Eight Big Medical and Science Trends to Watch in 2021

Promising developments underway include advancements in gene and cell therapy, better testing for COVID, and a renewed focus on climate change.
The world as we know it has forever changed. With a greater focus on science and technology than before, experts in the biotech and life sciences spaces are grappling with what comes next as SARS-CoV-2, the coronavirus that causes the COVID-19 illness, has spread and mutated across the world.
Even with vaccines being distributed, so much still remains unknown.
Jared Auclair, Technical Supervisor for the Northeastern University's Life Science Testing Center in Burlington, Massachusetts, guides a COVID testing lab that cranks out thousands of coronavirus test results per day. His lab is also focused on monitoring the quality of new cell and gene therapy products coming to the market.
Here are trends Auclair and other experts are watching in 2021.
Better Diagnostic Testing for COVID
Expect improvements in COVID diagnostic testing and the ability to test at home.
There are currently three types of coronavirus tests. The molecular test—also known as the RT-PCR test, detects the virus's genetic material, and is highly accurate, but it can take days to receive results. There are also antibody tests, done through a blood draw, designed to test whether you've had COVID in the past. Finally, there's the quick antigen test that isn't as accurate as the PCR test, but can identify if people are going to infect others.
Last month, Lucira Health secured the U.S. FDA Emergency Use Authorization for the first prescription molecular diagnostic test for COVID-19 that can be performed at home. On December 15th, the Ellume Covid-19 Home Test received authorization as the first over-the-counter COVID-19 diagnostic antigen test that can be done at home without a prescription. The test uses a nasal swab that is connected to a smartphone app and returns results in 15-20 minutes. Similarly, the BinaxNOW COVID-19 Ag Card Home Test received authorization on Dec. 16 for its 15-minute antigen test that can be used within the first seven days of onset of COIVD-19 symptoms.
Home testing has the possibility to impact the pandemic pretty drastically, Auclair says, but there are other considerations: the type and timing of test that is administered, how expensive is the test (and if it is financially feasible for the general public) and the ability of a home test taker to accurately administer the test.
"The vaccine roll-out will not eliminate the need for testing until late 2021 or early 2022."
Ideally, everyone would frequently get tested, but that would mean the cost of a single home test—which is expected to be around $30 or more—would need to be much cheaper, more in the $5 range.
Auclair expects "innovations in the diagnostic space to explode" with the need for more accurate, inexpensive, quicker COVID tests. Auclair foresees innovations to be at first focused on COVID point-of-care testing, but he expects improvements within diagnostic testing for other types of viruses and diseases too.
"We still need more testing to get the pandemic under control, likely over the next 12 months," Auclair says. "The vaccine roll-out will not eliminate the need for testing until late 2021 or early 2022."
Rise of mRNA-based Vaccines and Therapies
A year ago, vaccines weren't being talked about like they are today.
"But clearly vaccines are the talk of the town," Auclair says. "The reason we got a vaccine so fast was there was so much money thrown at it."
A vaccine can take more than 10 years to fully develop, according to the World Economic Forum. Prior to the new COVID vaccines, which were remarkably developed and tested in under a year, the fastest vaccine ever made was for mumps -- and it took four years.
"Normally you have to produce a protein. This is typically done in eggs. It takes forever," says Catherine Dulac, a neuroscientist and developmental biologist at Harvard University who won the 2021 Breakthrough Prize in Life Sciences. "But an mRNA vaccine just enabled [us] to skip all sorts of steps [compared with burdensome conventional manufacturing] and go directly to a product that can be injected into people."
Non-traditional medicines based on genetic research are in their infancy. With mRNA-based vaccines hitting the market for the first time, look for more vaccines to be developed for whatever viruses we don't currently have vaccines for, like dengue virus and Ebola, Auclair says.
"There's a whole bunch of things that could be explored now that haven't been thought about in the past," Auclair says. "It could really be a game changer."
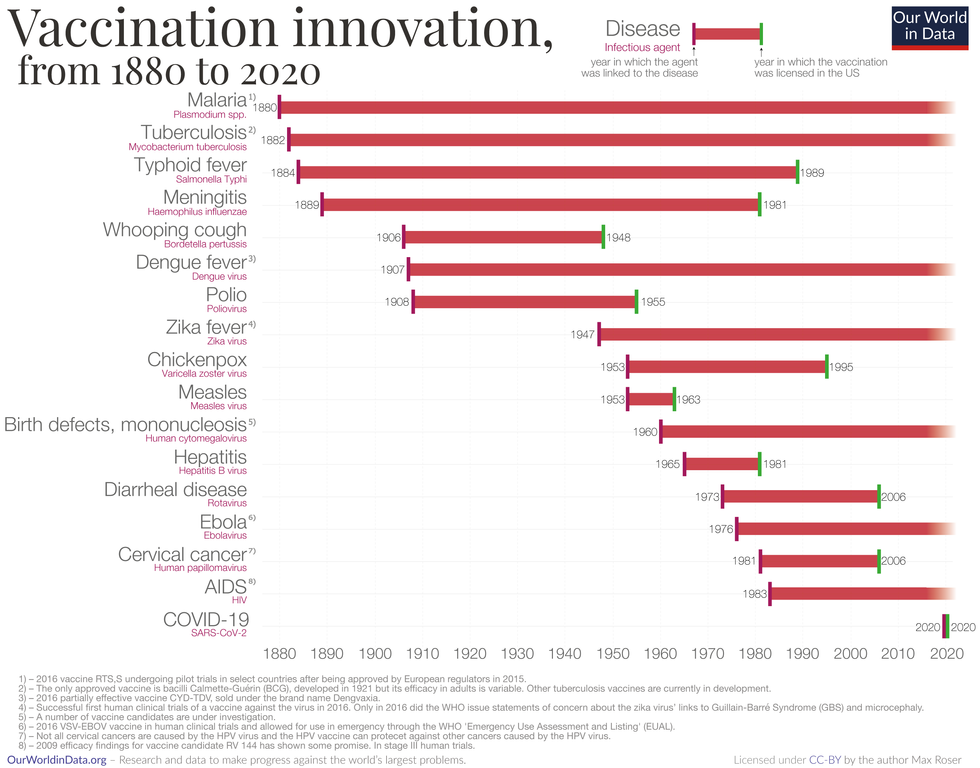
Vaccine Innovation over the last 140 years.
Max Roser/Our World in Data (Creative Commons license)
Advancements in Cell and Gene Therapies
CRISPR, a type of gene editing, is going to be huge in 2021, especially after the Nobel Prize in Chemistry was awarded to Emmanuelle Charpentier and Jennifer Doudna in October for pioneering the technology.
Right now, CRISPR isn't completely precise and can cause deletions or rearrangements of DNA.
"It's definitely not there yet, but over the next year it's going to get a lot closer and you're going to have a lot of momentum in this space," Auclair says. "CRISPR is one of the technologies I'm most excited about and 2021 is the year for it."
Gene therapies are typically used on rare genetic diseases. They work by replacing the faulty dysfunctional genes with corrected DNA codes.
"Cell and gene therapies are really where the field is going," Auclair says. "There is so much opportunity....For the first time in our life, in our existence as a species, we may actually be able to cure disease by using [techniques] like gene editing, where you cut in and out of pieces of DNA that caused a disease and put in healthy DNA," Auclair says.
For example, Spinal Muscular Atrophy is a rare genetic disorder that leads to muscle weakness, paralysis and death in children by age two. As of last year, afflicted children can take a gene therapy drug called Zolgensma that targets the missing or nonworking SMN1 gene with a new copy.
Another recent breakthrough uses gene editing for sickle cell disease. Victoria Gray, a mom from Mississippi who was exclusively followed by NPR, was the first person in the United States to be successfully treated for the genetic disorder with the help of CRISPR. She has continued to improve since her landmark treatment on July 2, 2019 and her once-debilitating pain has greatly eased.
"This is really a life-changer for me," she told NPR. "It's magnificent."
"You are going to see bigger leaps in gene therapies."
Look out also for improvements in cell therapies, but on a much lesser scale.
Cell therapies remove immune cells from a person or use cells from a donor. The cells are modified or cultured in lab, multiplied by the millions and then injected back into patients. These include stem cell therapies as well as CAR-T cell therapies, which are typically therapies of last resort and used in cancers like leukemia, Auclair says.
"You are going to see bigger leaps in gene therapies," Auclair says. "It's being heavily researched and we understand more about how to do gene therapies. Cell therapies will lie behind it a bit because they are so much more difficult to work with right now."
More Monoclonal Antibody Therapies
Look for more customized drugs to personalize medicine even more in the biotechnology space.
In 2019, the FDA anticipated receiving more than 200 Investigational New Drug (IND) applications in 2020. But with COVID, the number of INDs skyrocketed to 6,954 applications for the 2020 fiscal year, which ended September 30, 2020, according to the FDA's online tracker. Look for antibody therapies to play a bigger role.
Monoclonal antibodies are lab-grown proteins that mimic or enhance the immune system's response to fight off pathogens, like viruses, and they've been used to treat cancer. Now they are being used to treat patients with COVID-19.
President Donald Trump received a monoclonal antibody cocktail, called REGEN-COV2, which later received FDA emergency use authorization.
A newer type of monoclonal antibody therapy is Antibody-Drug Conjugates, also called ADCs. It's something we're going to be hearing a lot about in 2021, Auclair says.
"Antibody-Drug Conjugates is a monoclonal antibody with a chemical, we consider it a chemical warhead on it," Auclair says. "The monoclonal antibody binds to a specific antigen in your body or protein and delivers a chemical to that location and kills the infected cell."
Moving Beyond Male-Centric Lab Testing
Scientific testing for biology has, until recently, focused on testing males. Dulac, a Howard Hughes Medical Investigator and professor of molecular and cellular biology at Harvard University, challenged that idea to find brain circuitry behind sex-specific behaviors.
"For the longest time, until now, all the model systems in biology, are male," Dulac says. "The idea is if you do testing on males, you don't need to do testing on females."
Clinical models are done in male animals, as well as fundamental research. Because biological research is always done on male models, Dulac says the outcomes and understanding in biology is geared towards understanding male biology.
"All the drugs currently on the market and diagnoses of diseases are biased towards the understanding of male biology," Dulac says. "The diagnostics of diseases is way weaker in women than men."
That means the treatment isn't necessarily as good for women as men, she says, including what is known and understood about pain medication.
"So pain medication doesn't work well in women," Dulac says. "It works way better in men. It's true for almost all diseases that I know. Why? because you have a science that is dominated by males."
Although some in the scientific community challenge that females are not interesting or too complicated with their hormonal variations, Dulac says that's simply not true.
"There's absolutely no reason to decide 50% of life forms are interesting and the other 50% are not interesting. What about looking at both?" says Dulac, who was awarded the $3 million Breakthrough Prize in Life Sciences in September for connecting specific neural mechanisms to male and female parenting behaviors.
Disease Research on Single Cells
To better understand how diseases manifest in the body's cell and tissues, many researchers are looking at single-cell biology. Cells are the most fundamental building blocks of life. Much still needs to be learned.
"A remarkable development this year is the massive use of analysis of gene expression and chromosomal regulation at the single-cell level," Dulac says.
Much is focused on the Human Cell Atlas (HCA), a global initiative to map all cells in healthy humans and to better identify which genes associated with diseases are active in a person's body. Most estimates put the number of cells around 30 trillion.
Dulac points to work being conducted by the Cell Census Network (BICCN) Brain Initiative, an initiative by the National Institutes of Health to come up with an atlas of cell types in mouse, human and non-human primate brains, and the Chan Zuckerberg Initiative's funding of single-cell biology projects, including those focused on single-cell analysis of inflammation.
"Our body and our brain are made of a large number of cell types," Dulac says. "The ability to explore and identify differences in gene expression and regulation in massively multiplex ways by analyzing millions of cells is extraordinarily important."
Converting Plastics into Food
Yep, you heard it right, plastics may eventually be turned into food. The Defense Advanced Research Projects Agency, better known as DARPA, is funding a project—formally titled "Production of Macronutrients from Thermally Oxo-Degraded Wastes"—and asking researchers how to do this.
"When I first heard about this challenge, I thought it was absolutely absurd," says Dr. Robert Brown, director of the Bioeconomy Institute at Iowa State University and the project's principal investigator, who is working with other research partners at the University of Delaware, Sandia National Laboratories, and the American Institute of Chemical Engineering (AIChE)/RAPID Institute.
But then Brown realized plastics will slowly start oxidizing—taking in oxygen—and microorganisms can then consume it. The oxidation process at room temperature is extremely slow, however, which makes plastics essentially not biodegradable, Brown says.
That changes when heat is applied at brick pizza oven-like temperatures around 900-degrees Fahrenheit. The high temperatures get compounds to oxidize rapidly. Plastics are synthetic polymers made from petroleum—large molecules formed by linking many molecules together in a chain. Heated, these polymers will melt and crack into smaller molecules, causing them to vaporize in a process called devolatilization. Air is then used to cause oxidation in plastics and produce oxygenated compounds—fatty acids and alcohols—that microorganisms will eat and grow into single-cell proteins that can be used as an ingredient or substitute in protein-rich foods.
"The caveat is the microorganisms must be food-safe, something that we can consume," Brown says. "Like supplemental or nutritional yeast, like we use to brew beer and to make bread or is used in Australia to make Vegemite."
What do the microorganisms look like? For any home beer brewers, it's the "gunky looking stuff you'd find at the bottom after the fermentation process," Brown says. "That's cellular biomass. Like corn grown in the field, yeast or other microorganisms like bacteria can be harvested as macro-nutrients."
Brown says DARPA's ReSource program has challenged all the project researchers to find ways for microorganisms to consume any plastics found in the waste stream coming out of a military expeditionary force, including all the packaging of food and supplies. Then the researchers aim to remake the plastic waste into products soldiers can use, including food. The project is in the first of three phases.
"We are talking about polyethylene, polypropylene, like PET plastics used in water bottles and converting that into macronutrients that are food," says Brown.
Renewed Focus on Climate Change
The Union of Concerned Scientists say carbon dioxide levels are higher today than any point in at least 800,000 years.
"Climate science is so important for all of humankind. It is critical because the quality of life of humans on the planet depends on it."
Look for technology to help locate large-scale emitters of carbon dioxide, including sensors on satellites and artificial intelligence to optimize energy usage, especially in data centers.
Other technologies focus on alleviating the root cause of climate change: emissions of heat-trapping gasses that mainly come from burning fossil fuels.
Direct air carbon capture, an emerging effort to capture carbon dioxide directly from ambient air, could play a role.
The technology is in the early stages of development and still highly uncertain, says Peter Frumhoff, director of science and policy at Union of Concerned Scientists. "There are a lot of questions about how to do that at sufficiently low costs...and how to scale it up so you can get carbon dioxide stored in the right way," he says, and it can be very energy intensive.
One of the oldest solutions is planting new forests, or restoring old ones, which can help convert carbon dioxide into oxygen through photosynthesis. Hence the Trillion Trees Initiative launched by the World Economic Forum. Trees are only part of the solution, because planting trees isn't enough on its own, Frumhoff says. That's especially true, since 2020 was the year that human-made, artificial stuff now outweighs all life on earth.
More research is also going into artificial photosynthesis for solar fuels. The U.S. Department of Energy awarded $100 million in 2020 to two entities that are conducting research. Look also for improvements in battery storage capacity to help electric vehicles, as well as back-up power sources for solar and wind power, Frumhoff says.
Another method to combat climate change is solar geoengineering, also called solar radiation management, which reflects sunlight back to space. The idea stems from a volcanic eruption in 1991 that released a tremendous amount of sulfate aerosol particles into the stratosphere, reflecting the sunlight away from Earth. The planet cooled by a half degree for nearly a year, Frumhoff says. However, he acknowledges, "there's a lot of things we don't know about the potential impacts and risks" involved in this controversial approach.
Whatever the approach, scientific solutions to climate change are attracting renewed attention. Under President Trump, the White House Office of Science and Technology Policy didn't have an acting director for almost two years. Expect that to change when President-elect Joe Biden takes office.
"Climate science is so important for all of humankind," Dulac says. "It is critical because the quality of life of humans on the planet depends on it."
Time to visit your TikTok doc? The good and bad of doctors on social media
Rakhi Patel is among an increasing number of health care professionals, including doctors and nurses, who maintain an active persona on Instagram, TikTok and other social media sites.
Rakhi Patel has carved a hobby out of reviewing pizza — her favorite food — on Instagram. In a nod to her preferred topping, she calls herself thepepperoniqueen. Photos and videos show her savoring slices from scores of pizzerias. In some of them, she’s wearing scrubs — her attire as an inpatient neurology physician associate at Tufts Medical Center in Boston.
“Depending on how you dress your pizza, it can be more nutritious,” said Patel, who suggests a thin crust, sugarless tomato sauce and vegetables galore as healthier alternatives. “There are no boundaries for a health care professional to enjoy pizza.”
Beyond that, “pizza fuels my mental health and makes me happy, especially when loaded with pepperoni,” she said. “If I’m going to be a pizza connoisseur, then I also need to take care of my physical health by ensuring that I get at least three days of exercise per week and eat nutritiously when I’m not eating pizza.”
She’s among an increasing number of health care professionals, including doctors and nurses, who maintain an active persona on social media, according to bioethics researchers. They share their hobbies and interests with people inside and outside the world of medicine, helping patients and the public become acquainted with the humans behind the scrubs or white coats. Other health care experts limit their posts to medical topics, while some opt for a combination of personal and professional commentaries. Depending on the posts, ethical issues may come into play.
“Health care professionals are quite prevalent on social media,” said Mercer Gary, a postdoctoral researcher at The Hastings Center, an independent bioethics research institute in Garrison, New York. “They’ve been posting on #medTwitter for many years, mainly to communicate with one another, but, of course, anyone can see the threads. Most recently, doctors and nurses have become a presence on TikTok.”
On social media, many health care providers perceive themselves to be “humanizing” their profession by coming across as more approachable — “reminding patients that providers are people and workers, as well as repositories of medical expertise,” Gary said. As a result, she noted that patients who are often intimidated by clinicians may feel comfortable enough to overcome barriers to scheduling health care appointments. The use of TikTok in particular may help doctors and nurses connect with younger followers.
When health care providers post on social media, they must bear in mind that they have legal and ethical duties to their patients, profession and society, said Elizabeth Levy, founder and director of Physicians for Justice.
While enduring three years of pandemic conditions, many health care professionals have struggled with burnout, exhaustion and moral distress. “Much health care provider content on social media seeks to expose the difficulties of the work,” Gary added. “TikTok and Instagram reels have shown health care providers crying after losing a patient or exhausted after a night shift in the emergency department.”
A study conducted in Beijing, China and published last year found that TikTok is the world’s most rapidly growing video application, amassing 1.6 billion users in 2021. “More and more patients are searching for information on genitourinary cancers via TikTok,” the study’s authors wrote in Frontiers in Oncology, referring to cancers of the urinary tracts and male reproductive organs. Among the 61 sample videos examined by the researchers, health care practitioners contributed the content in 29, or 47 percent, of them. Yet, 22 posts, 36 percent, were misinformative, mostly due to outdated information.
More than half of the videos offered good content on disease symptoms and examinations. The authors concluded that “most videos on genitourinary cancers on TikTok are of poor to medium quality and reliability. However, videos posted by media agencies enjoyed great public attention and interaction. Medical practitioners could improve the video quality by cooperating with media agencies and avoiding unexplained terminologies.”
When health care providers post on social media, they must bear in mind that they have legal and ethical duties to their patients, profession and society, said Elizabeth Levy, founder and director of Physicians for Justice in Irvine, Calif., a nonprofit network of volunteer physicians partnering with public interest lawyers to address the social determinants of health.
“Providers are also responsible for understanding the mechanics of their posts,” such as who can see these messages and how long they stay up, Levy said. As a starting point for figuring what’s acceptable, providers could look at social media guidelines put out by their professional associations. Even beyond that, though, they must exercise prudent judgment. “As social media continues to evolve, providers will also need to stay updated with the changing risks and benefits of participation.”
Patients often research their providers online, so finding them on social media can help inform about values and approaches to care, said M. Sara Rosenthal, a professor and founding director of the program for bioethics and chair of the hospital ethics committee at the University of Kentucky College of Medicine.
Health care providers’ posts on social media also could promote patient education. They can advance informed consent and help patients navigate the risks and benefits of various treatments or preventive options. However, providers could violate ethical principles if they espouse “harmful, risky or questionable therapies or medical advice that is contrary to clinical practice guidelines or accepted standards of care,” Rosenthal said.
Inappropriate self-disclosure also can affect a provider’s reputation, said Kelly Michelson, a professor of pediatrics and director of the Center for Bioethics and Medical Humanities at Northwestern University’s Feinberg School of Medicine. A clinician’s obligations to professionalism extend beyond those moments when they are directly taking care of their patients, she said. “Many experts recommend against clinicians ‘friending’ patients or the families on social media because it blurs the patient-clinician boundary.”
Meanwhile, clinicians need to adhere closely to confidentiality. In sharing a patient’s case online for educational purposes, safeguarding identity becomes paramount. Removing names and changing minor details is insufficient, Michelson said.
“The patient-clinician relationship is sacred, and it can only be effective if patients have 100 percent confidence that all that happens with their clinician is kept in the strictest of confidence,” she said, adding that health care providers also should avoid obtaining information about their patients from social media because it can lead to bias and risk jeopardizing objectivity.
Academic clinicians can use social media as a recruitment tool to expand the pool of research participants for their studies, Michelson said. Because the majority of clinical research is conducted at academic medical centers, large segments of the population are excluded. “This affects the quality of the data and knowledge we gain from research,” she said.
Don S. Dizon, a professor of medicine and surgery at the Warren Alpert Medical School of Brown University in Providence, Rhode Island, uses LinkedIn and Doximity, as well as Twitter, Instagram, TikTok, Facebook, and most recently, YouTube and Post. He’s on Twitter nearly every day, where he interacts with the oncology community and his medical colleagues.
Also, he said, “I really like Instagram. It’s where you will see a hybrid of who I am professionally and personally. I’ve become comfortable sharing both up to a limit, but where else can I combine my appreciation of clothes with my professional life?” On that site, he’s seen sporting shirts with polka dots or stripes and an occasional bow-tie. He also posts photos of his cats.

Don S. Dizon, a professor of medicine and surgery at Brown, started using TikTok several years ago, telling medical stories in short-form videos.
Don S. Dizon
Dizon started using TikTok several years ago, telling medical stories in short-form videos. He may talk about an inspirational patient, his views on end-of-life care and death, or memories of people who have passed. But he is careful not to divulge any details that would identify anyone.
Recently, some people have become his patients after viewing his content on social media or on the Internet in general, which he clearly states isn’t a forum for medical advice. “In both situations, they are so much more relaxed when we meet, because it’s as if they have a sense of who I am as a person,” Dizon said. “I think that has helped so much in talking through a cancer diagnosis and a treatment plan, and yes, even discussions about prognosis.”
He also posts about equity and diversity. “I have found myself more likely to repost or react to issues that are inherently political, including racism, homophobia, transphobia and lack-of-access issues, because medicine is not isolated from society, and I truly believe that medicine is a social justice issue,” said Dizon, who is vice chair of diversity, equity, inclusion and professional integrity at the SWOG Cancer Research Network.
Through it all, Dizon likes “to break through the notion of doctor as infallible and all-knowing, the doctor as deity,” he said. “Humanizing what I do, especially in oncology, is something that challenges me on social media, and I appreciate the opportunities to do it on TikTok.”
Could this habit related to eating slow down rates of aging?
Previous research showed that restricting calories results in longer lives for mice, worms and flies. A new study by Columbia University researchers applied those findings to people. But what does this paper actually show?
Last Thursday, scientists at Columbia University published a new study finding that cutting down on calories could lead to longer, healthier lives. In the phase 2 trial, 220 healthy people without obesity dropped their calories significantly and, at least according to one test, their rate of biological aging slowed by 2 to 3 percent in over a couple of years. Small though that may seem, the researchers estimate that it would translate into a decline of about 10 percent in the risk of death as people get older. That's basically the same as quitting smoking.
Previous research has shown that restricting calories results in longer lives for mice, worms and flies. This research is unique because it applies those findings to people. It was published in Nature Aging.
But what did the researchers actually show? Why did two other tests indicate that the biological age of the research participants didn't budge? Does the new paper point to anything people should be doing for more years of healthy living? Spoiler alert: Maybe, but don't try anything before talking with a medical expert about it. I had the chance to chat with someone with inside knowledge of the research -- Dr. Evan Hadley, director of the National Institute of Aging's Division of Geriatrics and Clinical Gerontology, which funded the study. Dr. Hadley describes how the research participants went about reducing their calories, as well as the risks and benefits involved. He also explains the "aging clock" used to measure the benefits.

Evan Hadley, Director of the Division of Geriatrics and Clinical Gerontology at the National Institute of Aging
NIA

