Democratize the White Coat by Honoring Black, Indigenous, and People of Color in Science

Celebrating BIPOC's achievements in science are a strong first step to make science a guiding force for all.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
Journalists, educators, and curators have responded to Black Lives Matter by highlighting the history and achievements of Black Americans in a variety of fields, including science. The movement has also sparked important demands to address longstanding scientific inequities such as lack of access to quality healthcare and the disproportionate impact of climate change and environmental pollution on neighborhoods of Black, Indigenous, and people of color (BIPOC). Making such improvements requires bringing BIPOC into science and into positions of leadership in laboratories, graduate schools, medical practices, and clinical trials. The moment is right to challenge scientific gatekeepers to respond to Black Lives Matter by widening the pathways that determine who becomes a scientist, a researcher, or a clinician.
The scientific workforce has long lacked diversity, which in turn discourages Black people from pursuing such careers. Causes include a dearth of mentors and role models, preconceived notions that science is exclusive to white males, and subpar STEM education. Across race, gender, class, ability, and all other dimensions that inform how an individual navigates the world, from the familial to the global level, seeing role models who resemble you impacts what you strive for and believe possible. As Marian Wright Edelman stated, "You can't be what you can't see"—a truth with ever-increasing resonance since the U.S. is projected to be minority-white by 2045.
Black Americans have paved the way for the nation to lead in science and technology, despite marginalization and exclusion from textbooks. Physicist Dr. Shirley Ann Jackson invented the technology behind Caller I.D. and Call Waiting. Otis Boykin's patents made televisions and radios what they are today. Thanks to the 2017 movie Hidden Figures, millions of Americans know about Katherine Johnson, the NASA mathematician whose calculations were essential to the successful trajectory of the Apollo 11 mission.
However, highlighting past role models who were Black achievers is not enough and paints too static a picture—especially when examples of transformative work by contemporary BIPOC scientists serving BIPOC communities abound. Cognitive neuroscientist Dr. Jonathan Jackson founded the Community Access, Recruitment, & Engagement (CARE) Research Center with the goal to break down barriers so that people of color participate in clinical trials. Geneticist Dr. Nanibaa' Garrison's research creates ethical frameworks to overcome genomic injustices so Indigenous populations can benefit from genetic research. Computer scientists Joy Buolamwini and Dr. Timnit Gebru's research drew attention to reinforced racial bias in artificial intelligence, leading Microsoft, Amazon, and IBM this summer to halt use of their facial recognition software.
"Integration does not mean equality if the space being integrated isn't exuberantly down for the cause."
In order to honor concretely the ubiquitous public statements and commitments to justice and equity that flooded everyone's inboxes in early June, we must include traditionally underrepresented voices in all phases of science and its applications. For guidance, we would benefit from listening to activists leading, for example, climate marches and protests over toxic water. Indeed, science is at the core of the issues for which young BIPOC are mobilizing. We need to sit down with these individuals to gain their input on how the narratives, practices, and opportunities in science should change. As Zeena Abdulkarim, a youth climate change organizer working with Zero Hour, explains: "Minority communities are exposed to what the privileged and people in power are not; therefore these communities know the right steps to take in the change we need for the kickstart of true social and environmental justice."
Two other Black youth, for example, used the platform of the laboratory while in high school to mobilize for change. Elle Lanair Lett, now specializing in epidemiology as an M.D.-Ph.D. student in Philadelphia, was prompted by family prevalence of diabetes to research the genetics of pancreatic cells. Dr. Otana Jakpor, now an ophthalmology resident in Michigan, was motivated by the pollution in her hometown of Riverside, California, to research the pulmonary effects of indoor air purifiers, with findings that influenced California ozone regulations. Both became finalists in a national science fair, propelling them on paths toward science careers. These young scientists demonstrate how people's communities and lived experiences can shape trajectories of science research, which, in turn, determines which visions for society are materialized and popularized.
We can also gain insight from another childhood science fair veteran, self-proclaimed "Black STEMinist" Augusta Uwamanzu-Nna, who graduated from college in May and works as a bioengineer. In her view, "we need to shift the burden away from Black people and onto individuals who have contributed to our current reality—fundamentally requiring understanding, open-mindedness, a lack of bias, cultural competency, anti-racism, anti-homophobia, and many, many other things."
Celebrating BIPOC's accomplishments in science and cultivating new leadership today are strong first steps to make science a guiding force for all. Ms. Uwamanzu-Nna keenly reminds us, "Integration does not mean equality if the space being integrated isn't exuberantly down for the cause." Indeed, educational institutions, scientific companies, and medical centers must acknowledge and embrace their role in democratizing science in order for society to realize racial and scientific justice.
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Have You Heard of the Best Sport for Brain Health?
In this week's Friday Five, research points to this brain healthiest of sports. Plus, the natural way to reprogram cells to a younger state, the network that could underlie many different mental illnesses, and a new test could diagnose autism in newborns. Plus, scientists 3D print an ear and attach it to woman
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- Reprogram cells to a younger state
- Pick up this sport for brain health
- Do all mental illnesses have the same underlying cause?
- New test could diagnose autism in newborns
- Scientists 3D print an ear and attach it to woman
Can blockchain help solve the Henrietta Lacks problem?
Marielle Gross, a professor at the University of Pittsburgh, shows patients a new app that tracks how their samples are used during biomedical research.
Science has come a long way since Henrietta Lacks, a Black woman from Baltimore, succumbed to cervical cancer at age 31 in 1951 -- only eight months after her diagnosis. Since then, research involving her cancer cells has advanced scientific understanding of the human papilloma virus, polio vaccines, medications for HIV/AIDS and in vitro fertilization.
Today, the World Health Organization reports that those cells are essential in mounting a COVID-19 response. But they were commercialized without the awareness or permission of Lacks or her family, who have filed a lawsuit against a biotech company for profiting from these “HeLa” cells.
While obtaining an individual's informed consent has become standard procedure before the use of tissues in medical research, many patients still don’t know what happens to their samples. Now, a new phone-based app is aiming to change that.
Tissue donors can track what scientists do with their samples while safeguarding privacy, through a pilot program initiated in October by researchers at the Johns Hopkins Berman Institute of Bioethics and the University of Pittsburgh’s Institute for Precision Medicine. The program uses blockchain technology to offer patients this opportunity through the University of Pittsburgh's Breast Disease Research Repository, while assuring that their identities remain anonymous to investigators.
A blockchain is a digital, tamper-proof ledger of transactions duplicated and distributed across a computer system network. Whenever a transaction occurs with a patient’s sample, multiple stakeholders can track it while the owner’s identity remains encrypted. Special certificates called “nonfungible tokens,” or NFTs, represent patients’ unique samples on a trusted and widely used blockchain that reinforces transparency.
Blockchain could be used to notify people if cancer researchers discover that they have certain risk factors.
“Healthcare is very data rich, but control of that data often does not lie with the patient,” said Julius Bogdan, vice president of analytics for North America at the Healthcare Information and Management Systems Society (HIMSS), a Chicago-based global technology nonprofit. “NFTs allow for the encapsulation of a patient’s data in a digital asset controlled by the patient.” He added that this technology enables a more secure and informed method of participating in clinical and research trials.
Without this technology, de-identification of patients’ samples during biomedical research had the unintended consequence of preventing them from discovering what researchers find -- even if that data could benefit their health. A solution was urgently needed, said Marielle Gross, assistant professor of obstetrics, gynecology and reproductive science and bioethics at the University of Pittsburgh School of Medicine.
“A researcher can learn something from your bio samples or medical records that could be life-saving information for you, and they have no way to let you or your doctor know,” said Gross, who is also an affiliate assistant professor at the Berman Institute. “There’s no good reason for that to stay the way that it is.”
For instance, blockchain could be used to notify people if cancer researchers discover that they have certain risk factors. Gross estimated that less than half of breast cancer patients are tested for mutations in BRCA1 and BRCA2 — tumor suppressor genes that are important in combating cancer. With normal function, these genes help prevent breast, ovarian and other cells from proliferating in an uncontrolled manner. If researchers find mutations, it’s relevant for a patient’s and family’s follow-up care — and that’s a prime example of how this newly designed app could play a life-saving role, she said.
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app -- called de-bi, which is short for decentralized biobank -- before undergoing a mastectomy for early-stage breast cancer in November, after it was diagnosed on a routine mammogram. She often takes part in medical research and looks forward to tracking her tissues.
“Anytime there’s a scientific experiment or study, I’m quick to participate -- to advance my own wellness as well as knowledge in general,” said Burton, 49, a life insurance service representative who lives in Carnegie, Pa. “It’s my way of contributing.”
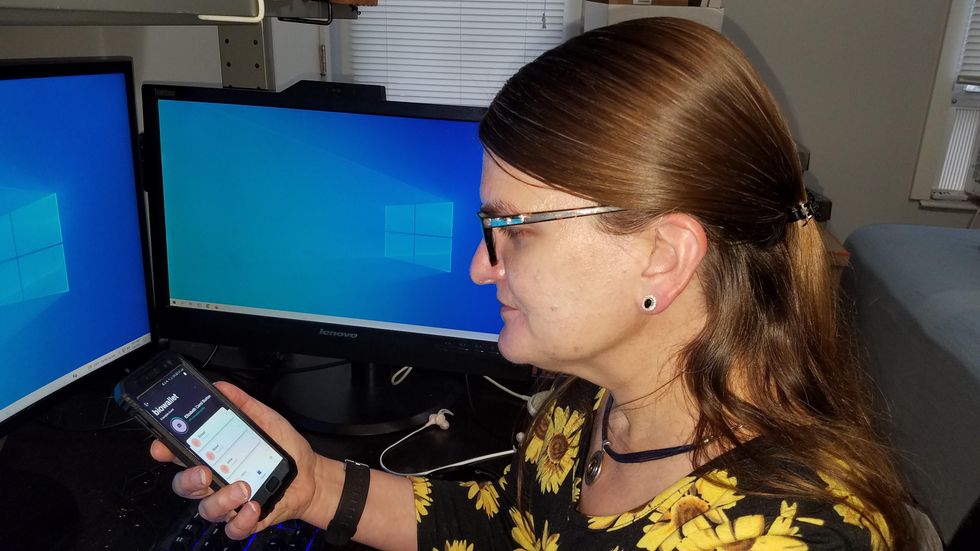
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app before undergoing a mastectomy for early-stage breast cancer.
Liz Burton
The pilot program raises the issue of what investigators may owe study participants, especially since certain populations, such as Black and indigenous peoples, historically were not treated in an ethical manner for scientific purposes. “It’s a truly laudable effort,” Tamar Schiff, a postdoctoral fellow in medical ethics at New York University’s Grossman School of Medicine, said of the endeavor. “Research participants are beautifully altruistic.”
Lauren Sankary, a bioethicist and associate director of the neuroethics program at Cleveland Clinic, agrees that the pilot program provides increased transparency for study participants regarding how scientists use their tissues while acknowledging individuals’ contributions to research.
However, she added, “it may require researchers to develop a process for ongoing communication to be responsive to additional input from research participants.”
Peter H. Schwartz, professor of medicine and director of Indiana University’s Center for Bioethics in Indianapolis, said the program is promising, but he wonders what will happen if a patient has concerns about a particular research project involving their tissues.
“I can imagine a situation where a patient objects to their sample being used for some disease they’ve never heard about, or which carries some kind of stigma like a mental illness,” Schwartz said, noting that researchers would have to evaluate how to react. “There’s no simple answer to those questions, but the technology has to be assessed with an eye to the problems it could raise.”
To truly make a difference, blockchain must enable broad consent from patients, not just de-identification.
As a result, researchers may need to factor in how much information to share with patients and how to explain it, Schiff said. There are also concerns that in tracking their samples, patients could tell others what they learned before researchers are ready to publicly release this information. However, Bogdan, the vice president of the HIMSS nonprofit, believes only a minimal study identifier would be stored in an NFT, not patient data, research results or any type of proprietary trial information.
Some patients may be confused by blockchain and reluctant to embrace it. “The complexity of NFTs may prevent the average citizen from capitalizing on their potential or vendors willing to participate in the blockchain network,” Bogdan said. “Blockchain technology is also quite costly in terms of computational power and energy consumption, contributing to greenhouse gas emissions and climate change.”
In addition, this nascent, groundbreaking technology is immature and vulnerable to data security flaws, disputes over intellectual property rights and privacy issues, though it does offer baseline protections to maintain confidentiality. To truly make a difference, blockchain must enable broad consent from patients, not just de-identification, said Robyn Shapiro, a bioethicist and founding attorney at Health Sciences Law Group near Milwaukee.
The Henrietta Lacks story is a prime example, Shapiro noted. During her treatment for cervical cancer at Johns Hopkins, Lacks’s tissue was de-identified (albeit not entirely, because her cell line, HeLa, bore her initials). After her death, those cells were replicated and distributed for important and lucrative research and product development purposes without her knowledge or consent.
Nonetheless, Shapiro thinks that the initiative by the University of Pittsburgh and Johns Hopkins has potential to solve some ethical challenges involved in research use of biospecimens. “Compared to the system that allowed Lacks’s cells to be used without her permission, Shapiro said, “blockchain technology using nonfungible tokens that allow patients to follow their samples may enhance transparency, accountability and respect for persons who contribute their tissue and clinical data for research.”
Read more about laws that have prevented people from the rights to their own cells.