How dozens of men across Alaska (and their dogs) teamed up to save one town from a deadly outbreak

In 1925, health officials in Alaska came up with a creative solution to save a remote fishing town from a deadly disease outbreak.
During the winter of 1924, Curtis Welch – the only doctor in Nome, a remote fishing town in northwest Alaska – started noticing something strange. More and more, the children of Nome were coming to his office with sore throats.
Initially, Welch dismissed the cases as tonsillitis or some run-of-the-mill virus – but when more kids started getting sick, with some even dying, he grew alarmed. It wasn’t until early 1925, after a three-year-old boy died just two weeks after becoming ill, that Welch realized that his worst suspicions were true. The boy – and dozens of other children in town – were infected with diphtheria.
A DEADLY BACTERIA
Diphtheria is nearly nonexistent and almost unheard of in industrialized countries today. But less than a century ago, diphtheria was a household name – one that struck fear in the heart of every parent, as it was extremely contagious and particularly deadly for children.
Diphtheria – a bacterial infection – is an ugly disease. When it strikes, the bacteria eats away at the healthy tissues in a patient’s respiratory tract, leaving behind a thick, gray membrane of dead tissue that covers the patient's nose, throat, and tonsils. Not only does this membrane make it very difficult for the patient to breathe and swallow, but as the bacteria spreads through the bloodstream, it causes serious harm to the heart and kidneys. It sometimes also results in nerve damage and paralysis. Even with treatment, diphtheria kills around 10 percent of people it infects. Young children, as well as adults over the age of 60, are especially at risk.
Welch didn’t suspect diphtheria at first. He knew the illness was incredibly contagious and reasoned that many more people would be sick – specifically, the family members of the children who had died – if there truly was an outbreak. Nevertheless, the symptoms, along with the growing number of deaths, were unmistakable. By 1925 Welch knew for certain that diphtheria had come to Nome.
In desperation, Welch tried treating an infected seven-year-old girl with some expired antitoxin – but she died just a few hours after he administered it.
AN INACCESSIBLE CURE
A vaccine for diphtheria wouldn’t be widely available until the mid-1930s and early 1940s – so an outbreak of the disease meant that each of the 10,000 inhabitants of Nome were all at serious risk.
One option was to use something called an antitoxin – a serum consisting of anti-diphtheria antibodies – to treat the patients. However, the town’s reserve of diphtheria antitoxin had expired. Welch had ordered a replacement shipment of antitoxin the previous summer – but the shipping port that was set to deliver the serum had been closed due to ice, and no new antitoxin would arrive before spring of 1925. In desperation, Welch tried treating an infected seven-year-old girl with some expired antitoxin – but she died just a few hours after he administered it.
Welch radioed for help to all the major towns in Alaska as well as the US Public Health Service in Washington, DC. His telegram read: An outbreak of diphtheria is almost inevitable here. I am in urgent need of one million units of diphtheria antitoxin. Mail is the only form of transportation.
FOUR-LEGGED HEROES
When the Alaskan Board of Health learned about the outbreak, the men rushed to devise a plan to get antitoxin to Nome. Dropping the serum in by airplane was impossible, as the available planes were unsuitable for flying during Alaska’s severe winter weather, where temperatures were routinely as cold as -50 degrees Fahrenheit.
In late January 1925, roughly 30,000 units of antitoxin were located in an Anchorage hospital and immediately delivered by train to a nearby city, Nenana, en route to Nome. Nenana was the furthest city that was reachable by rail – but unfortunately it was still more than 600 miles outside of Nome, with no transportation to make the delivery. Meanwhile, Welch had confirmed 20 total cases of diphtheria, with dozens more at high risk. Diphtheria was known for wiping out entire communities, and the entire town of Nome was in danger of suffering the same fate.
It was Mark Summer, the Board of Health superintendent, who suggested something unorthodox: Using a relay team of sled-racing dogs to deliver the antitoxin serum from Nenana to Nome. The Board quickly voted to accept Summer’s idea and set up a plan: The thousands of units of antitoxin serum would be passed along from team to team at different towns along the mail route from Nenana to Nome. When it reached a town called Nulato, a famed dogsled racer named Leonhard Seppala and his experienced team of huskies would take the serum more than 90 miles over the ice of Norton Sound, the longest and most treacherous part of the journey. Past the sound, the serum would change hands several times more before arriving in Nome.
Between January 27 and 31, the serum passed through roughly a dozen drivers and their dog sled teams, each of them carrying the serum between 20 and 50 miles to the next destination. Though each leg of the trip took less than a day, the sub-zero temperatures – sometimes as low as -85 degrees – meant that every driver and dog risked their lives. When the first driver, Bill Shannon, arrived at his checkpoint in Tolovana on January 28th, his nose was black with frostbite, and three of his dogs had died. The driver who relieved Bill Shannon, named Edgar Kalland, needed the owner of a local roadhouse to pour hot water over his hands to free them from the sled’s metal handlebar. Two more dogs from another relay team died before the serum was passed to Seppala at a town called Ungalik.
THE FINAL STRETCHES
Seppala and his team raced across the ice of the Norton Sound in the dead of night on January 31, with wind chill temperatures nearing an astonishing -90 degrees. The team traveled 84 miles in a single day before stopping to rest – and once rested, they set off again in the middle of the night through a raging winter storm. The team made it across the ice, as well as a 5,000-foot ascent up Little McKinley Mountain, to pass the serum to another driver in record time. The serum was now just 78 miles from Nome, and the death toll in town had reached 28.
The serum reached Gunnar Kaasen and his team of dogs on February 1st. Balto, Kaasen’s lead dog, guided the team heroically through a winter storm that was so severe Kaasen later reported not being able to see the dogs that were just a few feet ahead of him.
Visibility was so poor, in fact, that Kaasen ran his sled two miles past the relay point before noticing – and not wanting to lose a minute, he decided to forge on ahead rather than doubling back to deliver the serum to another driver. As they continued through the storm, the hurricane-force winds ripped past Kaasen’s sled at one point and toppled the sled – and the serum – overboard. The cylinder containing the antitoxin was left buried in the snow – and Kaasen tore off his gloves and dug through the tundra to locate it. Though it resulted in a bad case of frostbite, Kaasen eventually found the cylinder and kept driving.
Kaasen arrived at the next relay point on February 2nd, hours ahead of schedule. When he got there, however, he found the relay driver of the next team asleep. Kaasen took a risk and decided not to wake him, fearing that time would be wasted with the next driver readying his team. Kaasen, Balto, and the rest of the team forged on, driving another 25 miles before finally reaching Nome just before six in the morning. Eyewitnesses described Kaasen pulling up to the town’s bank and stumbling to the front of the sled. There, he collapsed in exhaustion, telling onlookers that Balto was “a damn fine dog.”
A LIVING LEGACY
Just a few hours after Balto’s heroic arrival in Nome, the serum had been thawed and was ready to administer to the patients with diphtheria. Amazingly, the relay team managed to complete the entire journey in just 127 hours – a world record at the time – without one serum vial damaged or destroyed. The serum shipment that arrived by dogsled – along with additional serum deliveries that followed in the next several weeks – were successful in stopping the outbreak in its tracks.
Balto and several other dogs – including Togo, the lead dog on Seppala’s team – were celebrated as local heroes after the race. Balto died in 1933, while the last of the human serum runners died in 1999 – but their legacy lives on: In early 2021, an all-female team of healthcare workers made the news by braving the Alaskan winter to deliver COVID-19 vaccines to people in rural North Alaska, traveling by bobsled and snowmobile – a heroic journey, and one that would have been unthinkable had Balto, Togo, and the 1925 sled runners not first paved the way.
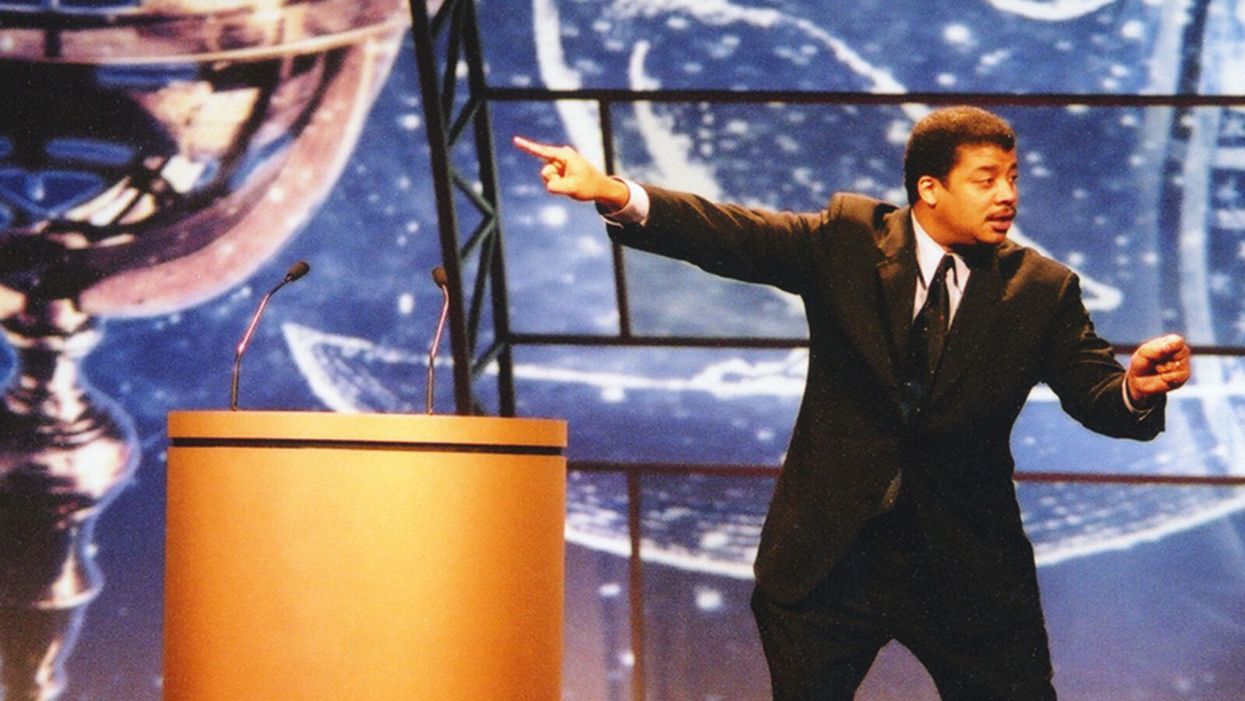
Neil deGrasse Tyson Wants Celebrities to Promote Scientists
Neil de Grasse Tyson wants fellow celebrities to point their followers to experts and organizations who know what they're talking about.
"President Kennedy was the first president to not wear a hat. Have you seen men wearing hats since then?" Neil deGrasse Tyson, one of the world's few astrophysicists with a household name, asks on the phone from his car. Well, no. "If I wear some cowboy hats, it's because it's the outfit, it's not because that's my standard equipment when I leave the home."
"We have classes on 100 things and none of them are on the ability to distinguish what is true and what is not."
But Tyson, who speaks in methodically reasoned paragraphs with lots of semi-rhetorical questions to make sure we're all still listening, isn't really making a point about Mad Men-era men's clothing trends. "Should a president influence fashion?" he says. "I think people sometimes don't know the full power they have over other people. So, that's the first prong in this comment. My second prong is, why would anyone take medical advice from a politician?"
Days before our conversation, news broke that President Trump said he was taking hydroxychloroquine, which he had hyped for months as a surefire magical cure for COVID-19 — the science just hadn't caught up to his predictions. But the science never did catch up; instead, it went the opposite direction, showing that hydroxychloroquine, when used to treat COVID-19 patients, actually led to an increased risk of death.
Alarm spread swiftly around the globe as experts cast the president's professed self-medicating as illogical and dangerous. However, it was just one of a series of wild pieces of medical advice espoused by Trump from his mighty pulpit, like that, hey, maybe disinfectants could cure people when injected into their bodies. (That also leads to death.)
But people do take medical advice from politicians. An Arizona man afraid of COVID-19 died after consuming chloroquine phosphate, which he and his wife had sitting on the back of a shelf after using it to treat koi fish for parasites. The pandemic has exposed many weaknesses in the feedback loop of society, government, the media, and science, including the difficulty of seeding accurate medical information with the masses. Many on the left and right decry a broken political and news media system, but Tyson believes the problem isn't mega-influencers like Trump. Rather it's the general public's desire to take their advice on complex topics – like the science of virology – that such influencers know nothing about.
Tyson's not upset with the public, who follow Trump's advice. "As an educator, I can't get angry with you," he says. Or even Trump himself. "Trump was elected by 60 million people, right? So, you could say all you want about Trump, kick him out of office, whatever. [There's] still the 60 million fellow Americans who walk among us who voted for him. So, what are you going to do with them?"
Tyson also isn't upset with Facebook, Twitter, and other social platforms that serve as today's biggest conduits for misinformation. After all, in the realm of modern media's history, these networks are tadpoles. "As an educator and as a scientist, I'm leaning towards, let's figure out a way to train people in school to not fall victim to false information, and how to judge what is likely to be false relative to what is likely to be true. And that's hard, but you and I have never had a class in that, have we? We've had biology classes, we've had English lit, we've had classes on Shakespeare — we have classes on 100 things and none of them are on the ability to distinguish what is true and what is not."
This is why Tyson himself doesn't engage in Trump bashing on his social feeds, but does try to get people to differentiate factual science from fake news. "I feel responsibility to participate in the enlightenment of culture and of civilization, because I have that access," says Tyson, who has 13.9M followers on Twitter, 1.2M on Instagram, and 4.2M on Facebook. He doesn't tell his followers not to inject themselves with Clorox ("no one likes being told what to do"), but tries to get them to visualize a pandemic's impact by comparing it to, say, a throng of rabbits.
"Left unchecked, 1,000 rabbits in 5 years, become 7-billion, the human population of the World. After 15 years, a 'land-ocean' of rabbits fills to one-kilometer depth across all of Earth's continents. Viruses can reproduce waaaay faster than Rabbits," he tweeted on April 6, after much of the nation had locked down to slow the pandemic's spread. For added viral impact, he attached a photo of an adorable, perhaps appropriately scared-looking, white bunny.
Of course, not all celebrities message responsibly.
Tyson is a rare scientist-turned-celebrity. His appeal isn't acting in movies or singing dance-pop anthems (if only). Rather, his life's work is making science fun and interesting to as many people as possible through his best-selling books on astrophysics and his directorship of the planetarium at the American Museum of Natural History in New York. His longstanding place in popular culture is an exception, not the rule.
And he believes his fellow celebrities, actors and pop music stars and internet influencers, should aid the public's quest for accurate scientific information. And in order to do that, they must point their followers to experts and organizations who know what they're talking about. "It could be to a website, it could be to a talk that was given. I would say that that's where the responsibility lies if you control the interests of a million people," he says.
One example of this is Lady Gaga's March 14 Instagram of herself on her couch with her three dogs with the caption, "So I talked to some doctors and scientists. It's not the easiest for everyone right now but the kindest/healthiest thing we can do is self-quarantine and not hang out with people over 65 and in large groups. I wish I could see my parents and grandmas right now but it's much safer to not so I don't get them sick in case I have it. I'm hanging at home with my dogs." (All the celebrities here in this article are my references, not Tyson's, who does not call out specific people.)
Of course, not all celebrities message responsibly. Jessica Biel and Jenny McCarthy have faced scorn for public stances against vaccines. Gwyneth Paltrow and her media brand GOOP have faced backlash for promoting homeopathic treatments with no basis in science.
"The New Age Movement is a cultural idea, it has nothing to do with religion, has nothing to do with politics, and it's people who were rejecting objectively established science in part or in total because they have a belief system that they want to attach to it, okay? This is how you get the homeopathic remedies," says Tyson. "That's why science exists, so that we don't have to base decisions on belief systems."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
Masks and Distancing Won't Be Enough to Prevent School Outbreaks, Latest Science Suggests
The likely dominant mode of aerosol transmission cannot be ignored in school settings.
Never has the prospect of "back to school" seemed so ominous as it does in 2020. As the number of COVID-19 cases climb steadily in nearly every state, the prospect of in-person classes are filling students, parents, and faculty alike with a corresponding sense of dread.
The notion that children are immune or resistant to SARS-CoV-2 is demonstrably untrue.
The decision to resume classes at primary, secondary, and collegiate levels is not one that should be regarded lightly, particularly as coronavirus cases skyrocket across the United States.
What should be a measured, data-driven discussion that weighs risks and benefits has been derailed by political talking points. President Trump has been steadily advocating for an unfettered return to the classroom, often through imperative "OPEN THE SCHOOLS!!!" tweets. In July, Secretary of Education Betsy DeVos threatened to withhold funding from schools that did not reopen for full-time, in-person classes, despite not having the authority to do so. Like so many public health issues, opening schools in the midst of a generational pandemic has been politicized to the point that the question of whether it is safe to do so has been obscured and confounded. However, this question still deserves to be examined based on evidence.
What We Know About Kids and COVID-19
Some arguments for returning to in-person education have focused on the fact that children and young adults are less susceptible to severe disease. In some cases, people have stated that children cannot be infected, pointing to countries that have resumed in-person education with no associated outbreaks. However, those countries had extremely low community transmission and robust testing and surveillance.
The notion that children are immune or resistant to SARS-CoV-2 is demonstrably untrue: children can be infected, they can become sick, and, in rare cases, they can die. Children can also transmit the virus to others, especially if they are in prolonged proximity to them. A Georgia sleepaway camp was the site of at least 260 cases among mostly children and teenagers, some as young as 6 years old. Children have been shown to shed infectious virus in their nasal secretions and have viral loads comparable to adults. Children can unquestionably be infected with SARS-CoV-2 and spread it to others.
The more data emerges, the more it appears that both primary and secondary schools and universities alike are conducive environments for super-spreading. Mitigating these risks depends heavily on individual schools' ability to enforce reduction measures. So far, the evidence demonstrates that in most cases, schools are unable to adequately protect students or staff. A school superintendent from a small district in Arizona recently described an outbreak that occurred among staff prior to in-person classes resuming. Schools that have opened so far have almost immediately reported new clusters of cases among students or staff.
This is because it is impossible to completely eliminate risk even with the most thoughtful mitigation measures when community transmission is high. Risk can be reduced, but the greater the likelihood that someone will be exposed in the community, the greater the risk they might pass the virus to others on campus or in the classroom.
There are still many unknowns about SARS-CoV-2 transmission, but some environments are known risks for virus transmission: enclosed spaces with crowds of people in close proximity over extended durations. Transmission is thought to occur predominantly through inhaled aerosols or droplets containing SARS-CoV-2, which are produced through common school activities such as breathing, speaking, or singing. Masks reduce but do not eliminate the production of these aerosols. Implementing universal mask-wearing and physical distancing guidelines will furthermore be extraordinarily challenging for very young children.
Smaller particle aerosols can remain suspended in the air and accumulate over time. In an enclosed space where people are gathering, such as a classroom, this renders risk mitigation measures such as physical distancing and masks ineffective. Many classrooms at all levels of education are not conducive to improving ventilation through low-cost measures such as opening windows, much less installing costly air filtration systems.
As a risk reduction measure, ventilation greatly depends on factors like window placement, window type, room size, room occupancy, building HVAC systems, and overall airflow. There isn't much hard data on the specific effects of ventilation on virus transmission, and the models that support ventilation rely on assumptions based on scant experimental evidence that doesn't account for virologic parameters.
There is also no data about how effective air filtration or UV systems would be for SARS-CoV-2 transmission risk reduction, so it's hard to say if this would result in a meaningful risk reduction or not. We don't have enough data outside of a hospital setting to support that ventilation and/or filtration would significantly reduce risk, and it's impractical (and most likely impossible in most schools) to implement hospital ventilation systems, which would likely require massive remodeling of existing HVAC infrastructure. In a close contact situation, the risk reduction might be minimal anyway since it's difficult to avoid exposure to respiratory aerosols and droplets a person is exhaling.
You'd need to get very low rates in the local community to open safely in person regardless of other risk reduction measures, and this would need to be complemented by robust testing and contact tracing capacity.
Efforts to resume in-person education depend heavily on school health and safety plans, which often rely on self-reporting of symptoms due to insufficient testing capacity. Self-reporting is notoriously unreliable, and furthermore, SARS-CoV-2 can be readily transmitted by pre-symptomatic individuals who may be unaware that they are sick, making testing an essential component of any such plan. Primary and secondary schools are faced with limited access to testing and no funds to support it. Even in institutions that include a testing component in their reopening plans, this is still too infrequent to support the full student body returning to campus.
Economic Conflicts of Interest
Rebecca Harrison, a PhD candidate at Cornell University serving on the campus reopening committee, is concerned that her institution's plan places too much faith in testing capacity and is over-reliant on untested models. Harrison says that, as a result, students are being implicitly encouraged to return to campus and "very little has been done to actively encourage students who are safe and able to stay home, to actually stay home."
Harrison also is concerned that her institution "presumably hopes to draw students back from the safety of their parents' basements to (re)join the residential campus experience ... and drive revenue." This is a legitimate concern. Some schools may be actively thwarting safety plans in place to protect students based on financial incentives. Student athletes at Colorado State have alleged that football coaches told them not to report COVID-19 symptoms and are manipulating contact tracing reports.
Public primary and secondary schools are not dependent on student athletics for revenue, but nonetheless are susceptible to state and federal policies that tie reopening to budgets. If schools are forced to make decisions based on a balance sheet, rather than the health and safety of students, teachers, and staff, they will implement health and safety plans that are inadequate. Schools will become ground zero for new clusters of cases.
Looking Ahead: When Will Schools Be Able to Open Again?
One crucial measure is the percent positivity rate in the local community, the number of positive tests based on all the tests that are done. Some states, like California, have implemented policies guiding the reopening of schools that depend in part on a local community's percent positivity rate falling under 8 percent, among other benchmarks including the rate of new daily cases. Currently, statewide, test positivity is below 7%, with an average of 3 new daily cases per 1000 people per day. However, the California department of health acknowledges that new cases per day are underreported. There are 6.3 million students in the California public school system, suggesting that at any given time, there could be nearly 20,000 students who might be contagious, without accounting for presymptomatic teachers and staff. In the classroom environment, just one of those positive cases could spread the virus to many people in one day despite masks, distancing, and ventilation.
You'd need to get very low rates in the local community to open safely in person regardless of other risk reduction measures, and this would need to be complemented by robust testing and contact tracing capacity. Only with rapid identification and isolation of new cases, followed by contact tracing and quarantine, can we break chains of transmission and prevent further spread in the school and the larger community.
None of these safety concerns diminish the many harms associated with the sudden and haphazard way remote learning has been implemented. Online education has not been effective in many cases and is difficult to implement equitably. Young children, in particular, are deprived of the essential social and intellectual development they would normally get in a classroom with teachers and their peers. Parents of young children are equally unprepared and unable to provide full-time instruction. Our federal leadership's catastrophic failure to contain the pandemic like other countries has put us in this terrible position, where we must choose between learning or spreading a deadly pathogen.
Blame aside, parents, educators, and administrators must decide whether to resume in-person classes this fall. Those decisions should be based on evidence, not on politics or economics. The data clearly shows that community transmission is out of control throughout most of the country. Thus, we ignore the risk of school outbreaks at our peril.
[Editor's Note: Here's the other essay in the Back to School series: 5 Key Questions to Consider Before Sending Your Child Back to School.]