The Nose Knows: Dogs Are Being Trained to Detect the Coronavirus

Security workers walk with detection dogs in an airport terminal.
Asher is eccentric and inquisitive. He loves an audience, likes keeping busy, and howls to be let through doors. He is a six-year-old working Cocker Spaniel, who, with five other furry colleagues, has now been trained to sniff body odor samples from humans to detect COVID-19 infections.
As the Delta variant and other new versions of the SARS-CoV-2 virus emerge, public health agencies are once again recommending masking while employers contemplate mandatory vaccination. While PCR tests remain the "gold standard" of COVID-19 tests, they can take hours to flag infections. To accelerate the process, scientists are turning to a new testing tool: sniffer dogs.
At the London School of Hygiene and Tropical Medicine (LSHTM), researchers deployed Asher and five other trained dogs to test sock samples from 200 asymptomatic, infected individuals and 200 healthy individuals. In May, they published the findings of the yearlong study in a preprint, concluding that dogs could identify COVID-19 infections with a high degree of accuracy – they could correctly identify a COVID-positive sample up to 94% of the time and a negative sample up to 92% of the time. The paper has yet to be peer-reviewed.
"Dogs can screen lots of people very quickly – 300 people per dog per hour. This means they could be used in places like airports or public venues like stadiums and maybe even workplaces," says James Logan, who heads the Department of Disease Control at LSHTM, adding that canines can also detect variants of SARS-CoV-2. "We included samples from two variants and the dogs could still detect them."
Detection dogs have been one of the most reliable biosensors for identifying the odor of human disease. According to Gemma Butlin, a spokesperson of Medical Detection Dogs, the UK-based charity that trained canines for the LSHTM study, the olfactory capabilities of dogs have been deployed to detect malaria, Parkinson's disease, different types of cancers, as well as pseudomonas, a type of bacteria known to cause infections in blood, lungs, eyes, and other parts of the human body.
COVID-19 has a distinctive smell — a result of chemicals known as volatile organic compounds released by infected body cells, which give off an odor "fingerprint."
"It's estimated that the percentage of a dog's brain devoted to analyzing odors is 40 times larger than that of a human," says Butlin. "Humans have around 5 million scent receptors dedicated to smell. Dogs have 350 million and can detect odors at parts per trillion. To put this into context, a dog can detect a teaspoon of sugar in a million gallons of water: two Olympic-sized pools full."
According to LSHTM scientists, COVID-19 has a distinctive smell — a result of chemicals known as volatile organic compounds released by infected body cells, which give off an odor "fingerprint." Other studies, too, have revealed that the SARS-CoV-2 virus has a distinct olfactory signature, detectable in the urine, saliva, and sweat of infected individuals. Humans can't smell the disease in these fluids, but dogs can.
"Our research shows that the smell associated with COVID-19 is at least partly due to small and volatile chemicals that are produced by the virus growing in the body or the immune response to the virus or both," said Steve Lindsay, a public health entomologist at Durham University, whose team collaborated with LSHTM for the study. He added, "There is also a further possibility that dogs can actually smell the virus, which is incredible given how small viruses are."
In April this year, researchers from the University of Pennsylvania and collaborators published a similar study in the scientific journal PLOS One, revealing that detection dogs could successfully discriminate between urine samples of infected and uninfected individuals. The accuracy rate of canines in this study was 96%. Similarly, last December, French scientists found that dogs were 76-100% effective at identifying individuals with COVID-19 when presented with sweat samples.
Grandjean Dominique, a professor at France's National Veterinary School of Alfort, who led the French study, said that the researchers used two types of dogs — search and rescue dogs, as they can sniff sweat, and explosive detection dogs, because they're often used at airports to find bomb ingredients. Dogs may very well be as good as PCR tests, said Dominique, but the goal, he added, is not to replace these tests with canines.
In France, the government gave the green light to train hundreds of disease detection dogs and deploy them in airports. "They will act as mass pre-test, and only people who are positive will undergo a PCR test to check their level of infection and the kind of variant," says Dominique. He thinks the dogs will be able to decrease the amount of PCR testing and potentially save money.
Since the accuracy rate for bio-detection dogs is fairly high, scientists think they could prove to be a quick diagnosis and mass screening tool, especially at ports, airports, train stations, stadiums, and public gatherings. Countries like Finland, Thailand, UAE, Italy, Chile, India, Australia, Pakistan, Saudi Arabia, Switzerland, and Mexico are already training and deploying canines for COVID-19 detection. The dogs are trained to sniff the area around a person, and if they find the odor of COVID-19 they will sit or stand back from an individual as a signal that they've identified an infection.
While bio-detection dogs seem promising for cheap, large-volume screening, many of the studies that have been performed to date have been small and in controlled environments. The big question is whether this approach work on people in crowded airports, not just samples of shirts and socks in a lab.
"The next step is 'real world' testing where they [canines] are placed in airports to screen people and see how they perform," says Anna Durbin, professor of international health at the John Hopkins Bloomberg School of Public Health. "Testing in real airports with lots of passengers and competing scents will need to be done."
According to Butlin of Medical Detection Dogs, scalability could be a challenge. However, scientists don't intend to have a dog in every waiting room, detecting COVID-19 or other diseases, she said.
"Dogs are the most reliable bio sensors on the planet and they have proven time and time again that they can detect diseases as accurately, if not more so, than current technological diagnostics," said Butlin. "We are learning from them all the time and what their noses know will one day enable the creation an 'E-nose' that does the same job – imagine a day when your mobile phone can tell you that you are unwell."
Tech-related injuries are becoming more common as many people depend on - and often develop addictions for - smart phones and computers.
In the 1990s, a mysterious virus spread throughout the Massachusetts Institute of Technology Artificial Intelligence Lab—or that’s what the scientists who worked there thought. More of them rubbed their aching forearms and massaged their cricked necks as new computers were introduced to the AI Lab on a floor-by-floor basis. They realized their musculoskeletal issues coincided with the arrival of these new computers—some of which were mounted high up on lab benches in awkward positions—and the hours spent typing on them.
Today, these injuries have become more common in a society awash with smart devices, sleek computers, and other gadgets. And we don’t just get hurt from typing on desktop computers; we’re massaging our sore wrists from hours of texting and Facetiming on phones, especially as they get bigger in size.
In 2007, the first iPhone measured 3.5-inches diagonally, a measurement known as the display size. That’s been nearly doubled by the newest iPhone 13 Pro, which has a 6.7-inch display. Other phones, too, like the Google Pixel 6 and the Samsung Galaxy S22, have bigger screens than their predecessors. Physical therapists and orthopedic surgeons have had to come up with names for a variety of new conditions: selfie elbow, tech neck, texting thumb. Orthopedic surgeon Sonya Sloan says she sees selfie elbow in younger kids and in women more often than men. She hears complaints related to technology once or twice a day.
The addictive quality of smartphones and social media means that people spend more time on their devices, which exacerbates injuries. According to Statista, 68 percent of those surveyed spent over three hours a day on their phone, and almost half spent five to six hours a day. Another report showed that people dedicate a third of their day to checking their phones, while the Media Effects Research Laboratory at Pennsylvania State University has found that bigger screens, ideal for entertainment purposes, immerse their users more than smaller screens. Oversized screens also provide easier navigation and more space for those with bigger hands or trouble seeing.
But others with conditions like arthritis can benefit from smaller phones. In March of 2016, Apple released the iPhone SE with a display size of 4.7 inches—an inch smaller than the iPhone 7, released that September. Apple has since come out with two more versions of the diminutive iPhone SE, one in 2020 and another in 2022.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable?
Kavin Senapathy, a freelance science journalist, has the Google Pixel 6. She was drawn to the phone because Google marketed the Pixel 6’s camera as better at capturing different skin tones. But this phone boasts one of the largest display sizes on the market: 6.4 inches.
Senapathy was diagnosed with carpal and cubital tunnel syndromes in 2017 and fibromyalgia in 2019. She has had to create a curated ergonomic workplace setup, otherwise her wrists and hands get weak and tingly, and she’s had to adjust how she holds her phone to prevent pain flares.
Recently, Senapathy underwent an electromyography, or an EMG, in which doctors insert electrodes into muscles to measure their electrical activity. The electrical response of the muscles tells doctors whether the nerve cells and muscles are successfully communicating. Depending on her results, steroid shots and even surgery might be required. Senapathy wants to stick with her Pixel 6, but the pain she’s experiencing may push her to buy a smaller phone. Unfortunately, options for these modestly sized phones are more limited.
These devices are now an inextricable part of our lives. So where does the burden of responsibility lie? Is it with consumers like Senapathy to adjust body positioning, get ergonomic workstations, and change habits to abate tech-related pain? Or should tech companies be held accountable for creating addictive devices that lead to musculoskeletal injury?

Kavin Senapathy, a freelance journalist, bought the Google Pixel 6 because of its high-quality camera, but she’s had to adjust how she holds the oversized phone to prevent pain flares.
Kavin Senapathy
A one-size-fits-all mentality for smartphones will continue to lead to injuries because every user has different wants and needs. S. Shyam Sundar, the founder of Penn State’s lab on media effects and a communications professor, says the needs for mobility and portability conflict with the desire for greater visibility. “The best thing a company can do is offer different sizes,” he says.
Joanna Bryson, an AI ethics expert and professor at The Hertie School of Governance in Berlin, Germany, echoed these sentiments. “A lot of the lack of choice we see comes from the fact that the markets have consolidated so much,” she says. “We want to make sure there’s sufficient diversity [of products].”
Consumers can still maintain some control despite the ubiquity of tech. Sloan, the orthopedic surgeon, has to pester her son to change his body positioning when using his tablet. Our heads get heavier as they bend forward: at rest, they weigh 12 pounds, but bent 60 degrees, they weigh 60. “I have to tell him, ‘Raise your head, son!’” she says. It’s important, Sloan explains, to consider that growth and development will affect ligaments and bones in the neck, potentially making kids even more vulnerable to injuries from misusing gadgets. She recommends that parents limit their kids’ tech time to alleviate strain. She also suggested that tech companies implement a timer to remind us to change our body positioning.
In 2017, Nan-Wei Gong, a former contractor for Google, founded Figur8, which uses wearable trackers to measure muscle function and joint movement. It’s like physical therapy with biofeedback. “Each unique injury has a different biomarker,” says Gong. “With Figur8, you are comparing yourself to yourself.” This allows an individual to self-monitor for wear and tear and strengthen an injury in a way that’s efficient and designed for their body. Gong noticed that the work-from-home model during the COVID-19 pandemic created a new set of ergonomic problems that resulted in injuries. Figur8 provides real-time data for these injuries because “behavioral change requires feedback.”
Gong worked on a project called Jacquard while at Google. Textile experts weave conductive thread into their fabric, and the result is a patch of the fabric—like the cuff of a Levi’s jacket—that responds to commands on your smartphone. One swipe can call your partner or check the weather. It was designed with cyclists in mind who can’t easily check their phones, and it’s part of a growing movement in the tech industry to deliver creative, hands-free design. Gong thinks that engineers at large corporations like Google have accessibility in mind; it’s part of what drives their decisions for new products.
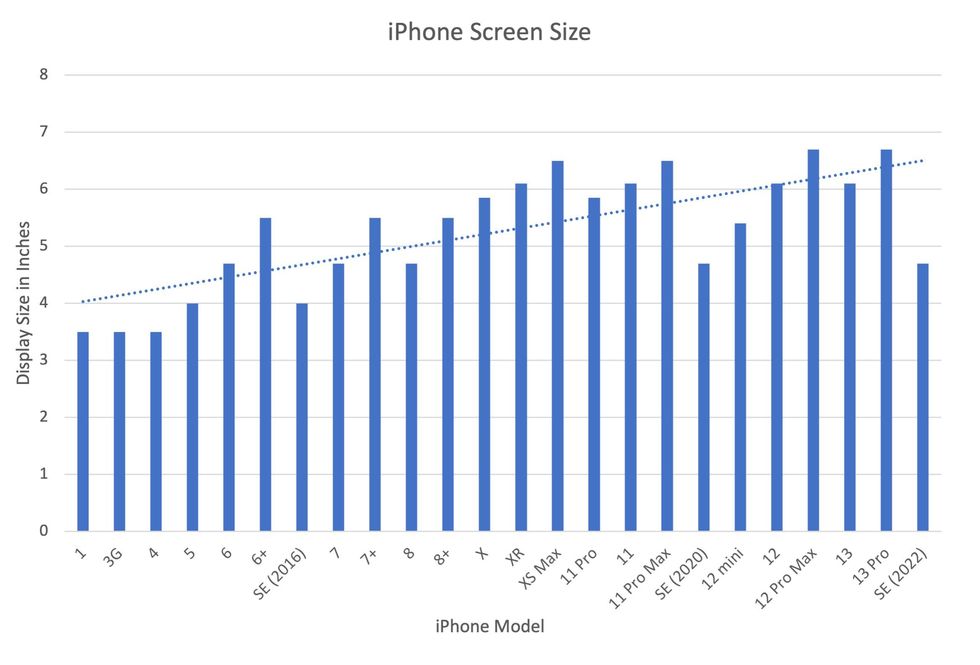
Display sizes of iPhones have become larger over time.
Sourced from Screenrant https://screenrant.com/iphone-apple-release-chronological-order-smartphone/ and Apple Tech Specs: https://www.apple.com/iphone-se/specs/
Back in Germany, Joanna Bryson reminds us that products like smartphones should adhere to best practices. These rules may be especially important for phones and other products with AI that are addictive. Disclosure, accountability, and regulation are important for AI, she says. “The correct balance will keep changing. But we have responsibilities and obligations to each other.” She was on an AI Ethics Council at Google, but the committee was disbanded after only one week due to issues with one of their members.
Bryson was upset about the Council’s dissolution but has faith that other regulatory bodies will prevail. OECD.AI, and international nonprofit, has drafted policies to regulate AI, which countries can sign and implement. “As of July 2021, 46 governments have adhered to the AI principles,” their website reads.
Sundar, the media effects professor, also directs Penn State’s Center for Socially Responsible AI. He says that inclusivity is a crucial aspect of social responsibility and how devices using AI are designed. “We have to go beyond first designing technologies and then making them accessible,” he says. “Instead, we should be considering the issues potentially faced by all different kinds of users before even designing them.”
Entomologist Jessica Ware is using new technologies to identify insect species in a changing climate. She shares her suggestions for how we can live harmoniously with creeper crawlers everywhere.
Jessica Ware is obsessed with bugs.
My guest today is a leading researcher on insects, the president of the Entomological Society of America and a curator at the American Museum of Natural History. Learn more about her here.
You may not think that insects and human health go hand-in-hand, but as Jessica makes clear, they’re closely related. A lot of people care about their health, and the health of other creatures on the planet, and the health of the planet itself, but researchers like Jessica are studying another thing we should be focusing on even more: how these seemingly separate areas are deeply entwined. (This is the theme of an upcoming event hosted by Leaps.org and the Aspen Institute.)
Listen to the Episode
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google

Entomologist Jessica Ware
D. Finnin / AMNH
Maybe it feels like a core human instinct to demonize bugs as gross. We seem to try to eradicate them in every way possible, whether that’s with poison, or getting out our blood thirst by stomping them whenever they creep and crawl into sight.
But where did our fear of bugs really come from? Jessica makes a compelling case that a lot of it is cultural, rather than in-born, and we should be following the lead of other cultures that have learned to live with and appreciate bugs.
The truth is that a healthy planet depends on insects. You may feel stung by that news if you hate bugs. Reality bites.
Jessica and I talk about whether learning to live with insects should include eating them and gene editing them so they don’t transmit viruses. She also tells me about her important research into using genomic tools to track bugs in the wild to figure out why and how we’ve lost 50 percent of the insect population since 1970 according to some estimates – bad news because the ecosystems that make up the planet heavily depend on insects. Jessica is leading the way to better understand what’s causing these declines in order to start reversing these trends to save the insects and to save ourselves.

