Should egg and sperm donors reveal their identities? The debate pivots on genetics and medical history.

Cassandra Adams performs on stage at the Jersey City Theater Center in March 2019 to raise awareness about traumatic experiences that she and others have had with anonymous donor conception.
Until age 35, Cassandra Adams assumed her mother and father were her biological parents. Then she took saliva tests through two genealogy databases—23andMe and AncestryDNA—and discovered a discrepancy in her heritage. In bringing up the matter with her parents, she learned that fertility issues had led the couple to use a sperm donor.
“Most people my age were not told,” said Adams, now 40 and a stay-at-home mom in Jersey City, New Jersey, who is involved with donor-conception advocacy. “Even now, there’s still a lot of secrecy in the industry. There are still many parents who aren’t truthful or planning not to be truthful with their children.”
While some of those offspring may never know a significant part of their medical history, Adams is grateful that she does. Surprisingly, the DNA test revealed Jewish ancestry.
“There are a lot more genetic conditions that run in Jewish families, so it was really important that I get my medical history, because it’s very different from my dad who raised me,” said Adams, who has met her biological father and two of three known half-siblings. As a result of this experience, she converted to Judaism. “It has been a big journey,” she said.
In an era of advancing assisted reproduction technologies, genetics and medical history have become front and center of the debate as to whether or not egg and sperm donations should be anonymous – and whether secrecy is even possible in many cases.
Obstacles to staying anonymous
People looking to become parents can choose what’s called an “identity-release donor,” meaning their child can receive information about the donor when he or she turns 18. There’s no way to ensure that the donor will consent to a relationship at that time. Instead, if a relationship between the donor and child is a priority, parents may decide to use a known donor.
The majority of donors want to remain anonymous, said reproductive endocrinologist Robert Kiltz, founder and director of CNY Fertility in Syracuse, New York. “In general, egg and sperm donation is mostly anonymous, meaning the recipient doesn’t know the donor and the donor doesn’t know the recipient.”
Even if the donor isn’t disclosed, though, the mystery may become unraveled when a donor-conceived person undergoes direct-to-consumer genetic testing through ancestry databases, which are growing in number and popularity. These services offer DNA testing and links to relatives with identifiable information.
In the future, another obstacle to anonymity could be laws that prohibit anonymous sperm and egg donations, if they catch on. In June, Colorado became the first state in the nation to ban anonymous sperm and egg donations. The law, which takes effect in 2025, will give donor-conceived adults the legal authority to obtain their donor’s identity and medical history. It also requires banks that provide sperm and egg collection to keep current medical records and contact information for all donors. Meanwhile, it prohibits donations from those who won’t consent to identity disclosures.
“The tradition of anonymous sperm or egg donation has created a vast array of problems, most significantly that the people thus created want to know who their mommy and daddy are,” said Kenneth W. Goodman, professor and director of the Institute for Bioethics and Health Policy at the University of Miami Miller School of Medicine.
“There are counter arguments on both sides. But the current situation has led to great uncertainty and, in many cases, grief,” Goodman said.
Donors should bear some moral responsibility for their role in reproduction by allowing their identity to be disclosed to donor-conceived individuals when they turn 18, Goodman added, noting that “there are counter arguments on both sides. But the current situation has led to great uncertainty and, in many cases, grief.”
Adams, the Jersey City woman who learned she was Jewish, has channeled these feelings into several works of art and performances on stage at venues such as the Jersey City Theater Center. During these performances, she describes the trauma of “not knowing where we come from [or] who we look like.”
In the last five years, Kathleen “Casey” DiPaola, a lawyer in Albany, New York, who focuses her practice on adoption, assisted reproduction and surrogacy, has observed a big shift toward would-be parents looking to use known sperm donors. On the other hand, with egg donation, “I’m not seeing a whole lot of change,” she said. Compared to sperm donation, more medical screening is involved with egg donation, so donors are primarily found through fertility clinics and egg donor agencies that prefer anonymity. This leads to fewer options for prospective parents seeking an egg donor with disclosed identity, DiPaola said.
Some donors want to keep in touch
Rachel Lemmons, 32, who lives in Denver, grew interested in becoming an egg donor when, as a graduate student in environmental sciences, she saw an online advertisement. “It seemed like a good way to help pay off my student loan debt,” said Lemmons, who is married and has a daughter who will turn 2-years-old in December. She didn’t end up donating until many years later, after she’d paid off the debt. “The primary motivation at that point wasn’t financial,” she said. “Instead, it felt like a really wonderful way to help someone else have a family in a few weeks’ time.”
Lemmons originally donated anonymously because she didn’t know open donations existed. She was content with that until she became aware of donor-conceived individuals’ struggles. “It concerned me that I could potentially be contributing to this,” she said, adding that the egg donor and surrogacy agency and fertility clinic wouldn’t allow her to disclose her identity retroactively.
Since then, she has donated as an open donor, and kept in touch with the recipients through email and video calls. Knowing that they were finally able to have children is “incredibly rewarding,” Lemmons said.
When to tell the kids
Stanton Honig, professor of urology and division chief of sexual and reproductive medicine at Yale School of Medicine, said for years his team has recommended that couples using donor sperm inform children about the role of the donor and their identity. “Honesty is always the best policy, and it is likely that when they become of age, they might or will be able to find out about their biological sperm donor,” he said. “Hiding it creates more of a complicated situation for children in the long run.”
Amy Jones, a 45-year-old resident of Syracuse, N.Y., has three children, including twins, who know they were conceived with anonymous donor eggs from the same individual, so they share the same genetics. Jones, who is a registered nurse and asked for her real name not to be published, told them around age seven.
“The thought of using a known donor brought more concerns—what if she wanted my babies after they were born, or how would I feel if she treated them as her own every time I saw her?” said Jones.
“I did a lot of reading, and all psychologists said that it is best to start the conversation early,” she recalled. “They understood very little of what I was telling them, but through the years, I have brought it up in discussion and encouraged them to ask questions. To this day, they don't seem to be all that interested, but I expect that later on in life they may have more questions.”
Jones and her husband opted to use a donor because premature ovarian failure at age 27 had rendered her infertile. “The decision to use an egg donor was hard enough,” she said. “The thought of using a known donor brought more concerns—what if she wanted my babies after they were born, or how would I feel if she treated them as her own every time I saw her?”
Susan C. Klock, a clinical psychologist in the section of fertility and reproductive medicine at Northwestern University Feinberg School of Medicine, said, “Anonymity is virtually impossible in the age of direct-to-consumer genetic testing.” In addition, “selecting an identity-release donor is typically not the first thing parents are looking at when they select a donor. First and foremost, they are looking for a donor with a healthy medical background. Then they may consider donor characteristics that resemble the parents.”
The donor’s medical history can be critical
Donor agencies rely on the self-reported medical history of egg and sperm donors, which can lead to gaps in learning important information. Knowing a donor’s medical history may have led some families to make different or more well-informed choices.
After Steven Gunner, a donor-conceived adult, suffered from schizophrenia and died of a drug overdose at age 27 in 2020, his parents, who live in New York, learned of a potential genetic link to his mental illness. A website, Donor Sibling Registry, revealed that the sperm donor the couple had used, a college student at the time of donation, had been hospitalized during childhood for schizophrenia and died of a drug overdose at age 46. Gunner’s story inspired Steven’s Law, a bill that was introduced in Congress in July. If passed, it would mandate sperm banks to collect information on donors’ medical conditions, and donors would have to disclose medical information the banks weren’t able to find.
With limited exceptions, the U.S. Food and Drug Administration requires donors to be screened and tested for relevant communicable disease agents and diseases such as HIV, hepatitis viruses B and C, the Zika virus and several STDs. With current technology, it is also impossible to screen for thousands of rare genetic diseases. “If a couple is using IVF (in vitro fertilization) to conceive with the donor gamete, some may opt for pre-implantation genetic testing to assess for chromosomal abnormalities,” Klock said.
Even these precautions wouldn't cover every disease, and some would-be parents don't get the genetic screening. In a situation where one donor has a large number of offspring, it is concerning that he or she can spread a rare disease to multiple people, said Nick Isel, 37, of Yorkville, Illinois, who was conceived with donor sperm due to his parents’ fertility issues. They told him the truth when he was a teenager, and he found his biological father with a journalist’s help.
Since 2016, Isel, who owns a roofing company, has been petitioning the FDA to extend the retention of medical records, requiring the fertility establishment to maintain information on sperm and egg donors for 50 years instead of the current 10-year mandate.
“The lack of family health information,” he said, “is an ongoing, slow-motion public health crisis since donor conception began being regulated by the FDA as a practice.”
Podcast: The Friday Five Weekly Roundup in Health Research
In this week's Friday Five, a new face mask can detect Covid and send an alert to your phone. Plus, promising research for a breakthrough drug to treat schizophrenia, an AI tool that can create new proteins, progress on a longevity drug - and more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five:
- A new mask can detect Covid and send an alert to your phone
- More promising research for a breakthrough drug to treat schizophrenia
- AI tool can create new proteins
- Connections between an unhealthy gut and breast cancer
- Progress on the longevity drug, rapamycin
And an honorable mention this week: Certain exercises may benefit some types of memory more than others
Life is Emerging: Review of Siddhartha Mukherjee’s Song of the Cell
A new book by Pulitzer-winning physician-scientist Siddhartha Mukherjee will be released from Simon & Schuster on October 25, 2022.
The DNA double helix is often the image spiraling at the center of 21st century advances in biomedicine and the growing bioeconomy. And yet, DNA is molecularly inert. DNA, the code for genes, is not alive and is not strictly necessary for life. Ought life be at the center of our communication of living systems? Is not the Cell a superior symbol of life and our manipulation of living systems?
A code for life isn’t a code without the life that instantiates it. A code for life must be translated. The cell is the basic unit of that translation. The cell is the minimal viable package of life as we know it. Therefore, cell biology is at the center of biomedicine’s greatest transformations, suggests Pulitzer-winning physician-scientist Siddhartha Mukherjee in his latest book, The Song of the Cell: The Exploration of Medicine and the New Human.
The Song of the Cell begins with the discovery of cells and of germ theory, featuring characters such as Louis Pasteur and Robert Koch, who brought the cell “into intimate contact with pathology and medicine.” This intercourse would transform biomedicine, leading to the insight that we can treat disease by thinking at the cellular level. The slightest rearrangement of sick cells might be the path toward alleviating suffering for the organism: eroding the cell walls of a bacterium while sparing our human cells; inventing a medium that coaxes sperm and egg to dance into cellular union for in vitro fertilization (IVF); designing molecular missiles that home to the receptors decorating the exterior of cancer cells; teaching adult skin cells to remember their embryonic state for regenerative medicines.
Mukherjee uses the bulk of the book to elucidate key cell types in the human body, along with their “connective relationships” that enable key organs and organ systems to function. This includes the immune system, the heart, the brain, and so on. Mukherjee’s distinctive style features compelling anecdotes and human stories that animate the scientific (and unscientific) processes that have led to our current state of understanding. In his chapter on neurons and the brain, for example, he integrates Santiago Ramon y Cajal’s meticulous black ink sketches of neurons into Mukherjee’s own personal encounter with clinical depression. In one lucid section, he interviews Dr. Helen Mayberg, a pioneering neurologist who takes seriously the descriptive power of her patients’ metaphors, as they suffer from “caves,” “holes,” “voids,” and “force fields” that render their lives gray. Dr. Mayberg aims to stimulate patients’ neuronal cells in a manner that brings back the color.
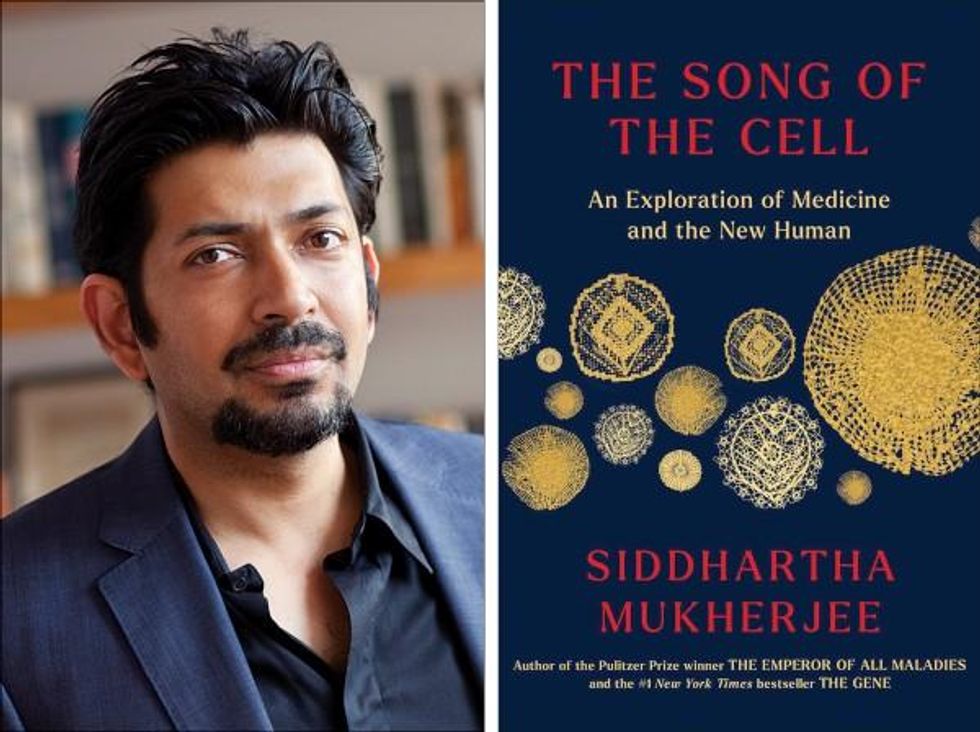
Beyond exposing the insight and inventiveness that has arisen out of cell-based thinking, it seems that Mukherjee’s bigger project is an epistemological one. The early chapters of The Song of the Cell continually hint at the potential for redefining the basic unit of biology as the cell rather than the gene. The choice to center biomedicine around cells is, above all, a conspicuous choice not to center it around genes (the subject of Mukherjee’s previous book, The Gene), because genes dominate popular science communication.
This choice of cells over genes is most welcome. Cells are alive. Genes are not. Letters—such as the As, Cs, Gs, and Ts that represent the nucleotides of DNA, which make up our genes—must be synthesized into a word or poem or song that offers a glimpse into deeper truths. A key idea embedded in this thinking is that of emergence. Whether in ancient myth or modern art, creation tends to be an emergent process, not a linearly coded script. The cell is our current best guess for the basic unit of life’s emergence, turning a finite set of chemical building blocks—nucleic acids, proteins, sugars, fats—into a replicative, evolving system for fighting stasis and entropy. The cell’s song is one for our times, for it is the song of biology’s emergence out of chemistry and physics, into the “frenetically active process” of homeostasis.
Re-centering our view of biology has practical consequences, too, for how we think about diagnosing and treating disease, and for inventing new medicines. Centering cells presents a challenge: which type of cell to place at the center? Rather than default to the apparent simplicity of DNA as a symbol because it represents the one master code for life, the tension in defining the diversity of cells—a mapping process still far from complete in cutting-edge biology laboratories—can help to create a more thoughtful library of cellular metaphors to shape both the practice and communication of biology.
Further, effective problem solving is often about operating at the right level, or the right scale. The cell feels like appropriate level at which to interrogate many of the diseases that ail us, because the senses that guide our own perceptions of sickness and health—the smoldering pain of inflammation, the tunnel vision of a migraine, the dizziness of a fluttering heart—are emergent.
This, unfortunately, is sort of where Mukherjee leaves the reader, under-exploring the consequences of a biology of emergence. Many practical and profound questions have to do with the ways that each scale of life feeds back on the others. In a tome on Cells and “the future human” I wished that Mukherjee had created more space for seeking the ways that cells will shape and be shaped by the future, of humanity and otherwise.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts.
For example, when discussing the regenerative power of pluripotent stem cells, Mukherjee raises the philosophical thought experiment of the Delphic boat, also known as the Ship of Theseus. The boat is made of many pieces of wood, each of which is replaced for repairs over the years, with the boat’s structure unchanged. Eventually none of the boat’s original wood remains: Is it the same boat?
Mukherjee raises the Delphic boat in one paragraph at the end of the chapter on stem cells, as a metaphor related to the possibility of stem cell-enabled regeneration in perpetuity. He does not follow any of the threads of potential answers. Given the current state of cellular engineering, about which Mukherjee is a world expert from his work as a physician-scientist, this book could have used an entire section dedicated to probing this question and, importantly, the ways this thought experiment falls apart.
We are entering a phase of real-world bioengineering that features the modularization of cellular parts within cells, of cells within organs, of organs within bodies, and of bodies within ecosystems. In this reality, we would be unwise to assume that any whole is the mere sum of its parts. Wholeness at any one of these scales of life—organelle, cell, organ, body, ecosystem—is what is at stake if we allow biological reductionism to assume away the relation between those scales.
In other words, Mukherjee succeeds in providing a masterful and compelling narrative of the lives of many of the cells that emerge to enliven us. Like his previous books, it is a worthwhile read for anyone curious about the role of cells in disease and in health. And yet, he fails to offer the broader context of The Song of the Cell.
As leading agronomist and essayist Wes Jackson has written, “The sequence of amino acids that is at home in the human cell, when produced inside the bacterial cell, does not fold quite right. Something about the E. coli internal environment affects the tertiary structure of the protein and makes it inactive. The whole in this case, the E. coli cell, affects the part—the newly made protein. Where is the priority of part now?” [1]
Beyond the ways that different kingdoms of life translate the same genetic code, the practical situation for humanity today relates to the ways that the different disciplines of modern life use values and culture to influence our genes, cells, bodies, and environment. It may be that humans will soon become a bit like the Delphic boat, infused with the buzz of fresh cells to repopulate different niches within our bodies, for healthier, longer lives. But in biology, as in writing, a mixed metaphor can cause something of a cacophony. For we are not boats with parts to be replaced piecemeal. And nor are whales, nor alpine forests, nor topsoil. Life isn’t a sum of parts, and neither is a song that rings true.
[1] Wes Jackson, "Visions and Assumptions," in Nature as Measure (p. 52-53).