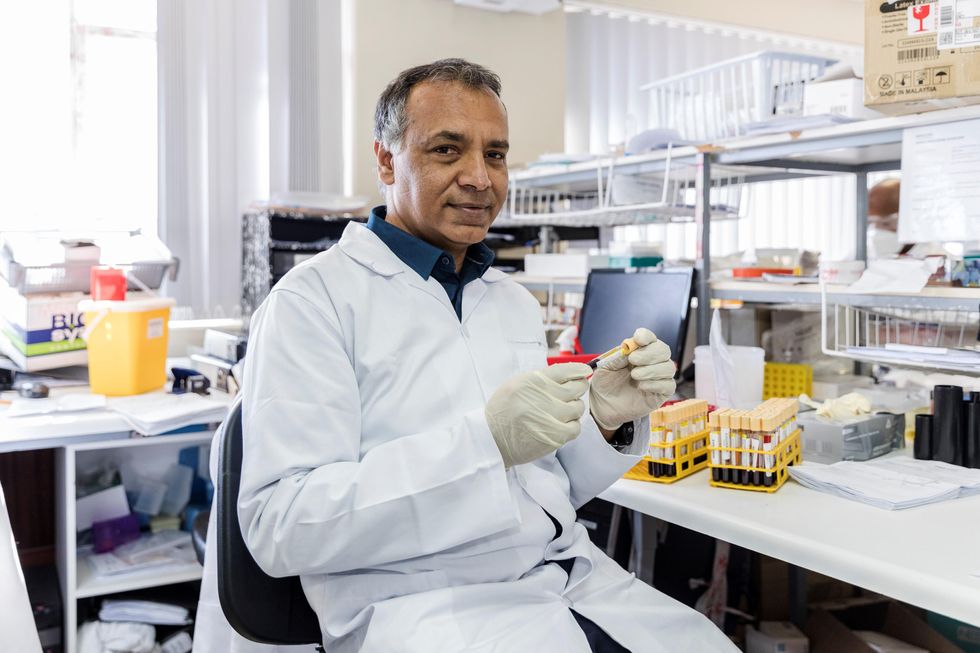
In late 2019, scientists Peter Hotez and Maria Elena Bottazzi set out to create a low-cost vaccine that would help inoculate populations in low- and middle-income countries. In February, they were nominated for a Nobel Peace Prize.
Texas Children's Hospital
The COVID-19 vaccination coverage is particularly low in African countries, and according to Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of African Local Initiative for Vaccinology Expertise, vaccine access and inequity remains a challenge in Africa. Madhi adds that a lack of vaccine access has affected the pandemic’s trajectory on the continent, but a majority of its people have now developed immunity through natural infection. “This has come at a high cost of loss of lives,” he says.
COVID-19 vaccines mean a significant financial burden for poorer countries, which spend an average of $41 per capita annually on health, while the average cost of every COVID-19 vaccine dose ranges between $2 and $40 in addition to a distribution cost of $3.70 per person for two doses. In December last year, the World Health Organisation (WHO) set a goal of immunizing 70 percent of the population of all countries by mid-2022. This, however, means that low-income countries would have to increase their health expenditure by an average of 56.6 percent to cover the cost, as opposed to 0.8 per cent in high-income countries.
Reflecting on the factors that have driven global inequity in COVID-19 vaccine distribution, Andrea Taylor, assistant director of programs at the Duke Global Health Innovation Center, says that wealthy nations took the risk of investing heavily in the development and scaling up of COVID-19 vaccines – at a time when there was little evidence to show that vaccines would work. This reserved a place for these nations at the front of the queue when doses started rolling off production lines. Lower-income countries, meanwhile, could not afford such investments.
“Now, however, global supply is not the issue,” says Taylor. “We are making plenty of doses to meet global need. The main problem is infrastructure to get the vaccine where it is most needed in a predictable and timely way and to ensure that countries have all the support they need to store, transport, and use the vaccine once it is received.”

Taufique Joarder, vice-chairperson of Bangladesh's Public Health Foundation, sees the need for more trials and data before Corbevax is made available to the general population.
In addition to global inequities in vaccination coverage, there are inequities within nations. Taufique Joarder, vice-chairperson of Bangladesh’s Public Health Foundation, points to the situation in his country, where vaccination coverage in rural and economically disadvantaged communities has suffered owing to weak vaccine-promotion initiatives and the difficulty many people face in registering online for jabs.
Joarder also cites the example of the COVID-19 immunization drive for children aged 12 years and above. “[Children] are given the Pfizer vaccine, which requires an ultralow temperature for storage. This is almost impossible to administer in many parts of the country, especially the rural areas. So, a large proportion of the children are being left out of vaccination,” says Joarder, adding that Corbevax, which is cheaper and requires regular temperature refrigeration “can be an excellent alternative to Pfizer for vaccinating rural children.”
Corbevax vs. mRNA Vaccines
As opposed to most other COVID-19 vaccines, which use the new Messenger RNA (mRNA) vaccine technology, Corbevax is an “old school” vaccine, says Hotez. The vaccine is made through microbial fermentation in yeast, similar to the process used to produce the recombinant hepatitis B vaccine, which has been administered to children in several countries for decades. Hence, says Hotez, the technology to produce Corbevax at large scales is already in place in countries like Vietnam, Bangladesh, India, Indonesia, Brazil, Argentina, among many others.
“So if you want to rapidly develop and produce and empower low- and middle-income countries, this is the technology to do it,” he says.
“Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines," says Andrea Taylor.
The COVID-19 vaccines created by Pfizer-BioNTech and Moderna marked the first time that mRNA vaccine technology was approved for use. However, scientists like Young feel that there is “a need to be pragmatic and not seduced by new technologies when older, tried and tested approaches can also be effective.” Taylor, meanwhile, says that although mRNA vaccines have dominated the COVID-19 vaccine market in the U.S., “there is no clear grounding for this preference in the data we have so far.” She adds that there is also growing evidence that the immunity from these shots may not hold up as well over time as that of vaccines using different platforms.
“The mRNA vaccines are well suited to wealthy countries with sufficient ultra-cold storage and transportation infrastructure, but these vaccines are divas and do not travel well in the rest of the world,” says Taylor. “Global access to high-quality vaccines will require serious investment in other types of COVID-19 vaccines, such as the protein subunit platform used by Novavax and Corbevax. These require only standard refrigeration, can be manufactured using existing facilities all over the world, and are easy to transport.”
Joarder adds that Corbevax is cheaper due to the developers’ waived intellectual rights. It could also be used as a booster vaccine in Bangladesh, where only five per cent of the population has currently received booster doses. “If this vaccine is proved effective for heterologous boosting, [meaning] it works well and is well tolerated as a booster with other vaccines that are available in Bangladesh, this can be useful,” says Joarder.
According to Hotez, Corbevax can play several important roles - as a standalone adult or paediatric vaccine, and as a booster for other vaccines. Studies are underway to determine Corbevax’s effectiveness in these regards, he says.
Need for More Data
Biological E conducted two clinical trials involving 3000 subjects in India, and found Corbevax to be “safe and immunogenic,” with 90 percent effectiveness in preventing symptomatic infections from the original strain of COVID-19 and over 80 percent effectiveness against the Delta variant. The vaccine is currently in use in India, and according to Hotez, it’s in the pipeline at different stages in Indonesia, Bangladesh and Botswana.
However, Corbevax is yet to receive emergency use approval from the WHO. Experts such as Joarder see the need for more trials and data before it is made available to the general population. He says that while the WHO’s emergency approval is essential for global scale-up of the vaccine, we need data to determine age-stratified efficacy of the vaccine and whether it can be used for heterologous boosting with other vaccines. “According to the most recent data, the 100 percent circulating variant in Bangladesh is Omicron. We need to know how effective is Corbevax against the Omicron variant,” says Joarder.
Shabir Madhi, a vaccinologist at the University of the Witwatersrand, Johannesburg and co-director of the African Local Initiative for Vaccinology Expertise, says that a majority of people in Africa have now developed immunity through natural infection. “This has come at a high cost of loss of lives."
Shivan Parusnath
Others, meanwhile, believe that availing vaccines to poorer countries is not enough to resolve the inequity. Young, the Warwick virologist, says that the global vaccination rollout has also suffered from a degree of vaccine hesitancy, echoing similar observations by President Biden and Pfizer’s CEO. The problem can be blamed on poor communication about the benefits of vaccination. “The Corbevax vaccine [helps with the issues of] patent protection, vaccine storage and distribution, but governments need to ensure that their people are clearly informed.” Notably, however, some research has found higher vaccine willingness in lower-income countries than in the U.S.
Young also emphasized the importance of establishing local vaccination stations to improve access. For some countries, meanwhile, it may be too late. Speaking about the African continent, Madhi says that Corbevax has arrived following the peak of the crisis and won’t reverse the suffering and death that has transpired because of vaccine hoarding by high-income countries.
“The same goes for all the sudden donations from countries such as France - pretty much of little to no value when the pandemic is at its tail end,” says Madhi. “This, unfortunately, is a repeat of the swine flu pandemic in 2009, when vaccines only became available to Africa after the pandemic had very much subsided.”
Clever Firm Predicts Patients Most at Risk, Then Tries to Intervene Before They Get Sicker
Health firm Populytics tracks and analyzes patient data, and makes care suggestions based on that data.
The diabetic patient hit the danger zone.
Ideally, blood sugar, measured by an A1C test, rests at 5.9 or less. A 7 is elevated, according to the Diabetes Council. Over 10, and you're into the extreme danger zone, at risk of every diabetic crisis from kidney failure to blindness.
In three months of working with a case manager, Jen's blood sugar had dropped to 7.2, a much safer range.
This patient's A1C was 10. Let's call her Jen for the sake of this story. (Although the facts of her case are real, the patient's actual name wasn't released due to privacy laws.).
Jen happens to live in Pennsylvania's Lehigh Valley, home of the nonprofit Lehigh Valley Health Network, which has eight hospital campuses and various clinics and other services. This network has invested more than $1 billion in IT infrastructure and founded Populytics, a spin-off firm that tracks and analyzes patient data, and makes care suggestions based on that data.
When Jen left the doctor's office, the Populytics data machine started churning, analyzing her data compared to a wealth of information about future likely hospital visits if she did not comply with recommendations, as well as the potential positive impacts of outreach and early intervention.
About a month after Jen received the dangerous blood test results, a community outreach specialist with psychological training called her. She was on a list generated by Populytics of follow-up patients to contact.
"It's a very gentle conversation," says Cathryn Kelly, who manages a care coordination team at Populytics. "The case manager provides them understanding and support and coaching." The goal, in this case, was small behavioral changes that would actually stick, like dietary ones.
In three months of working with a case manager, Jen's blood sugar had dropped to 7.2, a much safer range. The odds of her cycling back to the hospital ER or veering into kidney failure, or worse, had dropped significantly.
While the health network is extremely localized to one area of one state, using data to inform precise medical decision-making appears to be the wave of the future, says Ann Mongovern, the associate director of Health Care Ethics at the Markkula Center for Applied Ethics at Santa Clara University in California.
"Many hospitals and hospital systems don't yet try to do this at all, which is striking given where we're at in terms of our general technical ability in this society," Mongovern says.
How It Happened
While many hospitals make money by filling beds, the Lehigh Valley Health Network, as a nonprofit, accepts many patients on Medicaid and other government insurances that don't cover some of the costs of a hospitalization. The area's population is both poorer and older than national averages, according to the U.S. Census data, meaning more people with higher medical needs that may not have the support to care for themselves. They end up in the ER, or worse, again and again.
In the early 2000s, LVHN CEO Dr. Brian Nester started wondering if his health network could develop a way to predict who is most likely to land themselves a pricey ICU stay -- and offer support before those people end up needing serious care.
Embracing data use in such specific ways also brings up issues of data security and patient safety.
"There was an early understanding, even if you go back to the (federal) balanced budget act of 1997, that we were just kicking the can down the road to having a functional financial model to deliver healthcare to everyone with a reasonable price," Nester says. "We've got a lot of people living longer without more of an investment in the healthcare trust."
Popultyics, founded in 2013, was the result of years of planning and agonizing over those population numbers and cost concerns.
"We looked at our own health plan," Nester says. Out of all the employees and dependants on the LVHN's own insurance network, "roughly 1.5 percent of our 25,000 people — under 400 people — drove $30 million of our $130 million on insurance costs -- about 25 percent."
"You don't have to boil the ocean to take cost out of the system," he says. "You just have to focus on that 1.5%."
Take Jen, the diabetic patient. High blood sugar can lead to kidney failure, which can mean weekly expensive dialysis for 20 years. Investing in the data and staff to reach patients, he says, is "pennies compared to $100 bills."
For most doctors, "there's no awareness for providers to know who they should be seeing vs. who they are seeing. There's no incentive, because the incentive is to see as many patients as you can," he says.
To change that, first the LVHN invested in the popular medical management system, Epic. Then, they negotiated with the top 18 insurance companies that cover patients in the region to allow access to their patient care data, which means they have reams of patient history to feed the analytics machine in order to make predictions about outcomes. Nester admits not every hospital could do that -- with 52 percent of the market share, LVHN had a very strong negotiating position.
Third party services take that data and churn out analytics that feeds models and care management plans. All identifying information is stripped from the data.
"We can do predictive modeling in patients," says Populytics President and CEO Gregory Kile. "We can identify care gaps. Those care gaps are noted as alerts when the patient presents at the office."
Kile uses himself as a hypothetical patient.
"I pull up Gregory Kile, and boom, I see a flag or an alert. I see he hasn't been in for his last blood test. There is a care gap there we need to complete."
"There's just so much more you can do with that information," he says, envisioning a future where follow-up for, say, knee replacement surgery and outcomes could be tracked, and either validated or changed.
Ethical Issues at the Forefront
Of course, embracing data use in such specific ways also brings up issues of security and patient safety. For example, says medical ethicist Mongovern, there are many touchpoints where breaches could occur. The public has a growing awareness of how data used to personalize their experiences, such as social media analytics, can also be monetized and sold in ways that benefit a company, but not the user. That's not to say data supporting medical decisions is a bad thing, she says, just one with potential for public distrust if not handled thoughtfully.
"You're going to need to do this to stay competitive," she says. "But there's obviously big challenges, not the least of which is patient trust."
So far, a majority of the patients targeted – 62 percent -- appear to embrace the effort.
Among the ways the LVHN uses the data is monthly reports they call registries, which include patients who have just come in contact with the health network, either through the hospital or a doctor that works with them. The community outreach team members at Populytics take the names from the list, pull their records, and start calling. So far, a majority of the patients targeted – 62 percent -- appear to embrace the effort.
Says Nester: "Most of these are vulnerable people who are thrilled to have someone care about them. So they engage, and when a person engages in their care, they take their insulin shots. It's not rocket science. The rocket science is in identifying who the people are — the delivery of care is easy."
In The Fake News Era, Are We Too Gullible? No, Says Cognitive Scientist
Cognitive scientist Hugo Mercier says the real challenge is not fighting fake news, but figuring out "how to make it easier for people who say correct things to convince people."
One of the oddest political hoaxes of recent times was Pizzagate, in which conspiracy theorists claimed that Hillary Clinton and her 2016 campaign chief ran a child sex ring from the basement of a Washington, DC, pizzeria.
To fight disinformation more effectively, he suggests, humans need to stop believing in one thing above all: our own gullibility.
Millions of believers spread the rumor on social media, abetted by Russian bots; one outraged netizen stormed the restaurant with an assault rifle and shot open what he took to be the dungeon door. (It actually led to a computer closet.) Pundits cited the imbroglio as evidence that Americans had lost the ability to tell fake news from the real thing, putting our democracy in peril.
Such fears, however, are nothing new. "For most of history, the concept of widespread credulity has been fundamental to our understanding of society," observes Hugo Mercier in Not Born Yesterday: The Science of Who We Trust and What We Believe (Princeton University Press, 2020). In the fourth century BCE, he points out, the historian Thucydides blamed Athens' defeat by Sparta on a demagogue who hoodwinked the public into supporting idiotic military strategies; Plato extended that argument to condemn democracy itself. Today, atheists and fundamentalists decry one another's gullibility, as do climate-change accepters and deniers. Leftists bemoan the masses' blind acceptance of the "dominant ideology," while conservatives accuse those who do revolt of being duped by cunning agitators.
What's changed, all sides agree, is the speed at which bamboozlement can propagate. In the digital age, it seems, a sucker is born every nanosecond.
The Case Against Credulity
Yet Mercier, a cognitive scientist at the Jean Nicod Institute in Paris, thinks we've got the problem backward. To fight disinformation more effectively, he suggests, humans need to stop believing in one thing above all: our own gullibility. "We don't credulously accept whatever we're told—even when those views are supported by the majority of the population, or by prestigious, charismatic individuals," he writes. "On the contrary, we are skilled at figuring out who to trust and what to believe, and, if anything, we're too hard rather than too easy to influence."
He bases those contentions on a growing body of research in neuropsychiatry, evolutionary psychology, and other fields. Humans, Mercier argues, are hardwired to balance openness with vigilance when assessing communicated information. To gauge a statement's accuracy, we instinctively test it from many angles, including: Does it jibe with what I already believe? Does the speaker share my interests? Has she demonstrated competence in this area? What's her reputation for trustworthiness? And, with more complex assertions: Does the argument make sense?
This process, Mercier says, enables us to learn much more from one another than do other animals, and to communicate in a far more complex way—key to our unparalleled adaptability. But it doesn't always save us from trusting liars or embracing demonstrably false beliefs. To better understand why, leapsmag spoke with the author.
How did you come to write Not Born Yesterday?
In 2010, I collaborated with the cognitive scientist Dan Sperber and some other colleagues on a paper called "Epistemic Vigilance," which laid out the argument that evolutionarily, it would make no sense for humans to be gullible. If you can be easily manipulated and influenced, you're going to be in major trouble. But as I talked to people, I kept encountering resistance. They'd tell me, "No, no, people are influenced by advertising, by political campaigns, by religious leaders." I started doing more research to see if I was wrong, and eventually I had enough to write a book.
With all the talk about "fake news" these days, the topic has gotten a lot more timely.
Yes. But on the whole, I'm skeptical that fake news matters very much. And all the energy we spend fighting it is energy not spent on other pursuits that may be better ways of improving our informational environment. The real challenge, I think, is not how to shut up people who say stupid things on the internet, but how to make it easier for people who say correct things to convince people.
"History shows that the audience's state of mind and material conditions matter more than the leader's powers of persuasion."
You start the book with an anecdote about your encounter with a con artist several years ago, who scammed you out of 20 euros. Why did you choose that anecdote?
Although I'm arguing that people aren't generally gullible, I'm not saying we're completely impervious to attempts at tricking us. It's just that we're much better than we think at resisting manipulation. And while there's a risk of trusting someone who doesn't deserve to be trusted, there's also a risk of not trusting someone who could have been trusted. You miss out on someone who could help you, or from whom you might have learned something—including figuring out who to trust.
You argue that in humans, vigilance and open-mindedness evolved hand-in-hand, leading to a set of cognitive mechanisms you call "open vigilance."
There's a common view that people start from a state of being gullible and easy to influence, and get better at rejecting information as they become smarter and more sophisticated. But that's not what really happens. It's much harder to get apes than humans to do anything they don't want to do, for example. And research suggests that over evolutionary time, the better our species became at telling what we should and shouldn't listen to, the more open to influence we became. Even small children have ways to evaluate what people tell them.
The most basic is what I call "plausibility checking": if you tell them you're 200 years old, they're going to find that highly suspicious. Kids pay attention to competence; if someone is an expert in the relevant field, they'll trust her more. They're likelier to trust someone who's nice to them. My colleagues and I have found that by age 2 ½, children can distinguish between very strong and very weak arguments. Obviously, these skills keep developing throughout your life.
But you've found that even the most forceful leaders—and their propaganda machines—have a hard time changing people's minds.
Throughout history, there's been this fear of demagogues leading whole countries into terrible decisions. In reality, these leaders are mostly good at feeling the crowd and figuring out what people want to hear. They're not really influencing [the masses]; they're surfing on pre-existing public opinion. We know from a recent study, for instance, that if you match cities in which Hitler gave campaign speeches in the late '20s through early '30s with similar cities in which he didn't give campaign speeches, there was no difference in vote share for the Nazis. Nazi propaganda managed to make Germans who were already anti-Semitic more likely to express their anti-Semitism or act on it. But Germans who were not already anti-Semitic were completely inured to the propaganda.
So why, in totalitarian regimes, do people seem so devoted to the ruler?
It's not a very complex psychology. In these regimes, the slightest show of discontent can be punished by death, or by you and your whole family being sent to a labor camp. That doesn't mean propaganda has no effect, but you can explain people's obedience without it.
What about cult leaders and religious extremists? Their followers seem willing to believe anything.
Prophets and preachers can inspire the kind of fervor that leads people to suicidal acts or doomed crusades. But history shows that the audience's state of mind and material conditions matter more than the leader's powers of persuasion. Only when people are ready for extreme actions can a charismatic figure provide the spark that lights the fire.
Once a religion becomes ubiquitous, the limits of its persuasive powers become clear. Every anthropologist knows that in societies that are nominally dominated by orthodox belief systems—whether Christian or Muslim or anything else—most people share a view of God, or the spirit, that's closer to what you find in societies that lack such religions. In the Middle Ages, for instance, you have records of priests complaining of how unruly the people are—how they spend the whole Mass chatting or gossiping, or go on pilgrimages mostly because of all the prostitutes and wine-drinking. They continue pagan practices. They resist attempts to make them pay tithes. It's very far from our image of how much people really bought the dominant religion.
"The mainstream media is extremely reliable. The scientific consensus is extremely reliable."
And what about all those wild rumors and conspiracy theories on social media? Don't those demonstrate widespread gullibility?
I think not, for two reasons. One is that most of these false beliefs tend to be held in a way that's not very deep. People may say Pizzagate is true, yet that belief doesn't really interact with the rest of their cognition or their behavior. If you really believe that children are being abused, then trying to free them is the moral and rational thing to do. But the only person who did that was the guy who took his assault weapon to the pizzeria. Most people just left one-star reviews of the restaurant.
The other reason is that most of these beliefs actually play some useful role for people. Before any ethnic massacre, for example, rumors circulate about atrocities having been committed by the targeted minority. But those beliefs aren't what's really driving the phenomenon. In the horrendous pogrom of Kishinev, Moldova, 100 years ago, you had these stories of blood libel—a child disappeared, typical stuff. And then what did the Christian inhabitants do? They raped the [Jewish] women, they pillaged the wine stores, they stole everything they could. They clearly wanted to get that stuff, and they made up something to justify it.
Where do skeptics like climate-change deniers and anti-vaxxers fit into the picture?
Most people in most countries accept that vaccination is good and that climate change is real and man-made. These ideas are deeply counter-intuitive, so the fact that scientists were able to get them across is quite fascinating. But the environment in which we live is vastly different from the one in which we evolved. There's a lot more information, which makes it harder to figure out who we can trust. The main effect is that we don't trust enough; we don't accept enough information. We also rely on shortcuts and heuristics—coarse cues of trustworthiness. There are people who abuse these cues. They may have a PhD or an MD, and they use those credentials to help them spread messages that are not true and not good. Mostly, they're affirming what people want to believe, but they may also be changing minds at the margins.
How can we improve people's ability to resist that kind of exploitation?
I wish I could tell you! That's literally my next project. Generally speaking, though, my advice is very vanilla. The mainstream media is extremely reliable. The scientific consensus is extremely reliable. If you trust those sources, you'll go wrong in a very few cases, but on the whole, they'll probably give you good results. Yet a lot of the problems that we attribute to people being stupid and irrational are not entirely their fault. If governments were less corrupt, if the pharmaceutical companies were irreproachable, these problems might not go away—but they would certainly be minimized.

