A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
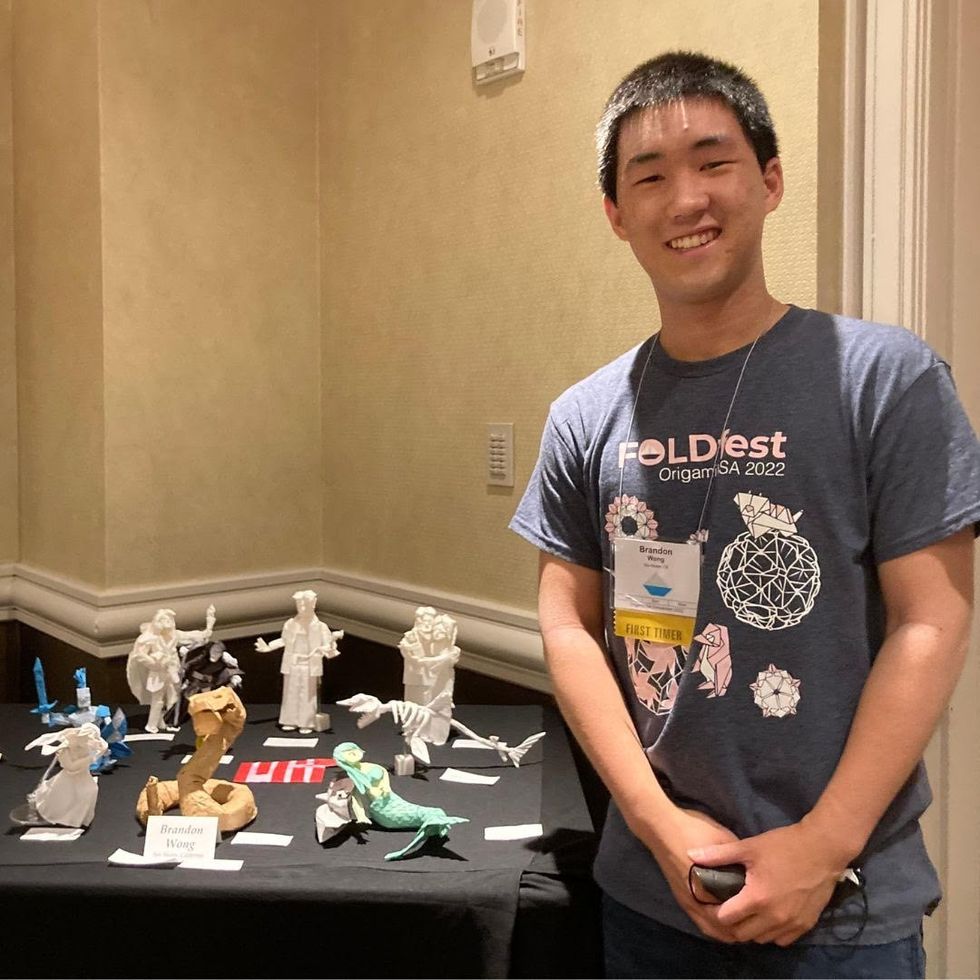
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Due to federal regulations, access to abortion medications is restricted, despite their record of safety and efficacy.
A few days before Christmas 2015, Paige Alexandria, a 28-year-old counselor at the Austin Women's Health Center in Texas, found out she was pregnant.
Alexandria had missed the cutoff for a medication abortion by three days.
"It was an unplanned pregnancy, and instantaneously I knew I needed an abortion," Alexandria recalls. Already a mother of two children, one with special needs, a third child was not something Alexandria and her husband felt prepared to take on. "Mentally, I knew my limit. I wasn't prepared for a third and I didn't want one," she says.
At an ultrasound appointment one week later, scans showed she was a little over eight weeks pregnant. Alexandria opted to have an abortion as soon as possible, and preferably with medication. "I really wanted to avoid a surgical abortion," she says. "It sounded a lot more invasive, and I'm already uncomfortable with pap smears and pelvic exams, so I initially went in wanting to do the pill."
But at the time, medication guidelines stipulated that one of the pills, called Mifepristone, could only be prescribed to end a pregnancy at eight weeks gestation or earlier – Alexandria had missed the cutoff by three days. If she wanted to end the pregnancy, she would need to undergo a surgical abortion, otherwise known as a vacuum aspiration abortion.
With a vacuum aspiration abortion, doctors dilate the cervix and manually aspirate out the contents of the uterus. Medication abortion, on the other hand, consists of the patient taking two pills – Mifepristone, which blocks the hormones that help the pregnancy develop, and Misoprostol, which empties the uterus over a period of days, identical to a miscarriage.
Alexandria was upset about the change of plans but resolute in her decision to end the pregnancy. "The fact that I didn't really have a choice in how my procedure was performed has made the experience just a little more sensitive for me," she says. She scheduled the earliest available appointment for a surgical abortion.

Paige Alexandria would have chosen to terminate her pregnancy with medication if the regulations were less stringent.
(Photo courtesy of Alexandria)
Like Alexandria, many people looking to terminate a pregnancy opt to do so with medication. According to research from the Guttmacher Institute, medication abortions accounted for nearly 40 percent of all abortions in the year 2017 – a marked increase from 2001, when medication abortions only accounted for roughly five percent of terminations. Taken 24-48 hours apart, Mifepristone and Misoprostol have a 95-99 percent success rate in terminating pregnancies up to 63 days – or nine weeks – of gestation, according to the American College of Obstetrics and Gynecology (ACOG).
But even though the World Health Organization (WHO) considers medical abortion to be highly safe and effective, the medication is still carefully guarded in the United States: Mifepristone is only available for terminating pregnancies up to 10 weeks gestation, per the FDA, even though limited research suggests that both are safe and effective at terminating pregnancies between 12 and 20 weeks.
Additionally, a separate set of regulations known as a Risk Evaluation and Mitigation Strategy (REMS) means that patients can only take Mifepristone under specific circumstances. Mifepristone must be distributed in person by a healthcare provider – usually interpreted in most states as a doctor or nurse practitioner – who has registered with the drug's manufacturer. The medication cannot be distributed through a pharmacy, so doctors who wish to provide the drug must stock the medication in-office, and both the provider and the patient must sign a form that warns them of the "risk of serious complications associated with Mifepristone," according to the FDA.
"REMS is a set of restrictions that the FDA puts on the distribution of drugs it considers dangerous or risky in some way," says Dr. Elizabeth Raymond, an OB-GYN and senior medical associate at Gynuity Health Projects. Although not always called REMS, these restrictions have been imposed on Mifepristone since the medication was approved by the FDA in 2000, Raymond says.
Raymond is part of a growing number of physicians and researchers who want to eliminate the REMS requirements for Mifepristone, also known by its brand name Mifeprex. In 2017, Raymond and several other physicians authored a paper in the New England Journal of Medicine (NEJM) arguing that Mifepristone is extremely safe and needlessly over-regulated.
"When the FDA first approved [Mifepristone] and imposed these requirements, they might have made sense 19 years ago when there was limited information about the use of this treatment in the United States," says Dr. Daniel Grossman, director at Advancing New Standards in Reproductive Health at UCSF and co-author of the 2017 report in the NEJM. "Now, after 19 years, it's clear that this medication is very safe, and safer than a lot of others available in a pharmacy."
Since 2000, Mifepristone has been implicated in 19 deaths, making its mortality rate 0.00063 percent.
According to their research, over three million people have taken Mifepristone since it was approved in 2000. Since then, Mifepristone has been implicated in 19 deaths, making its mortality rate 0.00063 percent. Even then, the risk is inflated, Grossman says.
"The requirement is that practitioners need to report any deaths that occur after taking these medications, and so you'll see deaths included in that figure which are homicides or suicides or something unrelated to taking Mifepristone," says Grossman. In contrast, Acetaminophen – better known as Tylenol – was associated with 458 overdose deaths between 1990 and 1998, as well as 56,000 emergency room visits and 26,000 hospitalizations. Sildenafil, better known as Viagra, was linked to 762 deaths in the first twenty months after it was approved by the FDA. Yet neither Tylenol nor Viagra have been burdened with the same REMS restrictions as Mifepristone.
"It's clearly about more than just the safety of the medication at this point," says Grossman. "It's more about stigma related to abortion and politics."
For people who want a medication abortion, the REMS requirements mean they often need to take off work to schedule a doctor's appointment, arrange for transportation and childcare, and then arrange an additional doctor's appointment days afterward to take the second dose of medication. While surgical abortion procedures are quicker (usually a one-day outpatient procedure, depending on gestation), many people prefer having the abortion in the comfort of their home or surrounded by family instead.
Paige Alexandria, who counsels people seeking abortions at her job, says that survivors of sexual violence often prefer medical abortions to surgical ones. "A lot of time survivors have a trauma associated with medical instruments or having pelvic exams, and so they're more comfortable taking a pill," she says.
But REMS also creates a barrier for healthcare providers, Grossman says. Stocking the medication in-office is "a hassle" and "expensive," while others are reluctant to register their name with the drug manufacturer, fearing harassment or violence from anti-choice protestors. As a result, the number of practitioners willing to provide medical abortions nationwide is severely limited. According to Grossman's own research published in the journal Obstetrics and Gynecology, 28 percent of OBGYNs admitted they would administer medication abortions if it were possible to write a prescription for Mifepristone rather than stock it in-office.
Amazingly, the restrictions on Mifepristone have loosened since it first came on the market. In 2016, the FDA updated the guidelines on Mifepristone to allow its use until 10 weeks gestation, up from eight weeks. But doctors say the REMS restrictions should be eliminated completely so that people can obtain abortions as early as possible.
"REMS restrictions inhibit people from being able to get a timely abortion," says Raymond, who stresses that abortion is generally more comfortable, more affordable, and safer for women the earlier it's done. "Abortion is very safe no matter when you get it, but it's also easier because there's less risk for bleeding, infections, or other complications," Raymond says. Abortions that occur earlier than eight weeks of gestation have a complication rate of less than one percent, while an abortion done at 12 or 13 weeks has a three to six percent chance of complications.
And even for people who want a medication abortion early on in their pregnancy, REMS restrictions make it so that they may not have time to obtain it before the 10-week period lapses, Raymond says.
"If you're seven weeks pregnant but it takes you three weeks to figure out travel and childcare arrangements to go into the doctor and take this medication, now you're at the cutoff date," she says. "Even if you manage to get an abortion at nine weeks, that's still a later gestational age, and so the risks are increased."
In 2016, at a little over nine weeks gestation, Alexandria completed her abortion by having a D&E. But because she didn't have anyone to drive her home after the procedure, she wasn't able to have sedation throughout, something she describes as "traumatic."
"I had the abortion completely aware and coherent, and paired with the fact that I hadn't even wanted a surgical abortion in the first place made it harder to deal with," Alexandria says.
"When you're just a day or two past eight weeks and you want an abortion – why is medication not immediately available?"
Today, Alexandria shares her story publicly to advocate for abortion care. Although she doesn't regret her surgical abortion and acknowledges that not everyone experiences surgical abortion the same way she did, she does wish that she could have gone a different route.
"If I had to do it over, I would still try to do the pill, because [the surgical abortion] was such a terrifying experience," she says. "When you're just a day or two past eight weeks and you want an abortion – why is medication not immediately available? It just doesn't make sense."
How Scientists Are Engineering Plastic-Eating Bacteria to Fight the Pollution Crisis
Scientists are turning to synthetic biology to engineer bacteria that can degrade plastic and turn it into higher-value materials.
[Ed. Note: This is the second episode in our Moonshot series, which will explore four cutting-edge scientific developments that stand to fundamentally transform our world.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

