Why Don’t We Have Artificial Wombs for Premature Infants?
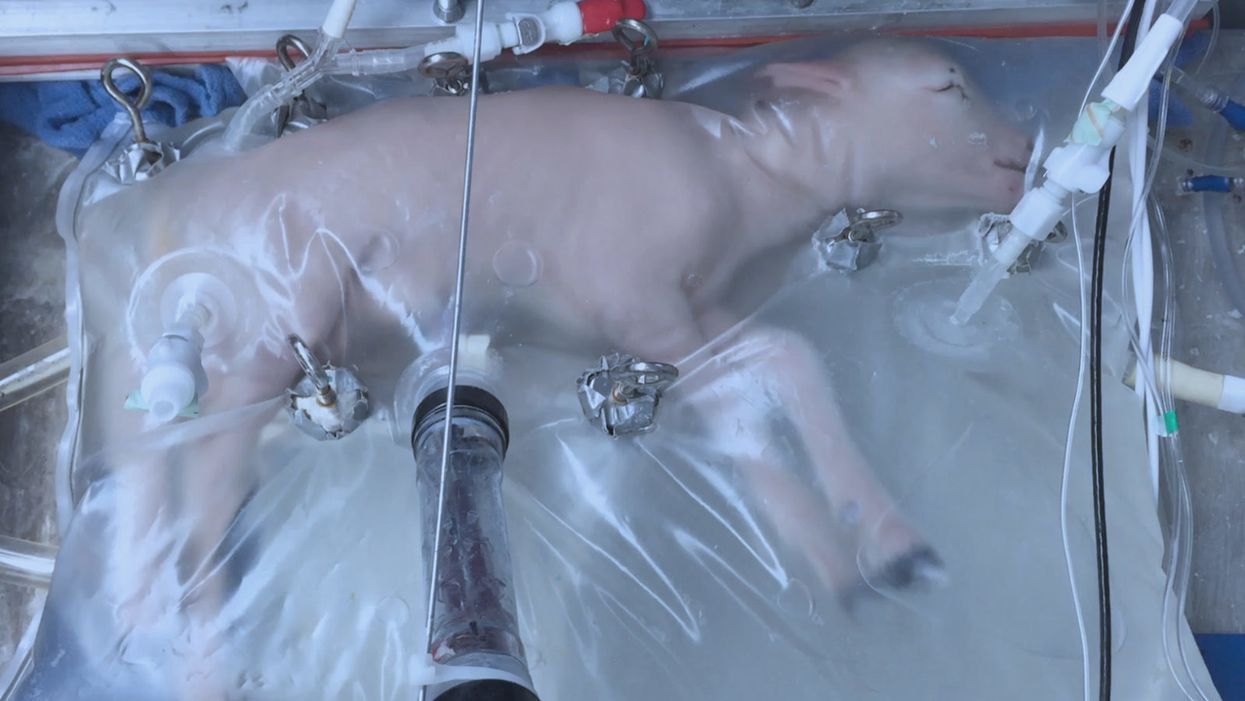
A lamb which was prematurely born at the equivalent of 23 weeks' human gestation, after 28 days of support from an artificial womb.
Ectogenesis, the development of a baby outside of the mother's body, is a concept that dates back to 1923. That year, British biochemist-geneticist J.B.S. Haldane gave a lecture to the "Heretics Society" of the University of Cambridge in which he predicted the invention of an artificial womb by 1960, leading to 70 percent of newborns being born that way by the 2070s. In reality, that's about when an artificial womb could be clinically operational, but trends in science and medicine suggest that such technology would come in increments, each fraught with ethical and social challenges.
An extra-uterine support device could be ready for clinical trials in humans in the next two to four years, with hopes that it could improve survival of very premature infants.
Currently, one major step is in the works, a system called an extra-uterine support device (EUSD) –or sometimes Ex-Vivo uterine Environment (EVE)– which researchers at the Children's Hospital of Philadelphia have been using to support fetal lambs outside the mother. It also has been called an artificial placenta, because it supplies nutrient- and oxygen-rich blood to the developing lambs via the umbilical vein and receives blood full of waste products through the umbilical arteries. It does not do everything that a natural placenta does, yet it does do some things that a placenta doesn't do. It breathes for the fetus like the mother's lungs, and encloses the fetus in sterile fluid, just like the amniotic sac. It represents a solution to one set of technical challenges in the path to an artificial womb, namely how to keep oxygen flowing into a fetus and carbon dioxide flowing out when the fetal lungs are not ready to function.
Capable of supporting fetal lambs physiologically equivalent to a human fetus at 23 weeks' gestation or earlier, the EUSD could be ready for clinical trials in humans in the next two to four years, with hopes that it could improve survival of very premature infants. Existing medical technology can keep human infants alive when born in this 23-week range, or even slightly less —the record is just below 22 weeks. But survival is low, because most of the treatment is directed at the lungs, the last major body system to mature to a functional status. This leads to complications not only in babies born before 24 weeks' gestation, but also in a fairly large number of births up to 28 weeks' gestation.
So, the EUSD is basically an advanced neonatal life support machine that beckons to square off the survival curve for infants born up to the 28th week. That is no doubt a good thing, but given the political prominence of reproductive issues, might any societal obstacles be looming?
"While some may argue that the EUSD system will shift the definition of viability to a point prior to the maturation of the fetus' lungs, ethical and legal frameworks must still recognize the mother's privacy rights as paramount."
Health care attorney and clinical ethicist David N. Hoffman points out that even though the EUSD may shift the concept of fetal viability away from the maturity of developing lungs, it would not change the current relationship of the fetus to the mother during pregnancy.
"Our social and legal frameworks, including Roe v. Wade, invite the view of the embryo-fetus as resembling a parasite. Not in a negative sense, but functionally, since it obtains its life support from the mother, while she does not need the fetus for her own physical health," notes Hoffman, who holds faculty appointments at Columbia University, and at the Benjamin N. Cardozo School of Law and the Albert Einstein College of Medicine, of Yeshiva University. "In contrast, our ethical conception of the relationship is grounded in the nurturing responsibility of parenthood. We prioritize the welfare of both mother and fetus ethically, but we lean toward the side of the mother's legal rights, regarding her health throughout pregnancy, and her right to control her womb for most of pregnancy. While some may argue that the EUSD system will shift the definition of viability to a point prior to the maturation of the fetus' lungs, ethical and legal frameworks must still recognize the mother's privacy rights as paramount, on the basis of traditional notions of personhood and parenthood."
Outside of legal frameworks, religion, of course, is a major factor in how society reacts to new reproductive technologies, and an artificial womb would trigger a spectrum of responses.
"Significant numbers of conservative Christians may oppose an artificial womb in fear that it might harm the central role of marriage in Christianity."
Speaking from the perspective of Lutheran scholarship, Dr. Daniel Deen, Assistant Professor of Philosophy at Concordia University in Irvine, Calif., does not foresee any objections to the EUSD, either theologically, or generally from Lutherans (who tend to be conservative on reproductive issues), since the EUSD is basically an improvement on current management of prematurity. But things would change with the advent of a full-blown artificial womb.
"Significant numbers of conservative Christians may oppose an artificial womb in fear that it might harm the central role of marriage in Christianity," says Deen, who specializes in the philosophy of science. "They may see the artificial womb as a catalyst for strengthening the mechanistic view of reproduction that dominates the thinking of secular society, and of other religious groups, including more liberal Christians."
Judaism, however, appears to be more receptive, even during the research phases.
"Even if researchers strive for a next-generation EUSD aimed at supporting a fetus several weeks earlier than possible with the current system, it still keeps the fetus inside the mother well beyond the 40-day threshold, so there likely are no concerns in terms of Jewish law," says Kalman Laufer, a rabbinical student and executive director of the Medical Ethics Society at Yeshiva University. Referring to a concept from the Babylonian Talmud that an embryo is "like water" until 40 days into pregnancy, at which time it receives a kind of almost-human status warranting protection, Laufer cautions that he's speaking about artificial wombs developed for the sake of rescuing very premature infants. At the same time though, he expects that artificial womb research will eventually trigger a series of complex, legalistic opinions from Jewish scholars, as biotechnology moves further toward supporting fetal growth entirely outside a woman's body.
"Since [the EUSD] gives some justification to end abortion, by transferring fetuses from mother to machine, conservatives will probably rally around it."
While the technology treads into uncomfortable territory for social conservatives at first glance, it's possible that the prospect of taking the abortion debate in a whole new direction could engender support for the artificial womb. "Since [the EUSD] gives some justification to end abortion, by transferring fetuses from mother to machine, conservatives will probably rally around it," says Zoltan Istvan, a transhumanist politician and journalist who ran for U.S. president in 2016. To some extent, Deen agrees with Istvan, provided we get to a point when the artificial womb is already a reality.
"The world has a way of moving forward despite the fear of its inhabitants," Deen notes. "If the technology gets developed, I could not see any Christians, liberal or conservative, arguing that people seeking abortion ought not opt for a 'transfer' versus an abortive procedure."
So then how realistic is a full-blown artificial womb? The researchers at the Children's Hospital of Philadelphia have noted various technical difficulties that would come up in any attempt to connect a very young fetus to the EUSD and maintain life. One issue is the small umbilical cord blood vessels that must be connected to the EUSD as fetuses of decreasing gestational age are moved outside the mother. Current procedures might be barely adequate for integrating a human fetus into the device in the 18 -21 week range, but going to lower gestational ages would require new technology and different strategies. It also would require numerous other factors to cover for fetal body systems that mature ahead of the lungs and that the current EUSD system is not designed to replace. However, biotechnology and tissue engineering strategies on the horizon could be added to later EUSDs. To address the blood vessel size issue, artificial womb research could benefit by drawing on experts in microfluidics, the field concerned with manipulation of tiny amounts of fluid through very small spaces, and which is ushering in biotech innovations like the "lab on a chip".
"The artificial womb might put fathers on equal footing with mothers, since any embryo could potentially achieve personhood without ever seeing the inside of a woman's uterus."
If the technical challenges to an artificial womb are indeed overcome, reproductive policy debates could be turned on their side.
"Evolution of the EUSD into a full-blown artificial external uterus has ramifications for any reproductive rights issues where policy currently assumes that a mother is needed for a fertilized egg to become a person," says Hoffman, the ethicist and legal scholar. "If we consider debates over whether to keep cryopreserved human embryos in storage, destroy them, or utilize them for embryonic stem cell research or therapies, the artificial womb might put fathers on equal footing with mothers, since any embryo could potentially achieve personhood without ever seeing the inside of a woman's uterus."
Such a scenario, of course, depends on today's developments not being curtailed or sidetracked by societal objections before full-blown ectogenesis is feasible. But if this does ever become a reality, the history of other biotechnologies suggests that some segment of society will embrace the new innovation and never look back.
Chris Mirabile sprints on a track in Sarasota, Florida, during his daily morning workout. He claims to be a superager already, at age 38, with test results to back it up.
Earlier this year, Harvard scientists reported that they used an anti-aging therapy to reverse blindness in elderly mice. Several other studies in the past decade have suggested that the aging process can be modified, at least in lab organisms. Considering mice and humans share virtually the same genetic makeup, what does the rodent-based study mean for the humans?
In truth, we don’t know. Maybe nothing.
What we do know, however, is that a growing number of people are dedicating themselves to defying the aging process, to turning back the clock – the biological clock, that is. Take Bryan Johnson, a man who is less mouse than human guinea pig. A very wealthy guinea pig.
The 45-year-old venture capitalist spends over $2 million per year reversing his biological clock. To do this, he employs a team of 30 medical doctors and other scientists. His goal is to eventually reset his biological clock to age 18, and “have all of his major organs — including his brain, liver, kidneys, teeth, skin, hair, penis and rectum — functioning as they were in his late teens,” according to a story earlier this year in the New York Post.
But his daily routine paints a picture that is far from appealing: for example, rigorously adhering to a sleep schedule of 8 p.m. to 5 a.m. and consuming more than 100 pills and precisely 1,977 calories daily. Considering all of Johnson’s sacrifices, one discovers a paradox:
To live forever, he must die a little every day until he reaches his goal - if he ever reaches his goal.
Less extreme examples seem more helpful for people interested in happy, healthy aging. Enter Chris Mirabile, a New Yorker who says on his website, SlowMyAge.com, that he successfully reversed his biological age by 13.6 years, from the chronological age of 37.2 to a biological age of 23.6. To put this achievement in perspective, Johnson, to date, has reversed his biological clock by 2.5 years.
Mirabile's habits and overall quest to turn back the clock trace back to a harrowing experience at age 16 during a school trip to Manhattan, when he woke up on the floor with his shirt soaked in blood.
Mirabile, who is now 38, supports his claim with blood tests that purport to measure biological age by assessing changes to a person’s epigenome, or the chemical marks that affect how genes are expressed. Mirabile’s tests have been run and verified independently by the same scientific lab that analyzes Johnson’s. (In an email to Leaps.org, the lab, TruDiagnostic, confirmed Mirabile’s claims about his test results.)
There is considerable uncertainty among scientists about the extent to which these tests can accurately measure biological age in individuals. Even so, Mirabile’s results are intriguing. They could reflect his smart lifestyle for healthy aging.
His habits and overall quest to turn back the clock trace back to a harrowing experience at age 16 during a school trip to Manhattan, when Mirabile woke up on the floor with his shirt soaked in blood. He’d severed his tongue after a seizure. He later learned it was caused by a tumor the size of a golf ball. As a result, “I found myself contemplating my life, what I had yet to experience, and mortality – a theme that stuck with me during my year of recovery and beyond,” Mirabile told me.
For the next 15 years, he researched health and biology, integrating his learnings into his lifestyle. Then, in his early 30s, he came across an article in the journal Cell, "The Hallmarks of Aging," that outlined nine mechanisms of the body that define the aging process. Although the paper says there are no known interventions to delay some of these mechanisms, others, such as inflammation, struck Mirabile as actionable. Reading the paper was his “moment of epiphany” when it came to the areas where he could assert control to maximize his longevity.
He also wanted “to create a resource that my family, friends, and community could benefit from in the short term,” he said. He turned this knowledge base into a company called NOVOS dedicated to extending lifespan.
His longevity advice is more accessible than Johnson’s multi-million dollar approach, as Mirabile spends a fraction of that amount. Mirabile takes one epigenetic test per year and has a gym membership at $45 per month. Unlike Johnson, who takes 100 pills per day, Mirabile takes 10, costing another $45 monthly, including a B-complex, fish oil, Vitamins D3 and K2, and two different multivitamin supplements.
Mirabile’s methods may be easier to apply in other ways as well, since they include activities that many people enjoy anyway. He’s passionate about outdoor activities, travels frequently, and has loving relationships with friends and family, including his girlfriend and collie.
Here are a few of daily routines that could, he thinks, contribute to his impressively young bio age:
After waking at 7:45 am, he immediately drinks 16 ounces of water, with 1/4 teaspoon of sodium and potassium to replenish electrolytes. He takes his morning vitamins, brushes and flosses his teeth, puts on a facial moisturizing sunblock and goes for a brisk, two-mile walk in the sun. At 8:30 am on Mondays, Wednesdays, and Fridays he lift weights, focusing on strength and power, especially in large muscle groups.
Tuesdays, Thursdays and Saturdays are intense cardio days. He runs 5-7 miles or bicycles for 60 minutes first thing in the morning at a brisk pace, listening to podcasts. Sunday morning cardio is more leisurely.
After working out each day, he’s back home at 9:20 am, where he makes black coffee, showers, then applies serum and moisturizing sunblock to his face. He works for about three hours on his laptop, then has a protein shake and fruit.
Mirabile is a dedicated intermittent faster, with a six hour eating window in between 18 hours fasts. At 3 pm, he has lunch. The Mediterranean lineup often features salmon, sardines, olive oil, pink Himalayan salt plus potassium salt for balance, and lots of dried herbs and spices. He almost always finishes with 1/3 to 1/2 bar of dark chocolate.
If you are what you eat, Mirabile is made of mostly plants and lean meats. He follows a Mediterranean diet full of vegetables, fruits, fatty fish and other meats full of protein and unsaturated fats. “These may cost more than a meal at an American fast-food joint, but then again, not by much,” he said. Each day, he spends $25 on all his meals combined.
At 6 pm, he takes the dog out for a two-mile walk, taking calls for work or from family members along the way. At 7 pm, he dines with his girlfriend. Like lunch, this meal is heavy on widely available ingredients, including fish, fresh garlic, and fermented food like kimchi. Mirabile finishes this meal with sweets, like coconut milk yogurt with cinnamon and clove, some stevia, a mix of fresh berries and cacao nibs.
If Mirabile's epigenetic tests are accurate, his young biological age could be thanks to his healthy lifestyle, or it could come from a stroke of luck if he inherited genes that protect against aging.
At 8 pm, he wraps up work duties and watches shows with his girlfriend, applies serum and moisturizer yet again, and then meditates with the lights off. This wind-down, he said, improves his sleep quality. Wearing a sleep mask and earplugs, he’s asleep by about 10:30.
“I’ve achieved stellar health outcomes, even after having had the physiological stressors of a brain tumor, without spending a fortune,” Mirabile said. “In fact, even during times when I wasn’t making much money as a startup founder with few savings, I still managed to live a very healthy, pro-longevity lifestyle on a modest budget.”
Mirabile said living a cleaner, healthier existence is a reality that many readers can achieve. It’s certainly true that many people live in food deserts and have limited time for exercise or no access to gyms, but James R. Doty, a clinical professor of neurosurgery at Stanford, thinks many can take more action to stack the odds that they’ll “be happy and live longer.” Many of his recommendations echo aspects of Mirabile’s lifestyle.
Each night, Doty said, it’s vital to get anywhere between 6-8 hours of good quality sleep. Those who sleep less than 6 hours per night are at an increased risk of developing a whole host of medical problems, including high blood pressure, type 2 diabetes, and stroke.
In addition, it’s critical to follow Mirabile’s prescription of exercise for about one hour each day, and intensity levels matter. Doty noted that, in 2017, researchers at Brigham Young University found that people who ran at a fast pace for 30-40 minutes five days per week were, on average, biologically younger by nine years, compared to those who subscribed to more moderate exercise programs, as well as those who rarely exercised.
When it comes to nutrition, one should consider fasting for 16 hours per day, Doty said. This is known as the 16/8 method, where one’s daily calories are consumed within an eight hour window, fasting for the remaining 16 hours, just like Mirabile. Intermittent fasting is associated with cellular repair and less inflammation, though it’s not for everyone, Doty added. Consult with a medical professional before trying a fasting regimen.
Finally, Doty advised to “avoid anger, avoid stress.” Easier said than done, but not impossible. “Between stimulus and response, there is a pause and within that pause lies your freedom,” Doty said. Mirabile’s daily meditation ritual could be key to lower stress for healthy aging. Research has linked regular, long-term meditation to having a lower epigenetic age, compared to control groups.
Many other factors could apply. Having a life purpose, as Mirabile does with his company, has also been associated with healthy aging and lower epigenetic age. Of course, Mirabile is just one person, so it’s hard to know how his experience will apply to others. If his tests are accurate, his young biological age could be thanks to his healthy lifestyle, or it could come from a stroke of luck if he inherited genes that protect against aging. Clearly, though, any such genes did not protect him from cancer at an early age.
The third and perhaps most likely explanation: Mirabile’s very young biological age results from a combination of these factors. Some research shows that genetics account for only 25 percent of longevity. That means environmental factors could be driving the other 75 percent, such as where you live, frequency of exercise, quality of nutrition and social support.
The middle-aged – even Brian Johnson – probably can’t ever be 18 again. But more modest goals are reasonable for many. Control what you can for a longer, healthier life.
FDA, researchers work to make clinical trials more diverse
The U.S. population is becoming more diverse, but clinical trials don't reflect that, experts say. Some are focusing on recruiting minorities to participate in research.
Nestled in a predominately Hispanic neighborhood, a new mural outside Guadalupe Centers Middle School in Kansas City, Missouri imparts a powerful message: “Clinical Research Needs Representation.” The colorful portraits painted above those words feature four cancer survivors of different racial and ethnic backgrounds. Two individuals identify as Hispanic, one as African American and another as Native American.
One of the patients depicted in the mural is Kim Jones, a 51-year-old African American breast cancer survivor since 2012. She advocated for an African American friend who participated in several clinical trials for ovarian cancer. Her friend was diagnosed in an advanced stage at age 26 but lived nine more years, thanks to the trials testing new therapeutics. “They are definitely giving people a longer, extended life and a better quality of life,” said Jones, who owns a nail salon. And that’s the message the mural aims to send to the community: Clinical trials need diverse participants.
While racial and ethnic minority groups represent almost half of the U.S. population, the lack of diversity in clinical trials poses serious challenges. Limited awareness and access impede equitable representation, which is necessary to prove the safety and effectiveness of medical interventions across different groups.
A Yale University study on clinical trial diversity published last year in BMJ Medicine found that while 81 percent of trials testing the new cancer drugs approved by the U.S. Food and Drug Administration between 2012 and 2017 included women, only 23 percent included older adults and 5 percent fairly included racial and ethnic minorities. “It’s both a public health and social justice issue,” said Jennifer E. Miller, an associate professor of medicine at Yale School of Medicine. “We need to know how medicines and vaccines work for all clinically distinct groups, not just healthy young White males.” A recent JAMA Oncology editorial stresses out the need for legislation that would require diversity action plans for certain types of trials.
Ensuring meaningful representation of racial and ethnic minorities in clinical trials for regulated medical products is fundamental to public health.--FDA Commissioner Robert M. Califf.
But change is on the horizon. Last April, the FDA issued a new draft guidance encouraging industry to find ways to revamp recruitment into clinical trials. The announcement, which expanded on previous efforts, called for including more participants from underrepresented racial and ethnic segments of the population.
“The U.S. population has become increasingly diverse, and ensuring meaningful representation of racial and ethnic minorities in clinical trials for regulated medical products is fundamental to public health,” FDA commissioner Robert M. Califf, a physician, said in a statement. “Going forward, achieving greater diversity will be a key focus throughout the FDA to facilitate the development of better treatments and better ways to fight diseases that often disproportionately impact diverse communities. This guidance also further demonstrates how we support the Administration’s Cancer Moonshot goal of addressing inequities in cancer care, helping to ensure that every community in America has access to cutting-edge cancer diagnostics, therapeutics and clinical trials.”
Lola Fashoyin-Aje, associate director for Science and Policy to Address Disparities in the Oncology Center of Excellence at the FDA, said that the agency “has long held the view that clinical trial participants should reflect the clinical and demographic characteristics of the patients who will ultimately receive the drug once approved.” However, “numerous studies over many decades” have measured the extent of underrepresentation. One FDA analysis found that the proportion of White patients enrolled in U.S. clinical trials (88 percent) is much higher than their numbers in country's population. Meanwhile, the enrollment of African American and Native Hawaiian/American Indian and Alaskan Native patients is below their national numbers.
The FDA’s guidance is accelerating researchers’ efforts to be more inclusive of diverse groups in clinical trials, said Joyce Sackey, a clinical professor of medicine and associate dean at Stanford School of Medicine. Underrepresentation is “a huge issue,” she noted. Sackey is focusing on this in her role as the inaugural chief equity, diversity and inclusion officer at Stanford Medicine, which encompasses the medical school and two hospitals.
Until the early 1990s, Sackey pointed out, clinical trials were based on research that mainly included men, as investigators were concerned that women could become pregnant, which would affect the results. This has led to some unfortunate consequences, such as indications and dosages for drugs that cause more side effects in women due to biological differences. “We’ve made some progress in including women, but we have a long way to go in including people of different ethnic and racial groups,” she said.

A new mural outside Guadalupe Centers Middle School in Kansas City, Missouri, advocates for increasing diversity in clinical trials. Kim Jones, 51-year-old African American breast cancer survivor, is second on the left.
Artwork by Vania Soto. Photo by Megan Peters.
Among racial and ethnic minorities, distrust of clinical trials is deeply rooted in a history of medical racism. A prime example is the Tuskegee Study, a syphilis research experiment that started in 1932 and spanned 40 years, involving hundreds of Black men with low incomes without their informed consent. They were lured with inducements of free meals, health care and burial stipends to participate in the study undertaken by the U.S. Public Health Service and the Tuskegee Institute in Alabama.
By 1947, scientists had figured out that they could provide penicillin to help patients with syphilis, but leaders of the Tuskegee research failed to offer penicillin to their participants throughout the rest of the study, which lasted until 1972.
Opeyemi Olabisi, an assistant professor of medicine at Duke University Medical Center, aims to increase the participation of African Americans in clinical research. As a nephrologist and researcher, he is the principal investigator of a clinical trial focusing on the high rate of kidney disease fueled by two genetic variants of the apolipoprotein L1 (APOL1) gene in people of recent African ancestry. Individuals of this background are four times more likely to develop kidney failure than European Americans, with these two variants accounting for much of the excess risk, Olabisi noted.
The trial is part of an initiative, CARE and JUSTICE for APOL1-Mediated Kidney Disease, through which Olabisi hopes to diversify study participants. “We seek ways to engage African Americans by meeting folks in the community, providing accessible information and addressing structural hindrances that prevent them from participating in clinical trials,” Olabisi said. The researchers go to churches and community organizations to enroll people who do not visit academic medical centers, which typically lead clinical trials. Since last fall, the initiative has screened more than 250 African Americans in North Carolina for the genetic variants, he said.
Other key efforts are underway. “Breaking down barriers, including addressing access, awareness, discrimination and racism, and workforce diversity, are pivotal to increasing clinical trial participation in racial and ethnic minority groups,” said Joshua J. Joseph, assistant professor of medicine at the Ohio State University Wexner Medical Center. Along with the university’s colleges of medicine and nursing, researchers at the medical center partnered with the African American Male Wellness Agency, Genentech and Pfizer to host webinars soliciting solutions from almost 450 community members, civic representatives, health care providers, government organizations and biotechnology professionals in 25 states and five countries.
Their findings, published in February in the journal PLOS One, suggested that including incentives or compensation as part of the research budget at the institutional level may help resolve some issues that hinder racial and ethnic minorities from participating in clinical trials. Compared to other groups, more Blacks and Hispanics have jobs in service, production and transportation, the authors note. It can be difficult to get paid leave in these sectors, so employees often can’t join clinical trials during regular business hours. If more leaders of trials offer money for participating, that could make a difference.
Obstacles include geographic access, language and other communications issues, limited awareness of research options, cost and lack of trust.
Christopher Corsico, senior vice president of development at GSK, formerly GlaxoSmithKline, said the pharmaceutical company conducted a 17-year retrospective study on U.S. clinical trial diversity. “We are using epidemiology and patients most impacted by a particular disease as the foundation for all our enrollment guidance, including study diversity plans,” Corsico said. “We are also sharing our results and ideas across the pharmaceutical industry.”
Judy Sewards, vice president and head of clinical trial experience at Pfizer’s headquarters in New York, said the company has committed to achieving racially and ethnically diverse participation at or above U.S. census or disease prevalence levels (as appropriate) in all trials. “Today, barriers to clinical trial participation persist,” Sewards said. She noted that these obstacles include geographic access, language and other communications issues, limited awareness of research options, cost and lack of trust. “Addressing these challenges takes a village. All stakeholders must come together and work collaboratively to increase diversity in clinical trials.”
It takes a village indeed. Hope Krebill, executive director of the Masonic Cancer Alliance, the outreach network of the University of Kansas Cancer Center in Kansas City, which commissioned the mural, understood that well. So her team actively worked with their metaphorical “village.” “We partnered with the community to understand their concerns, knowledge and attitudes toward clinical trials and research,” said Krebill. “With that information, we created a clinical trials video and a social media campaign, and finally, the mural to encourage people to consider clinical trials as an option for care.”
Besides its encouraging imagery, the mural will also be informational. It will include a QR code that viewers can scan to find relevant clinical trials in their location, said Vania Soto, a Mexican artist who completed the rendition in late February. “I’m so honored to paint people that are survivors and are living proof that clinical trials worked for them,” she said.
Jones, the cancer survivor depicted in the mural, hopes the image will prompt people to feel more open to partaking in clinical trials. “Hopefully, it will encourage people to inquire about what they can do — how they can participate,” she said.

