A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Meet the Psychologist Using Psychedelics to Treat Racial Trauma
Monnica Williams was stuck. The veteran psychologist wanted to conduct a study using psychedelics, but her university told her they didn't have the expertise to evaluate it via an institutional review board, which is responsible for providing ethical and regulatory oversight for research that involves human participants. Instead, they directed her to a hospital, whose reviewers turned it down, citing research of a banned substance as unethical.
"I said, 'We're not using illegal psilocybin, we're going through Health Canada,'" Williams said. Psilocybin was banned in Canada in 1974, but can now be obtained with an exemption from Health Canada, the federal government's health policy department. After learning this, the hospital review board told Williams they couldn't review her proposal because she's not affiliated with the hospital, after all.
It's all part of balancing bureaucracy with research goals for Williams, a leading expert on racial trauma and psychedelic medicine, as well as obsessive compulsive disorder (OCD), at the University of Ottawa. She's exploring the use of hallucinogenic substances like MDMA and psilocybin — commonly known as ecstasy and magic mushrooms, respectively — to help people of color address the psychological impacts of systemic racism. A prolific researcher, Williams also works as an expert witness, offering clinical evaluations for racial trauma cases.
Scientists have long known that psychedelics produce an altered state of consciousness and openness to new perspectives. For people with mental health conditions who haven't benefited from traditional therapy, psychedelics may be able to help them discover what's causing their pain or trauma, including racial trauma—the mental and emotional injury spurred by racial bias.
"Using psychedelics can not only bring these pain points to the surface for healing, but can reduce the anxiety or response to these memories and allow them to speak openly about them without the pain they bring," Williams says. Her research harnesses the potential of psychedelics to increase neuroplasticity, which includes the brain's ability to build new pathways.
"People of color are dealing with racism all the time, in large and small ways, and even dealing with racism in healthcare, even dealing with racism in therapy."
But she says therapists of color aren't automatically equipped to treat racial trauma. First, she notes, people of color are "vastly underrepresented in the mental health workforce." This is doubly true in psychedelic-assisted psychotherapy, in which a person is guided through a psychedelic session by a therapist or team of therapists, then processes the experience in subsequent therapy sessions.
"On top of that, the therapists of color are getting the same training that the white therapists are getting, so it's not even really guaranteed that they're going to be any better at helping a person that may have racial trauma emerging as part of their experience," she says.
In her own training to become a clinical psychologist at the University of Virginia, Williams says she was taught "how to be a great psychologist for white people." Yet even people of color, she argues, need specialized training to work with marginalized groups, particularly when it comes to MDMA, psilocybin and other psychedelics. Because these drugs can lower natural psychological defense mechanisms, Williams says, it's important for providers to be specially trained.
"People of color are dealing with racism all the time, in large and small ways, and even dealing with racism in healthcare, even dealing with racism in therapy. So [they] generally develop a lot of defenses and coping strategies to ward off racism so that they can function." she says. This is particularly true with psychedelic-assisted psychotherapy: "One possibility is that you're going to be stripped of your defenses, you're going to be vulnerable. And so you have to work with a therapist who is going to understand that and not enact more racism in their work with you."
Williams has struggled to find funding and institutional approval for research involving psychedelics, or funding for investigations into racial trauma or the impacts of conditions like OCD and post-traumatic stress disorder (PTSD) in people of color. With the bulk of her work focusing on OCD, she hoped to focus on people of color, but found there was little funding for that type of research. In 2020, that started to change as structural racism garnered more media attention.
After the killing of George Floyd, a 46-year-old Black man, by a white police officer in May 2020, Williams was flooded with media requests. "Usually, when something like that happens, I get contacted a lot for a couple of weeks, and it dies off. But after George Floyd, it just never did."

Monnica Williams, clinical psychologist at the University of Ottawa
Williams was no stranger to the questions that soon blazed across headlines: How can we mitigate microaggressions? How do race and ethnicity impact mental health? What terms should we use to discuss racial issues? What constitutes an ally, and why aren't there more of them? Why aren't there more people of color in academia, and so many other fields?
Now, she's hoping that the increased attention on racial justice will mean more acceptance for the kind of research she's doing.
In fact, Williams herself has used psychedelics in order to gain a better understanding of how to use them to treat racial trauma. In a study published in January, she and two other Black female psychotherapists took MDMA in a supervised setting, guided by a team of mental health practitioners who helped them process issues that came up as the session progressed. Williams, who was also the study's lead author, found that participants' experiences centered around processing and finding release from racial identities, and, in one case, of simply feeling wholly human without the burden of racial identity for the first time.
The purpose of the study was twofold: to understand how Black women react to psychedelics and to provide safe, firsthand, psychedelic experiences to Black mental health practitioners. One of the other study participants has since gone on to offer psychedelic-assisted psychotherapy to her own patients.
Psychedelic research, and psilocybin in particular, has become a hot topic of late, particularly after Oregon became the first state to legalize it for therapeutic use last November. A survey-based, observational study with 313 participants, published in 2020, paved the way for Williams' more recent MDMA experiments by describing improvements in depression, anxiety and racial trauma among people of color who had used LSD, psilocybin or MDMA in a non-research setting.
Williams and her team included only respondents who reported a moderate to strong psychoactive effect of past psychedelic consumption and believed these experiences provided "relief from the challenging effects of ethnic discrimination." Participants reported a memorable psychedelic experience as well as its acute and lasting effects, completing assessments of psychological insight, mystical experience and emotional challenges experienced during psychedelic experience, then describing their mental health — including depression, anxiety and trauma symptoms — before and after that experience.
Still, Williams says addressing racism is much more complex than treating racial trauma. "One of the questions I get asked a lot is, 'How can Black people cope with racism?' And I don't really like that question," she says. "I think it's important and I don't mind answering it, but I think the more important question is, how can we end racism? What can Black people do to stop racism that's happening to them and what can we do as a society to stop racism? And people aren't really asking this question."
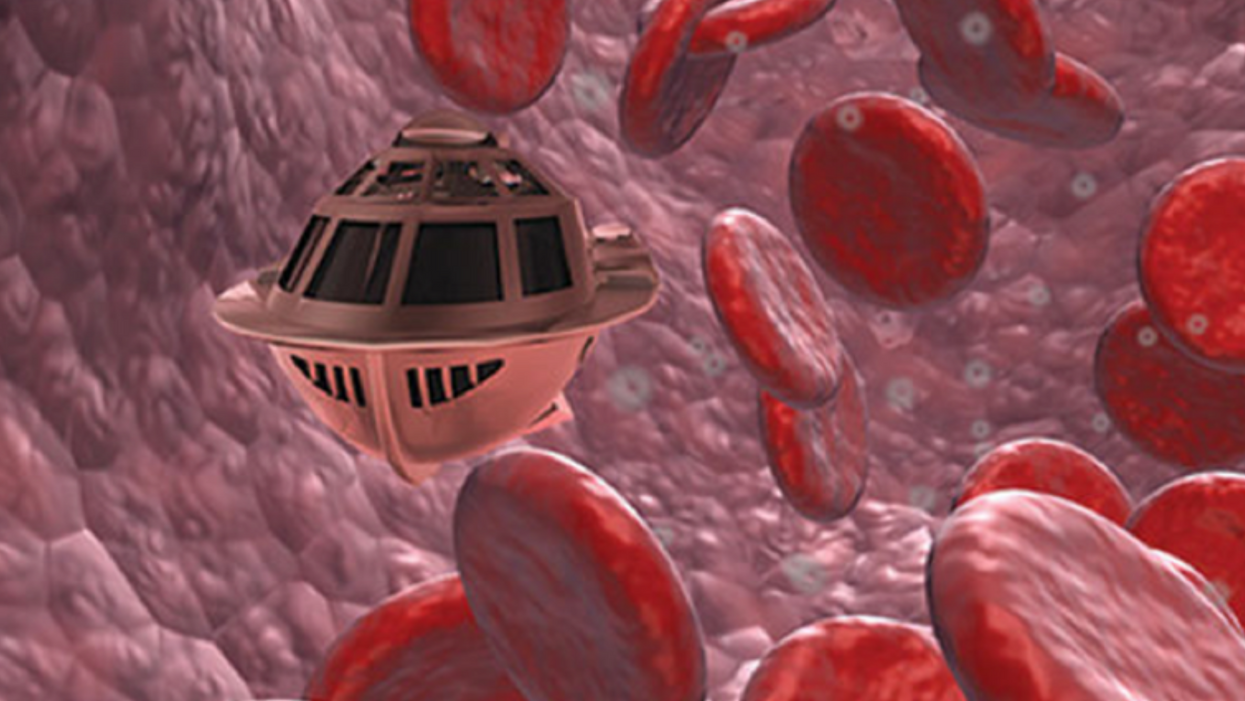
Tiny, Injectable Robots Could Be the Future of Brain Treatments
A movie still from the 1966 film "Fantastic Voyage"
In the 1966 movie "Fantastic Voyage," actress Raquel Welch and her submarine were shrunk to the size of a cell in order to eliminate a blood clot in a scientist's brain. Now, 55 years later, the scenario is becoming closer to reality.
California-based startup Bionaut Labs has developed a nanobot about the size of a grain of rice that's designed to transport medication to the exact location in the body where it's needed. If you think about it, the conventional way to deliver medicine makes little sense: A painkiller affects the entire body instead of just the arm that's hurting, and chemotherapy is flushed through all the veins instead of precisely targeting the tumor.
"Chemotherapy is delivered systemically," Bionaut-founder and CEO Michael Shpigelmacher says. "Often only a small percentage arrives at the location where it is actually needed."
But what if it was possible to send a tiny robot through the body to attack a tumor or deliver a drug at exactly the right location?
Several startups and academic institutes worldwide are working to develop such a solution but Bionaut Labs seems the furthest along in advancing its invention. "You can think of the Bionaut as a tiny screw that moves through the veins as if steered by an invisible screwdriver until it arrives at the tumor," Shpigelmacher explains. Via Zoom, he shares the screen of an X-ray machine in his Culver City lab to demonstrate how the half-transparent, yellowish device winds its way along the spine in the body. The nanobot contains a tiny but powerful magnet. The "invisible screwdriver" is an external magnetic field that rotates that magnet inside the device and gets it to move and change directions.
The current model has a diameter of less than a millimeter. Shpigelmacher's engineers could build the miniature vehicle even smaller but the current size has the advantage of being big enough to see with bare eyes. It can also deliver more medicine than a tinier version. In the Zoom demonstration, the micorobot is injected into the spine, not unlike an epidural, and pulled along the spine through an outside magnet until the Bionaut reaches the brainstem. Depending which organ it needs to reach, it could be inserted elsewhere, for instance through a catheter.
"The hope is that we can develop a vehicle to transport medication deep into the body."
Imagine moving a screw through a steak with a magnet — that's essentially how the device works. But of course, the Bionaut is considerably different from an ordinary screw: "At the right location, we give a magnetic signal, and it unloads its medicine package," Shpigelmacher says.
To start, Bionaut Labs wants to use its device to treat Parkinson's disease and brain stem gliomas, a type of cancer that largely affects children and teenagers. About 300 to 400 young people a year are diagnosed with this type of tumor. Radiation and brain surgery risk damaging sensitive brain tissue, and chemotherapy often doesn't work. Most children with these tumors live less than 18 months. A nanobot delivering targeted chemotherapy could be a gamechanger. "These patients really don't have any other hope," Shpigelmacher says.
Of course, the main challenge of the developing such a device is guaranteeing that it's safe. Because tissue is so sensitive, any mistake could risk disastrous results. Over the past four years, Bionaut has tested its technology in dozens of healthy sheep and pigs with no major adverse effects. Sheep make a good stand-in for humans because their brains and spines are similar to ours.

The Bionaut device is about the size of a grain of rice.
Bionaut Labs
"As the Bionaut moves through brain tissue, it creates a transient track that heals within a few weeks," Shpigelmacher says. The company is hoping to be the first to test a nanobot in humans. That could happen as early as 2023, Shpigelmacher says.
Once the technique has been perfected, further applications could include addressing other kinds of brain disorders that are considered incurable now, such as Alzheimer's or Huntington's disease. "Microrobots could serve as a bridgehead, opening the gateway to the brain and facilitating precise access of deep brain structure – either to deliver medication, take cell samples or stimulate specific brain regions," Shpigelmacher says.
Robot-assisted hybrid surgery with artificial intelligence is already used in state-of-the-art surgery centers, and many medical experts believe that nanorobotics will be the instrument of the future. In 2016, three scientists were awarded the Nobel Prize in Chemistry for their development of "the world's smallest machines," nano "elevators" and minuscule motors. Since then, the scientific experiments have progressed to the point where applicable devices are moving closer to actually being implemented.
Bionaut's technology was initially developed by a research team lead by Peer Fischer, head of the independent Micro Nano and Molecular Systems Lab at the Max Planck Institute for Intelligent Systems in Stuttgart, Germany. Fischer is considered a pioneer in the research of nano systems, which he began at Harvard University more than a decade ago. He and his team are advising Bionaut Labs and have licensed their technology to the company.
"The hope is that we can develop a vehicle to transport medication deep into the body," says Max Planck scientist Tian Qiu, who leads the cooperation with Bionaut Labs. He agrees with Shpigelmacher that the Bionaut's size is perfect for transporting medication loads and is researching potential applications for even smaller nanorobots, especially in the eye, where the tissue is extremely sensitive. "Nanorobots can sneak through very fine tissue without causing damage."
In "Fantastic Voyage," Raquel Welch's adventures inside the body of a dissident scientist let her swim through his veins into his brain, but her shrunken miniature submarine is attacked by antibodies; she has to flee through the nerves into the scientist's eye where she escapes into freedom on a tear drop. In reality, the exit in the lab is much more mundane. The Bionaut simply leaves the body through the same port where it entered. But apart from the dramatization, the "Fantastic Voyage" was almost prophetic, or, as Shpigelmacher says, "Science fiction becomes science reality."