The U.S. must fund more biotech innovation – or other countries will catch up faster than you think

In the coming years, U.S. market share in biotech will decline unless the federal government makes investments to improve the quality and quantity of U.S. research, writes the author.
The U.S. has approximately 58 percent of the market share in the biotech sector, followed by China with 11 percent. However, this market share is the result of several years of previous research and development (R&D) – it is a present picture of what happened in the past. In the future, this market share will decline unless the federal government makes investments to improve the quality and quantity of U.S. research in biotech.
The effectiveness of current R&D can be evaluated in a variety of ways such as monies invested and the number of patents filed. According to the UNESCO Institute for Statistics, the U.S. spends approximately 2.7 percent of GDP on R&D ($476,459.0M), whereas China spends 2 percent ($346,266.3M). However, investment levels do not necessarily translate into goods that end up contributing to innovation.
Patents are a better indication of innovation. The biotech industry relies on patents to protect their investments, making patenting a key tool in the process of translating scientific discoveries that can ultimately benefit patients. In 2020, China filed 1,497,159 patents, a 6.9 percent increase in growth rate. In contrast, the U.S. filed 597,172, a 3.9 percent decline. When it comes to patents filed, China has approximately 45 percent of the world share compared to 18 percent for the U.S.
So how did we get here? The nature of science in academia allows scientists to specialize by dedicating several years to advance discovery research and develop new inventions that can then be licensed by biotech companies. This makes academic science critical to innovation in the U.S. and abroad.
Academic scientists rely on government and foundation grants to pay for R&D, which includes salaries for faculty, investigators and trainees, as well as monies for infrastructure, support personnel and research supplies. Of particular interest to academic scientists to cover these costs is government support such as Research Project Grants, also known as R01 grants, the oldest grant mechanism from the National Institutes of Health. Unfortunately, this funding mechanism is extremely competitive, as applications have a success rate of only about 20 percent. To maximize the chances of getting funded, investigators tend to limit the innovation of their applications, since a project that seems overambitious is discouraged by grant reviewers.
Considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation.
This approach affects the future success of the R&D enterprise in the U.S. Pursuing less innovative work tends to produce scientific results that are more obvious than groundbreaking, and when a discovery is obvious, it cannot be patented, resulting in fewer inventions that go on to benefit patients. Even though there are governmental funding options available for scientists in academia focused on more groundbreaking and translational projects, those options are less coveted by academic scientists who are trying to obtain tenure and long-term funding to cover salaries and other associated laboratory expenses. Therefore, since only a small percent of projects gets funded, the likelihood of scientists interested in pursuing academic science or even research in general keeps declining over time.
Efforts to raise the number of individuals who pursue a scientific education are paying off. However, the number of job openings for those trainees to carry out independent scientific research once they graduate has proved harder to increase. These limitations are not just in the number of faculty openings to pursue academic science, which are in part related to grant funding, but also the low salary available to pay those scientists after they obtain their doctoral degree, which ranges from $53,000 to $65,000, depending on years of experience.
Thus, considering the difficulty in obtaining funding, the limited number of opportunities for scientists to become independent investigators capable of leading their own scientific projects, and the salaries available to pay for scientists with a doctoral degree, it is not surprising that the U.S. is progressively losing its workforce for innovation, which results in fewer patents filed.
Perhaps instead of encouraging scientists to propose less innovative projects in order to increase their chances of getting grants, the U.S. government should give serious consideration to funding investigators for their potential for success -- or the success they have already achieved in contributing to the advancement of science. Such a funding approach should be tiered depending on career stage or years of experience, considering that 42 years old is the median age at which the first R01 is obtained. This suggests that after finishing their training, scientists spend 10 years before they establish themselves as independent academic investigators capable of having the appropriate funds to train the next generation of scientists who will help the U.S. maintain or even expand its market share in the biotech industry for years to come. Patenting should be given more weight as part of the academic endeavor for promotion purposes, or governmental investment in research funding should be increased to support more than just 20 percent of projects.
Remaining at the forefront of biotech innovation will give us the opportunity to not just generate more jobs, but it will also allow us to attract the brightest scientists from all over the world. This talented workforce will go on to train future U.S. scientists and will improve our standard of living by giving us the opportunity to produce the next generation of therapies intended to improve human health.
This problem cannot rely on just one solution, but what is certain is that unless there are more creative changes in funding approaches for scientists in academia, eventually we may be saying “remember when the U.S. was at the forefront of biotech innovation?”
How Excessive Regulation Helped Ignite COVID-19's Rampant Spread
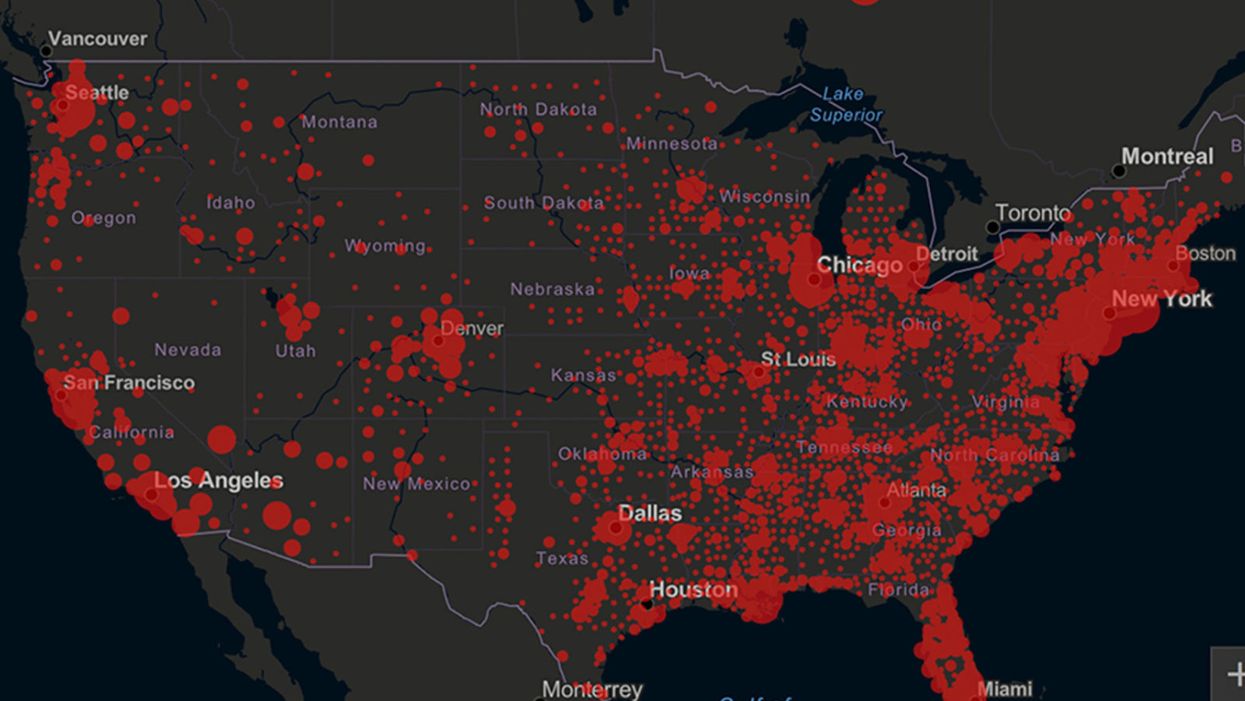
Screenshot of an interactive map of coronavirus cases across the United States, current as of 1:45 p.m. Pacific time on Tuesday, March 31st. Full map accessible at https://coronavirus.jhu.edu/map.html
When historians of the future look back at the 2020 pandemic, the heroic work of Helen Y. Chu, a flu researcher at the University of Washington, will be worthy of recognition.
Chu's team bravely defied the order and conducted the testing anyway.
In late January, Chu was testing nasal swabs for the Seattle Flu Study to monitor influenza spread when she learned of the first case of COVID-19 in Washington state. She deemed it a pressing public health matter to document if and how the illness was spreading locally, so that early containment efforts could succeed. So she sought regulatory approval to adapt the Flu Study to test for the coronavirus, but the federal government denied the request because the original project was funded to study only influenza.
Aware of the urgency, Chu's team bravely defied the order and conducted the testing anyway. Soon they identified a local case in a teenager without any travel history, followed by others. Still, the government tried to shutter their efforts until the outbreak grew dangerous enough to command attention.
Needless testing delays, prompted by excessive regulatory interference, eliminated any chances of curbing the pandemic at its initial stages. Even after Chu went out on a limb to sound alarms, a heavy-handed bureaucracy crushed the nation's ability to roll out early and widespread testing across the country. The Centers for Disease Control and Prevention infamously blundered its own test, while also impeding state and private labs from coming on board, fueling a massive shortage.
The long holdup created "a backlog of testing that needed to be done," says Amesh Adalja, an infectious disease specialist who is a senior scholar at the Johns Hopkins University Center for Health Security.
In a public health crisis, "the ideal situation" would allow the government's test to be "supplanted by private laboratories" without such "a lag in that transition," Adalja says. Only after the eventual release of CDC's test could private industry "begin in earnest" to develop its own versions under the Food and Drug Administration's emergency use authorization.
In a statement, CDC acknowledged that "this process has not gone as smoothly as we would have liked, but there is currently no backlog for testing at CDC."
Now, universities and corporations are in a race against time, playing catch up as the virus continues its relentless spread, also afflicting many health care workers on the front lines.
"Home-testing accessibility is key to preventing further spread of the COVID-19 pandemic."
Hospitals are attempting to add the novel coronavirus to the testing panel of their existent diagnostic machines, which would reduce the results processing time from 48 hours to as little as four hours. Meanwhile, at least four companies announced plans to deliver at-home collection tests to help meet the demand – before a startling injunction by the FDA halted their plans.
Everlywell, an Austin, Texas-based digital health company, had been set to launch online sales of at-home collection kits directly to consumers last week. Scaling up in a matter of days to an initial supply of 30,000 tests, Everlywell collaborated with multiple laboratories where consumers could ship their nasal swab samples overnight, projecting capacity to screen a quarter-million individuals on a weekly basis, says Frank Ong, chief medical and scientific officer.
Secure digital results would have been available online within 48 hours of a sample's arrival at the lab, as well as a telehealth consultation with an independent, board-certified doctor if someone tested positive, for an inclusive $135 cost. The test has a less than 3 percent false-negative rate, Ong says, and in the event of an inadequate self-swab, the lab would not report a conclusive finding. "Home-testing accessibility," he says, "is key to preventing further spread of the COVID-19 pandemic."
But on March 20, the FDA announced restrictions on home collection tests due to concerns about accuracy. The agency did note "the public health value in expanding the availability of COVID-19 testing through safe and accurate tests that may include home collection," while adding that "we are actively working with test developers in this space."
After the restrictions were announced, Everlywell decided to allocate its initial supply of COVID-19 collection kits to hospitals, clinics, nursing homes, and other qualifying health care companies that can commit to no-cost screening of frontline workers and high-risk symptomatic patients. For now, no consumers can order a home-collection test.
"Losing two months is close to disastrous, and that's what we did."
Currently, the U.S. has ramped up to testing an estimated 100,000 people a day, according to Stat News. But 150,000 or more Americans should be tested every day, says Ashish Jha, professor and director of the Harvard Global Health Institute. Due to the dearth of tests, many sick people who suspect they are infected still cannot get confirmation unless they need to be hospitalized.
To give a concrete sense of how far behind we are in testing, consider Palm Beach County, Fla. The state's only drive-thru test center just opened there, requiring an appointment. The center aims to test 750 people per day, but more than 330,000 people have already called to try to book a slot.
"This is such a rapidly moving infection that losing a few days is bad, and losing a couple of weeks is terrible," says Jha, a practicing general internist. "Losing two months is close to disastrous, and that's what we did."
At this point, it will take a long time to fully ramp up. "We are blindfolded," he adds, "and I'd like to take the blindfolds off so we can fight this battle with our eyes wide open."
Better late than never: Yesterday, FDA Commissioner Stephen Hahn said in a statement that the agency has worked with more than 230 test developers and has approved 20 tests since January. An especially notable one was authorized last Friday – 67 days since the country's first known case in Washington state. It's a rapid point-of-care test from medical-device firm Abbott that provides positive results in five minutes and negative results in 13 minutes. Abbott will send 50,000 tests a day to urgent care settings. The first tests are expected to ship tomorrow.
Your Privacy vs. the Public's Health: High-Tech Tracking to Fight COVID-19 Evokes Orwell
Governments around the world are using technology to track their citizens to contain COVID-19.
The COVID-19 pandemic has placed public health and personal privacy on a collision course, as smartphone technology has completely rewritten the book on contact tracing.
It's not surprising that an autocratic regime like China would adopt such measures, but democracies such as Israel have taken a similar path.
The gold standard – patient interviews and detective work – had been in place for more than a century. It's been all but replaced by GPS data in smartphones, which allows contact tracing to occur not only virtually in real time, but with vastly more precision.
China has gone the furthest in using such tech to monitor and prevent the spread of the coronavirus. It developed an app called Health Code to determine which of its citizens are infected or at risk of becoming infected. It has assigned each individual a color code – red, yellow or green – and restricts their movement depending on their assignment. It has also leveraged its millions of public video cameras in conjunction with facial recognition tech to identify people in public who are not wearing masks.
It's not surprising that an autocratic regime like China would adopt such measures, but democracies such as Israel have taken a similar path. The national security agency Shin Bet this week began analyzing all personal cellphone data under emergency measures approved by the government. It texts individuals when it's determined they had been in contact with someone who had the coronavirus. In Spain and China, police have sent drones aloft searching for people violating stay-at-home orders. Commands to disperse can be issued through audio systems built into the aircraft. In the U.S., efforts are underway to lift federal restrictions on drones so that police can use them to prevent people from gathering.
The chief executive of a drone manufacturer in the U.S. aptly summed up the situation in an interview with the Financial Times: "It seems a little Orwellian, but this could save lives."
Epidemics and how they're surveilled often pose thorny dilemmas, according to Craig Klugman, a bioethicist and professor of health sciences at DePaul University in Chicago. "There's always a moral issue to contact tracing," he said, adding that the issue doesn't change by nation, only in the way it's resolved.
"Once certain privacy barriers have been breached, it can be difficult to roll them back again."
In China, there's little to no expectation for privacy, so their decision to take the most extreme measures makes sense to Klugman. "In China, the community comes first. In the U.S., individual rights come first," he said.
As the U.S. has scrambled to develop testing kits and manufacture ventilators to identify potential patients and treat them, individual rights have mostly not received any scrutiny. However, that could change in the coming weeks.
The American approach is also leaning toward using smartphone apps, but in a way that may preserve the privacy of users. Researchers at MIT have released a prototype known as Private Kit: Safe Paths. Patients diagnosed with the coronavirus can use the app to disclose their location trail for the prior 28 days to other users without releasing their specific identity. They also have the option of sharing the data with public health officials. But such an app would only be effective if there is a significant number of users.
Singapore is offering a similar app to its citizens known as TraceTogether, which uses both GPS and Bluetooth pings among users to trace potential encounters. It's being offered on a voluntary basis.
The Electronic Frontier Foundation, the leading nonprofit organization defending civil liberties in the digital world, said it is monitoring how these apps are developed and deployed. "Governments around the world are demanding new dragnet location surveillance powers to contain the COVID-19 outbreak," it said in a statement. "But before the public allows their governments to implement such systems, governments must explain to the public how these systems would be effective in stopping the spread of COVID-19. There's no questioning the need for far-reaching public health measures to meet this urgent challenge, but those measures must be scientifically rigorous, and based on the expertise of public health professionals."
Andrew Geronimo, director of the intellectual property venture clinic at the Case Western University School of Law, said that the U.S. government is currently in talks with Facebook, Google and other tech companies about using deidentified location data from smartphones to better monitor the progress of the outbreak. He was hesitant to endorse such a step.
"These companies may say that all of this data is anonymized," he said, "but studies have shown that it is difficult to fully anonymize data sets that contain so much information about us."
Beyond the technical issues, social attitudes may mount another challenge. Epic events such as 9/11 tend to loosen vigilance toward protecting privacy, according to Klugman and Geronimo. And as more people are sickened and hospitalized in the U.S. with COVID-19, Klugman believes more Americans will be willing to allow themselves to be tracked. "If that happens, there needs to be a time limitation," he said.
However, even if time limits are put in place, Geronimo believes it would lead to an even greater rollback of privacy during the next crisis.
"Once certain privacy barriers have been breached, it can be difficult to roll them back again," he warned. "And the prior incidents could always be used as a precedent – or as proof of concept."