A Tool for Disease Detection Is Right Under Our Noses
In March, researchers published a review that lists which organic chemicals match up with certain diseases and biomarkers in the skin, saliva and urine. It’s an important step in creating a robot nose that can reliably detect diseases.
The doctor will sniff you now? Well, not on his or her own, but with a device that functions like a superhuman nose. You’ll exhale into a breathalyzer, or a sensor will collect “scent data” from a quick pass over your urine or blood sample. Then, AI software combs through an olfactory database to find patterns in the volatile organic compounds (VOCs) you secreted that match those associated with thousands of VOC disease biomarkers that have been identified and cataloged.
No further biopsy, imaging test or procedures necessary for the diagnosis. According to some scientists, this is how diseases will be detected in the coming years.
All diseases alter the organic compounds found in the body and their odors. Volatolomics is an emerging branch of chemistry that uses the smell of gases emitted by breath, urine, blood, stool, tears or sweat to diagnose disease. When someone is sick, the normal biochemical process is disrupted, and this alters the makeup of the gas, including a change in odor.
“These metabolites show a snapshot of what’s going on with the body,” says Cristina Davis, a biomedical engineer and associate vice chancellor of Interdisciplinary Research and Strategic Initiatives at the University of California, Davis. This opens the door to diagnosing conditions even before symptoms are present. It’s possible to detect a sweet, fruity smell in the breath of someone with diabetes, for example.
Hippocrates may have been the first to note that people with certain diseases give off an odor but dogs provided the proof of concept. Scientists have published countless studies in which dogs or other high-performing smellers like rodents have identified people with cancer, lung disease or other conditions by smell alone. The brain region that analyzes smells is proportionally about 40 times greater in dogs than in people. The noses of rodents are even more powerful.
Take prostate cancer, which is notoriously difficult to detect accurately with standard medical testing. After sniffing a tiny urine sample, trained dogs were able to pick out prostate cancer in study subjects more than 96 percent of the time, and earlier than a physician could in some cases.
But using dogs as bio-detectors is not practical. It is labor-intensive, complicated and expensive to train dogs to bark or lie down when they smell a certain VOC, explains Bruce Kimball, a chemical ecologist at the Monell Chemical Senses Center in Philadelphia. Kimball has trained ferrets to scratch a box when they smell a specific VOC so he knows. The lab animal must be taught to distinguish the VOC from background odors and trained anew for each disease scent.

In the lab of chemical ecologist Bruce Kimball, ferrets were trained to scratch a box when they identified avian flu in mallard ducks.
Glen J. Golden
There are some human super-smellers among us. In 2019, Joy Milne of Scotland proved she could unerringly identify people with Parkinson’s disease from a musky scent emitted from their skin. Clinical testing showed that she could distinguish the odor of Parkinson’s on a worn t-shirt before clinical symptoms even appeared.
Hossam Haick, a professor at Technion-Israel Institute of Technology, maintains that volatolomics is the future of medicine. Misdiagnosis and late detection are huge problems in health care, he says. “A precise and early diagnosis is the starting point of all clinical activities.” Further, this science has the potential to eliminate costly invasive testing or imaging studies and improve outcomes through earlier treatment.
The Nose Knows a Lot
“Volatolomics is not a fringe theory. There is science behind it,” Davis stresses. Every VOC has its own fingerprint, and a method called gas chromatography-mass spectrometry (GCMS) uses highly sensitive instruments to separate the molecules of these VOCs to determine their structures. But GCMS can’t discern the telltale patterns of particular diseases, and other technologies to analyze biomarkers have been limited.
We have technology that can see, hear and sense touch but scientists don’t have a handle yet on how smell works. The ability goes beyond picking out a single scent in someone’s breath or blood sample. It’s the totality of the smell—not the smell of a single chemical— which defines a disease. The dog’s brain is able to infer something when they smell a VOC that eludes human analysis so far.
Odor is a complex ecosystem and analyzing a VOC is compounded by other scents in the environment, says Kimball. A person’s diet and use of tobacco or alcohol also will affect the breath. Even fluctuations in humidity and temperature can contaminate a sample.
If successful, a sophisticated AI network can imitate how the dog brain recognizes patterns in smells. Early versions of robot noses have already been developed.
With today’s advances in data mining, AI and machine learning, scientists are trying to create mechanical devices that can draw on algorithms based on GCMS readings and data about diseases that dogs have sniffed out. If successful, a sophisticated AI network can imitate how the dog brain recognizes patterns in smells.
In March, Nano Research published a comprehensive review of volatolomics in health care authored by Haick and seven colleagues. The intent was to bridge gaps in the field for scientists trying to connect the biomarkers and sensor technology needed to develop a robot nose. This paper serves as a reference manual for the field that lists which VOCs are associated with what disease and the biomarkers in skin, saliva, breath, and urine.
Weiwei Wu, one of the co-authors and a professor at Xidian University in China, explains that creating a robotic nose requires the expertise of chemists, computer scientists, electrical engineers, material scientists, and clinicians. These researchers use different terms and methodologies and most have not collaborated before with the other disciplines. “The electrical engineers know the device but they don’t know as much about the biomarkers they need to detect,” Wu offers as an example.
This review is significant, Wu continues, because it can facilitate progress in the field by providing experts in all the disciplines with the basic knowledge needed to create an effective robot nose for diagnostic use. The paper also includes a systematic summary of the research methodology of volatolomics.
Once scientists build a stronger database of VOCs, they can program a device to identify critical patterns of specified diseases on a reliable basis. On a machine learning model, the algorithms automatically get better at diagnosing with each use. Wu envisions further tweaks in the next few years to make the devices smaller and consume less power.
A Whiff of the Future
Early versions of robot noses have already been developed. Some of them use chemical sensors to pick up smells in the breath or other body emission molecules. That data is sent through an electrical signal to a computer network for interpretation and possible linkage to a disease.
This electronic nose, or e-nose, has been successful in small pilot studies at labs around the world. At Ben-Gurion University in Israel, researchers detected breast cancer with electronic gas sensors with 95% accuracy, a higher sensitivity than mammograms. Other robot noses, called p-noses, use photons instead of electrical signals.
The mechanical noses being developed tap different methodologies and analytic techniques which makes it hard to compare them. Plus, the devices are intended for varying uses. One team, for example, is working on an e-nose that can be waved over a plate to screen for the presence of a particular allergen when you’re dining out.
A robot nose could be used as a real-time diagnostic tool in clinical practice. Kimball is working on one such tool that can distinguish between a viral and bacterial infection. This would enable physicians to determine whether an antibiotic prescription is appropriate without waiting for a lab result.
Davis is refining a hand-held device that identifies COVID-19 through a simple breath test. She sees the tool being used at crowded airports, sports stadiums and concert venues where PCR or rapid antigen testing is impractical. Background air samples are collected from the space so that those signals can be removed from the human breath measurement. “[The sensor tool] has the same accuracy as the rapid antigen test kits but exhaled breath is easier to collect,” she notes.

The NaNose, also known as the SniffPhone, uses tiny sensors boosted by AI to distinguish Alzheimer's, Crohn's disease, the early stages of several cancers, and other diseases with 84 to 98 percent accuracy.
Hossam Haick
Haick named his team’s robot nose, “NaNose,” since it is based on nanotechnology; the prototype is called the SniffPhone. Using tiny sensors boosted by AI, it can distinguish 23 diseases in human subjects with 84 to 98 percent accuracy. This includes early stages of several cancers, Alzheimer’s, tuberculosis and Crohn’s disease. His team has been raising the accuracy level by combining biomarker signals from both breath and skin, for example. The goal is to achieve 99.9 percent accuracy consistently so no other diagnostic tests would be needed before treating the patient. Plus, it will be affordable, he says.
Kimball predicts we’ll be seeing these diagnostic tools in the next decade. “The physician would narrow down what [the diagnosis] might be and then get the correct tool,” he says. Others are envisioning one device that can screen for multiple diseases by programming the software, which would be updated regularly with new findings.
Larger volatolomics studies must be conducted before these e-noses are ready for clinical use, however. Experts also need to learn how to establish normal reference ranges for e-nose readings to support clinicians using the tool.
“Taking successful prototypes from the lab to industry is the challenge,” says Haick, ticking off issues like reproducibility, mass production and regulation. But volatolomics researchers are unanimous in believing the future of health care is so close they can smell it.
CandyCodes could provide sweet justice against fake pills
A bioengineer at the University of California, Riverside, may have found a way to prevent counterfeit medications: pill coatings inspired by the sprinkles on baked goods and candies.
When we swallow a pill, we hope it will work without side effects. Few of us know to worry about a growing issue facing the pharmaceutical industry: counterfeit medications. These pills, patches, and other medical products might look just like the real thing. But they’re often stuffed with fillers that dilute the medication’s potency or they’re simply substituted for lookalikes that contain none of the prescribed medication at all.
Now, bioengineer William Grover at the University of California, Riverside, may have a solution. Inspired by the tiny, multi-colored sprinkles called nonpareils that decorate baked goods and candies, Grover created CandyCodes pill coatings to prevent counterfeits.
The idea was borne out of pandemic boredom. Confined to his home, Grover was struck by the patterns of nonpareils he saw on candies, and found himself counting the number of little balls on each one. “It’s random, how they’re applied,” he says. “I wondered if it ever repeats itself or if each of these candies is unique in the entire world.” He suspected the latter, and some quick math proved his hypothesis: Given dozens of nonpareils per candy in a handful of different colors, it’s highly unlikely that the sprinklings on any two candies would be identical.
He quickly realized his finding could have practical applications: pills or capsules could be coated with similar “sprinkles,” with the manufacturer photographing each pill or capsule before selling its products. Consumers looking to weed out fakes could potentially take a photo with their cell phones and go online to compare images of their own pills to the manufacturer’s database, with the help of an algorithm that would determine their authenticity. Or, a computer could generate another type of unique identifier, such as a text-based code, tracking to the color and location of the sprinkles. This would allow for a speedier validation than a photo-based comparison, Grover says. “It could be done very quickly, in a fraction of a second.”
Researchers and manufacturers have already developed some anti-counterfeit tools, including built-in identifiers like edible papers with scannable QR codes. But such methods, while functional, can be costly to implement, Grover says.
It wouldn’t be paranoid to take such precautions. Counterfeits are a growing problem, according to Young Kim, a biomedical engineer at Purdue University who was not involved in the CandyCodes study. “There are approximately 40,000 online pharmacies that one can access via the Internet,” he says. “Only three to four percent of them are operated legally.” Purchases from online pharmacies rose dramatically during the pandemic, and Kim expects a boom in counterfeit medical products alongside it.
The FDA warns that U.S. consumers can be exposed to counterfeits through online purchases, in particular. The problem is magnified in low- to middle-income nations, where one in 10 medical products are counterfeit, according to a World Health Organization estimate. Cost doesn’t seem to be a factor, either; antimalarials and antibiotics are most often reported as counterfeits or fakes, and generic medications are swapped as often as brand-name drugs, according to the same WHO report.
Counterfeits weren’t tracked globally until 2013; since then, there have been 1,500 reports to the WHO, with actual incidences of counterfeiting likely much higher. Fake medicines have been estimated to result in costs of $200 billion each year, and are blamed for more than 72,000 pneumonia- and 116,000 malaria-related deaths.
Researchers and manufacturers have already developed some anti-counterfeit tools, including built-in identifiers like edible papers with scannable QR codes or barcodes that are stamped onto or otherwise incorporated into pills and other medical products. But such methods, while functional, can be costly to implement, Grover says.

CandyCodes could provide unique identifiers for at least 41 million pills for every person on the planet.
William Grover
“Putting universal codes on each pill and each dosage is attractive,” he says. “The challenge is, how can we do it in a way that requires as little modification to the existing manufacturing process as possible? That's where I hope CandyCodes have an edge. It's not zero modification, but I hope it is as minor a modification of the manufacturing process as possible.”
Kim calls the concept “a clever idea to introduce entropy for high-level security” even if it may not be as close to market as other emerging technologies, including some edible watermarks he’s helped develop. He points out that CandyCodes still needs to be tested for reproducibility and readability.
The possibilities are already intriguing, though. Grover’s recent research, published in Scientific Reports, predicts that unique codes could be used for at least 41 million pills for every person on the planet.
Sadly, CandyCodes’ multicolored bits probably won’t taste like candy. They must be made of non-caloric ingredients to meet the international regulatory standards that govern food dyes and colorants. But Grover hopes CandyCodes represent a simple, accessible solution to a heart-wrenching issue. “This feels like trying to track down and go after bad guys,” he says. “Someone who would pass off a medicine intended for a child or a sick person and pass it off as something effective, I can't imagine anything much more evil than that. It's fun and, and a little fulfilling to try to develop technologies that chip away at that.”
New gene therapy helps patients with rare disease. One mother wouldn't have it any other way.
A biotech in Cambridge, Mass., is targeting a rare disease called cystinosis with gene therapy. It's been effective for five patients in a clinical trial that's still underway.
Three years ago, Jordan Janz of Consort, Alberta, knew his gene therapy treatment for cystinosis was working when his hair started to darken. Pigmentation or melanin production is just one part of the body damaged by cystinosis.
“When you have cystinosis, you’re either a redhead or a blonde, and you are very pale,” attests Janz, 23, who was diagnosed with the disease just eight months after he was born. “After I got my new stem cells, my hair came back dark, dirty blonde, then it lightened a little bit, but before it was white blonde, almost bleach blonde.”
According to Cystinosis United, about 500 to 600 people have the rare genetic disease in the U.S.; an estimated 20 new cases are diagnosed each year.
Located in Cambridge, Mass., AVROBIO is a gene therapy company that targets cystinosis and other lysosomal storage disorders, in which toxic materials build up in the cells. Janz is one of five patients in AVROBIO’s ongoing Phase 1/2 clinical trial of a gene therapy for cystinosis called AVR-RD-04.
Recently, AVROBIO compiled positive clinical data from this first and only gene therapy trial for the disease. The data show the potential of the therapy to genetically modify the patients’ own hematopoietic stem cells—a certain type of cell that’s capable of developing into all different types of blood cells—to express the functional protein they are deficient in. It stabilizes or reduces the impact of cystinosis on multiple tissues with a single dose.
Medical researchers have found that more than 80 different mutations to a gene called CTNS are responsible for causing cystinosis. The most common mutation results in a deficiency of the protein cystinosin. That protein functions as a transporter that regulates a lot metabolic processes in the cells.
“One of the first things we see in patients clinically is an accumulation of a particular amino acid called cystine, which grows toxic cystine crystals in the cells that cause serious complications,” explains Essra Rihda, chief medical officer for AVROBIO. “That happens in the cells across the tissues and organs of the body, so the disease affects many parts of the body.”

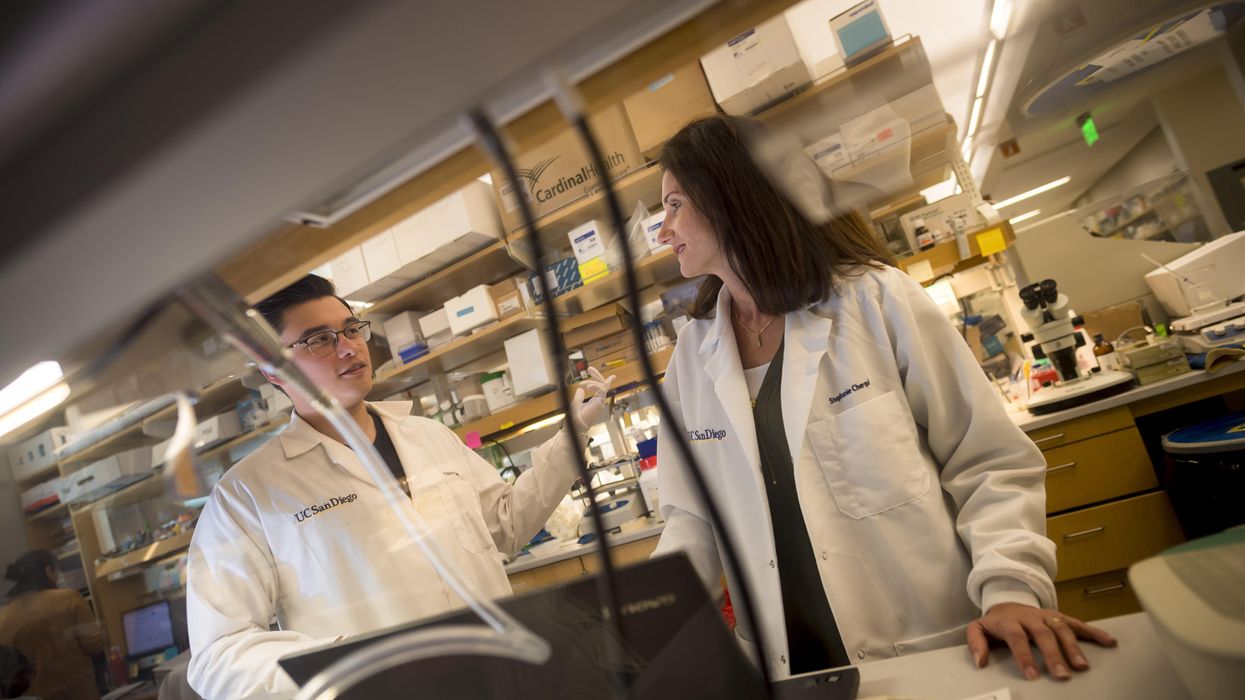
Jordan Janz, 23, meets Stephanie Cherqui, the principal investigator of his gene therapy trial, before the trial started in 2019.
Jordan Janz
According to Rihda, although cystinosis can occur in kids and adults, the most severe form of the disease affects infants and makes up about 95 percent of overall cases. Children typically appear healthy at birth, but around six to 18 months, they start to present for medical attention with failure to thrive.
Additionally, infants with cystinosis often urinate frequently, a sign of polyuria, and they are thirsty all the time, since the disease usually starts in the kidneys. Many develop chronic kidney disease that ultimately progresses to the point where the kidney no longer supports the body’s needs. At that stage, dialysis is required and then a transplant. From there the disease spreads to many other organs, including the eyes, muscles, heart, nervous system, etc.
“The gene for cystinosis is expressed in every single tissue we have, and the accumulation of this toxic buildup alters all of the organs of the patient, so little by little all of the organs start to fail,” says Stephanie Cherqui, principal investigator of Cherqui Lab, which is part of UC San Diego’s Department of Pediatrics.
Since the 1950s, a drug called cysteamine showed some therapeutic effect on cystinosis. It was approved by the FDA in 1994 to prevent damage that may be caused by the buildup of cystine crystals in organs. Prior to FDA approval, Cherqui says, children were dying of the disease before they were ten-years-old or after a kidney transplant. By taking oral cysteamine, they can live from 20 to 50 years longer. But it’s a challenging drug because it has to be taken every 6 or 12 hours, and there are serious gastric side effects such as nausea and diarrhea.
“With all of the complications they develop, the typical patient takes 40 to 60 pills a day around the clock,” Cherqui says. “They literally have a suitcase of medications they have to carry everywhere, and all of those medications don’t stop the progression of the disease, and they still die from it.”
Cherqui has been a proponent of gene therapy to treat children’s disorders since studying cystinosis while earning her doctorate in 2002. Today, her lab focuses on developing stem cell and gene therapy strategies for degenerative, hereditary disorders such as cystinosis that affect multiple systems of the body. “Because cystinosis expresses in every tissue in the body, I decided to use the blood-forming stem cells that we have in our bone marrow,” she explains. “These cells can migrate to anywhere in the body where the person has an injury from the disease.”
AVROBIO’s hematopoietic stem cell gene therapy approach collects stem cells from the patient’s bone marrow. They then genetically modify the stem cells to give the patient a copy of the healthy CTNS gene, which the person either doesn’t have or it’s defective.
The patient first undergoes apheresis, a medical procedure in which their blood is passed through an apparatus that separates out the diseased stem cells, and a process called conditioning is used to help eliminate the damaged cells so they can be replaced by the infusion of the patient’s genetically modified stem cells. Once they become engrafted into the patient’s bone marrow, they reproduce into a lot of daughter cells, and all of those daughter cells contain the CTNS gene. Those cells are able to express the healthy, functional, active protein throughout the body to correct the metabolic problem caused by cystinosis.
“What we’re seeing in the adult patients who have been dosed to date is the consistent and sustained engraftment of our genetically modified cells, 17 to 27 months post-gene therapy, so that’s very encouraging and positive,” says Rihda, the chief medical officer at AVROBIO.
When Janz was 11-years-old, his mother got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. Two years later, she made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial.
AVROBIO researchers have also confirmed stabilization or improvement in motor coordination and visual perception in the trial participants, suggesting a potential impact on the neuropathology of the disease. Data from five dosed patients show strong safety and tolerability as well as reduced accumulation of cystine crystals in cells across multiple tissues in the first three patients. None of the five patients need to take oral cysteamine.
Janz’s mother, Barb Kulyk, whom he credits with always making him take his medications and keeping him hydrated, had been following Cherqui’s research since his early childhood. When Janz was 11-years-old, she got him enrolled in the trial of a new form of cysteamine that would only need to be taken every 12 hours instead of every six. When he was 17, the FDA approved that drug. Two years later, his mother made sure he was the first person on the list for Cherqui’s current stem cell gene therapy trial. He received his new stem cells on October 7th, 2019, went home in January 2020, and returned to working full time in February.

Jordan Janz, pictured here with his girlfriend, has a new lease on life, plus a new hair color.
Jordan Janz
He notes that his energy level is significantly better, and his mother has noticed much improvement in him and his daily functioning: He rarely vomits or gets nauseous in the morning, and he has more color in his face as well as his hair. Although he could finish his participation at any time, he recently decided to continue in the clinical trial.
Before the trial, Janz was taking 56 pills daily. He is completely off all of those medications and only takes pills to keep his kidneys working. Because of the damage caused by cystinosis over the course of his life, he’s down to about 20 percent kidney function and will eventually need a transplant.
“Some day, though, thanks to Dr. Cherqui’s team and AVROBIO’s work, when I get a new kidney, cystinosis won’t destroy it,” he concludes.