A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
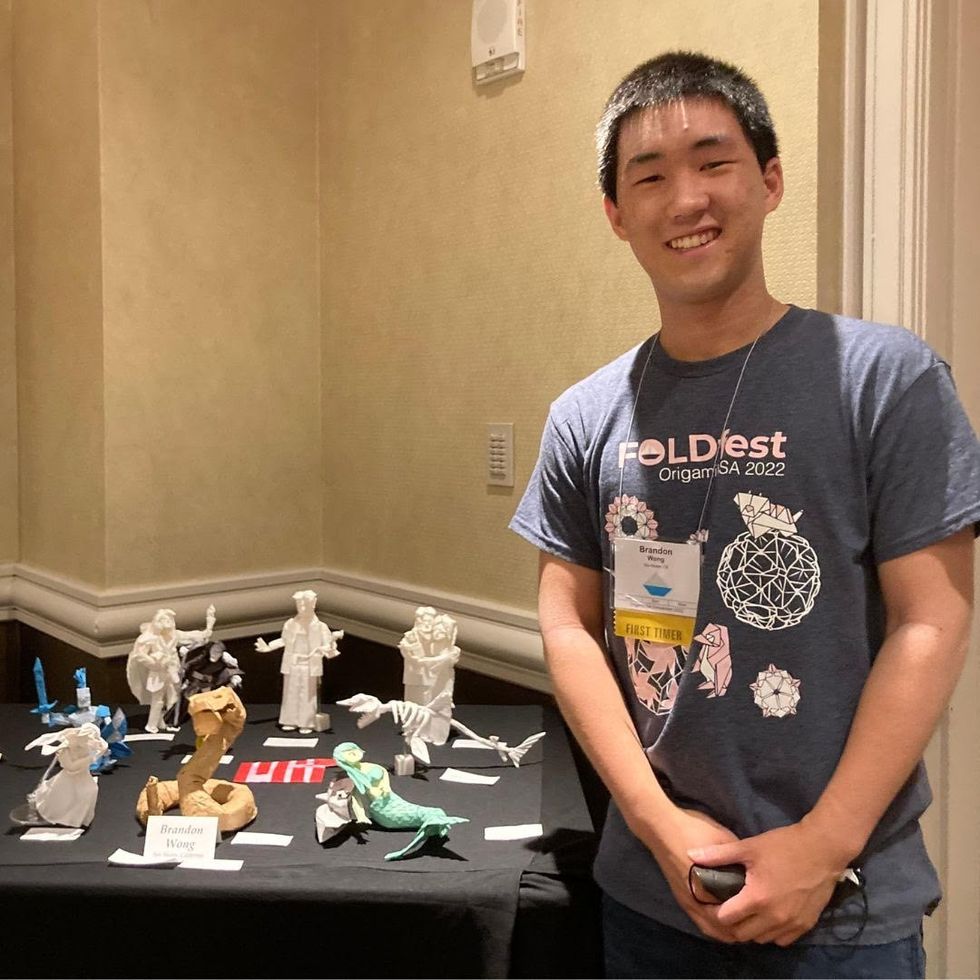
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Scientists Attempt to Make Human Cells Resistant to Coronaviruses and Ebola
Scientists are experimenting with turning certain genes on and off to make cells better fight viral infection.
Under the electronic microscope, the Ebola particles looked like tiny round bubbles floating inside human cells. Except these Ebola particles couldn't get free from their confinement.
They were trapped inside their bubbles, unable to release their RNA into the human cells to start replicating. These cells stopped the Ebola infection. And they did it on their own, without any medications, albeit in a petri dish of immunologist Adam Lacy-Hulbert. He studies how cells fight infections at the Benaroya Research Institute in Seattle, Washington.
These weren't just any ordinary human cells. They had a specific gene turned on—namely CD74, which typically wouldn't be on. Lacy-Hulbert's team was experimenting with turning various genes on and off to see what made cells fight viral infections better. One particular form of the CD74 gene did the trick. Normally, the Ebola particles would use the cells' own proteases—enzymes that are often called "molecular scissors" because they slice proteins—to cut the bubbles open. But CD74 produced a protein that blocked the scissors from cutting the bubbles, leaving Ebola trapped.
"When that gene turns on, it makes the protein that interferes with Ebola replication," Lacy-Hulbert says. "The protein binds to those molecular scissors and stops them from working." Even better, the protein interfered with coronaviruses too, including SARS-CoV-2, as the team published in the journal Science.
This begs the question: If one can turn on cells' viral resistance in a lab, can this be done in a human body so we that we can better fight Ebola, coronaviruses and other viral scourges?
Recent research indeed shows that our ability to fight viral infections is written in our genes. Genetic variability is at least one reason why some coronavirus-infected people don't develop symptoms while others stay on ventilators for weeks—often due to the aberrant response of their immune system, which went on overdrive to kill the pathogen. But if cells activate certain genes early in the infection, they might successfully stop viruses from replicating before the immune system spirals out of control.
"If my father who is 70 years old tests positive, I would recommend he takes interferon as early as possible."
When we talk about fighting infections, we tend to think in terms of highly specialized immune system cells—B-cells that release antibodies and T-cells that stimulate inflammatory responses, says Lacy-Hulbert. But all other cells in the body have the ability to fight infections too via different means. When cells detect the presence of a pathogen, they release interferons—small protein molecules named so because they set off a genetic chain reaction that interferes with viral replication. These molecules work as alarm signals to other cells around them. The neighboring cells transduce these signals inside themselves and turn on genes responsible for cellular defenses.
"There are at least 300 to 400 genes that are stimulated by type I interferons," says professor Jean-Laurent Casanova at Rockefeller University.
Scientists don't yet know exactly what all of these genes do, but they change the molecular behavior of the cells. "The cells go into a dramatic change and start producing hundreds of proteins that interfere with viral replication on the inside," explains Qian Zhang, a researcher at Casanova's lab. "Some block the proteins the virus needs and some physically tether the virus."
Some cells produce only small amount of interferon, enough to alert their neighbors. Others, such microphages and monocytes, whose jobs are to detect foreign invaders, produce a lot, injecting interferons into the blood to sound the alarm throughout the body. "They are professional cells so their jobs [are] to detect a viral or bacterial infection," Zhang explains.
People with impaired interferon responses are more vulnerable to infections, including influenza and coronaviruses. In two recent studies published in the journal Science, Casanova, Zhang and their colleagues found that patients who lacked a certain type of interferon had more severe Covid-19 symptoms and some died from it. The team ran a genetic comparison of blood samples from patients hospitalized with severe coronavirus cases against those with the asymptomatic infections.
They found that people with severe disease had rare variants in the 13 genes responsible for interferon production. More than three percent of them had a genetic mutation resulting in non-functioning genes. And over ten percent had an autoimmune condition, in which misguided antibodies neutralized their interferons, dampening their bodies' defenses—and these patients were predominantly men. These discoveries help explain why some young and seemingly healthy individuals require life support, while others have mild symptoms or none. The findings also offer ways of stimulating cellular resistance.
A New Frontier in the Making
The idea of making human cells genetically resistant to infections—and possibly other stressors like cancer or aging—has been considered before. It is the concept behind the Genome Project-write or GP-write project, which aims to create "ultra-safe" versions of human cells that resist a variety of pathogens by way of "recoding" or rewriting the cells' genes.
To build proteins, cells use combinations of three DNA bases called codons to represent amino acids—the proteins' building blocks. But biologists find that many of the codons are redundant so if they were removed from all genes, the human cells would still make all their proteins. However, the viruses, whose genes would still include these eliminated redundant codons, would no longer successfully be able to replicate inside human cells.
In 2016, the GP-Write team successfully reduced the number of Escherichia coli's codons from 64 to 57. Recoding genes in all human cells would be harder, but some recoded cells may be transplanted into the body, says Harvard Medical School geneticist George Church, the GP-Write core founding member.
"You can recode a subset of the body, such as all of your blood," he says. "You can also grow an organ inside a recoded pig and transplant it."
Church adds that these methods are still in stages that are too early to help us with this pandemic.
LeapsMag exclusively interviewed Church in 2019 about his latest progress with DNA recoding:
The Push for Clinical Trials
In the meantime, interferons may prove an easier medicine. Lacy-Hulbert thinks that interferon gamma might play a role in activating the CD74 gene, which gums up the molecular scissors. There also may be other ways to activate that gene. "So we are now thinking, can we develop a drug that mimics that actual activity?" he says.
Some interferons are already manufactured and used for treating certain diseases, including multiple sclerosis. Theoretically, nothing prevents doctors from prescribing interferons to Covid patients, but it must be done in the early stages of infection—to stimulate genes that trigger cellular defenses before the virus invades too many cells and before the immune systems mobilizes its big guns.
"If my father who is 70 years old tests positive, I would recommend he takes interferon as early as possible," says Zhang. But to make it a mainstream practice, doctors need clear prescription guidelines. "What would really help doctors make these decisions is clinical trials," says Casanova, so that such guidelines can be established. "We are now starting to push for clinical trials," he adds.
Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.
Thousands of Vaccine Volunteers Got a Dummy Shot. Should They Get the Real Deal Now?
If a treatment or prevention is known to work, it is considered unethical to withhold it from volunteers in order to prolong a research trial, experts say.
The highly anticipated rollout of a COVID-19 vaccine poses ethical considerations: When will trial volunteers who got a placebo be vaccinated? And how will this affect the data in those trials?
It's an issue that vaccine manufacturers and study investigators are wrestling with as the Food and Drug Administration is expected to grant emergency use authorization this weekend to a vaccine developed by Pfizer and the German company BioNTech. Another vaccine, produced by Moderna, is nearing approval in the United States.
The most vulnerable—health care workers and nursing home residents—are deemed eligible to receive the initial limited supply in accordance with priority recommendations from the Centers for Disease Control and Prevention (CDC).
With health care workers constituting an estimated 20 percent of trial participants, this question also comes to the fore: "Is it now ethically imperative that we offer them the vaccine, those who have had placebo?" says William Schaffner, an infectious diseases physician at Vanderbilt University and an adviser to the CDC's immunization practices committee.
When a "gold-standard" measure becomes available, participants in the placebo group "would ordinarily be notified" of the strong public health recommendation to opt for immunization, says Johan Bester, interim assistant dean for biomedical science education and director of bioethics at the University of Nevada, Las Vegas School of Medicine.
"If a treatment or prevention exists that we know works, it is unethical to withhold it from people who would benefit from it just to answer a research question." This moral principle poses a quandary for ethicists and physicians alike, as they ponder possible paths to proceed with vaccination amid ongoing trials. Rigorous trials are double-blinded—neither the participants nor the investigators know who received the actual vaccine and who got a dummy injection.
"The intent of these trials is to follow these folks for up to two years," says Marci Drees, infection prevention officer and hospital epidemiologist for ChristianaCare in Wilmington, Delaware. At a minimum, she adds, researchers would prefer to monitor participants for six months.
"You can still follow safety over a long-term period of time without actually continuing to have a placebo group for comparison."
But in the midst of a pandemic, that may not be feasible. Prolonged exposure to the highly contagious and lethal virus could have dire consequences.
To avoid compromising the integrity of the blinded data, "there are some potentially creative solutions," Drees says. For instance, trial participants could receive the opposite of what they initially got, whether it was the vaccine or the placebo.
One factor in this decision-making process depends on when a particular trial is slated to conclude. If that time is approaching, the risk of waiting would be lower than if the trial is only halfway in progress, says Eric Lofgren, an epidemiologist at Washington State University who has studied the impact of COVID-19 in jails and at in-person sporting events.
Sometimes a study concludes earlier than the projected completion date. "All clinical trials have a data and safety monitoring board that reviews the interim results," Lofgren says. The board may halt a trial after finding evidence of harm, or when a treatment or vaccine has proven to be "sufficiently good," rendering it unethical to deprive the placebo group of its benefits.
The initial months of a trial are most crucial for assessing a vaccine's safety. Differences between the trial groups would be illuminating if fewer individuals who got the active vaccine contracted the virus and developed symptoms when compared to the placebo recipients. After that point, in vaccine-administered participants, "you can still follow safety over a long-term period of time without actually continuing to have a placebo group for comparison," says Dial Hewlett Jr., medical director for disease control at the Westchester County Department of Health in New York.
Even outside of a trial, safety is paramount and any severe side effects that occur will be closely monitored and investigated through national reporting networks. For example, regulators in the U.K. are investigating several rare but serious allergic reactions to the Pfizer vaccine given on Tuesday. The FDA has asked Pfizer to track allergic reactions in its safety monitoring plan, and some experts are proposing that Pfizer conduct a separate study of the vaccine on people with a history of severe allergies.
As the FDA eventually grants authorization to multiple vaccines, more participants are likely to leave trials and opt to be vaccinated. It is important that enough participants choose to stay in ongoing trials, says Nicole Hassoun, professor of philosophy at the State University of New York at Binghamton, where she directs the Global Health Impact program to extend medical access to the poor.
She's hopeful that younger participants and individuals without underlying medical conditions will make that determination. But the departure of too many participants at high risk for the virus would make it more difficult to evaluate the vaccine's safety and efficacy in those populations, Hassoun says, while acknowledging, "We can't have the best of both worlds."
Once a safe and effective vaccine is approved in the United States, "it would not be ethically appropriate to do placebo trials to test new vaccines."
One solution would entail allowing health care workers to exit a trial after a vaccine is approved, even though this would result in "a conundrum when the next group of people are brought forward to get the vaccine—whether they're people age 65 and older or they're essential workers, or whoever they are," says Vanderbilt physician Schaffner, who is a former board member of the Infectious Diseases Society of America. "All of a sudden, you'll have an erosion of the volunteers who are in the trial."
For now, one way or another, experts agree that current and subsequent trials should proceed. There is a compelling reason to identify additional vaccines with potentially greater effectiveness but with fewer side effects or less complex delivery methods that don't require storage at extremely low temperatures.
"Continuing with existing vaccine trials and starting others remains important," says Nir Eyal, professor and director of Rutgers University's Center for Population-Level Bioethics in New Brunswick, New Jersey. "We still need to tell how much proven vaccines block infections and how long their duration lasts. And populations around the world need vaccines that are easier to store and deliver, or simply cheaper."
But once a safe and effective vaccine is approved in the United States, "it would not be ethically appropriate to do placebo trials to test new vaccines," says bioethicist Bester at the University of Nevada, Las Vegas School of Medicine. "One possibility if a new vaccine emerges, is to test it against existing vaccines."
In a letter sent to trial volunteers in November, Pfizer and BioNTech committed to establishing "a process that would allow interested participants in the placebo group who meet the eligibility criteria for early access in their country to 'cross-over' to the vaccine group." The trial plans to continue monitoring all subjects regardless of whether people in the placebo group cross over, Pfizer said in a presentation to the FDA today. After Pfizer has collected six months of safety data, in April 2021, it plans to ask the FDA for full approval of the vaccine.
In the meantime, the company pledged to update volunteers as they obtain more input from regulatory authorities. "Thank you again for making a difference by being a part of this study," they wrote. "It is only through the efforts of volunteers like you that reaching this important milestone and developing a potential vaccine against COVID-19 is possible."
CORRECTION: An earlier version of this article mistakenly stated that the FDA would be granting emergency "approval" to the Pfizer/BioNTech vaccine, rather than "emergency use authorization." We regret the error.

