A skin patch to treat peanut allergies teaches the body to tolerate the nuts

Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
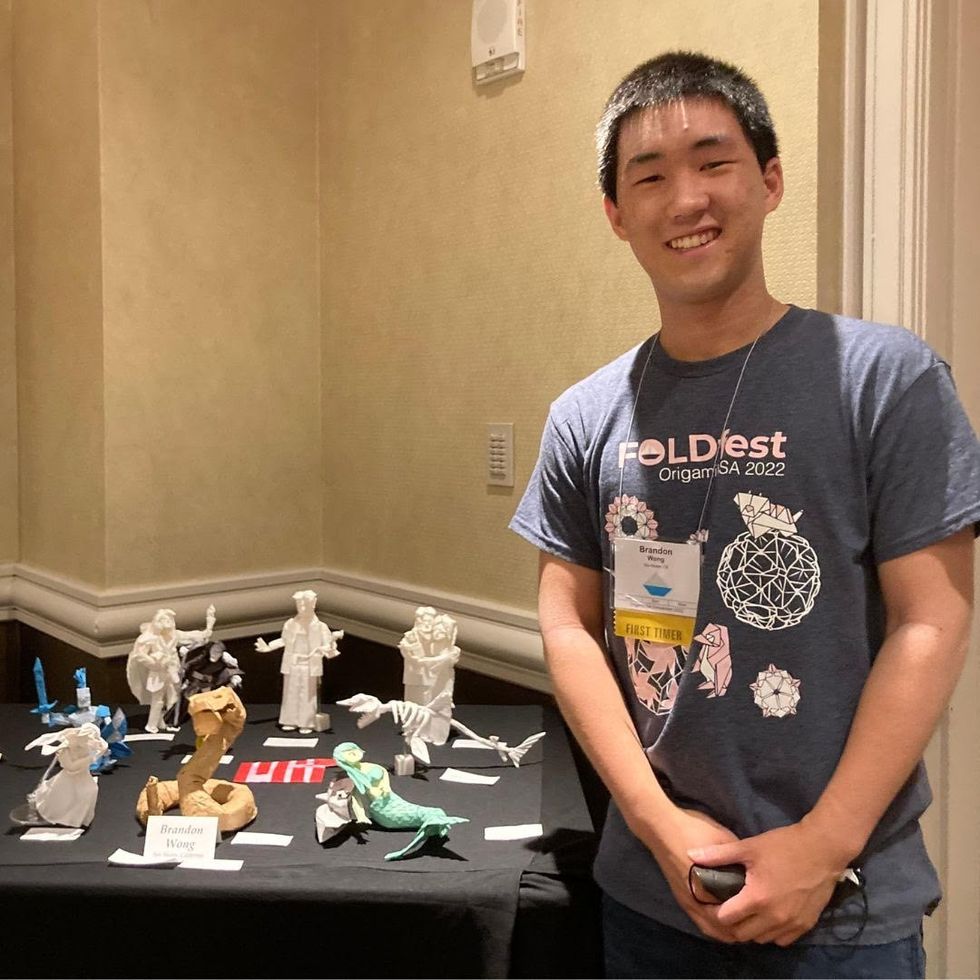
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”
Podcast: The Friday Five - your health research roundup
The Friday Five is a new series in which Leaps.org covers five breakthroughs in research over the previous week that you may have missed.
The Friday Five is a new podcast series in which Leaps.org covers five breakthroughs in research over the previous week that you may have missed. There are plenty of controversies and ethical issues in science – and we get into many of them in our online magazine – but there’s also plenty to be excited about, and this news roundup is focused on inspiring scientific work to give you some momentum headed into the weekend.
Covered in this week's Friday Five:
- Puffer fish chemical for treating chronic pain
- Sleep study on the health benefits of waking up multiples times per night
- Best exercise regimens for reducing the risk of mortality aka living longer
- AI breakthrough in mapping protein structures with DeepMind
- Ultrasound stickers to see inside your body
CandyCodes could provide sweet justice against fake pills
A bioengineer at the University of California, Riverside, may have found a way to prevent counterfeit medications: pill coatings inspired by the sprinkles on baked goods and candies.
When we swallow a pill, we hope it will work without side effects. Few of us know to worry about a growing issue facing the pharmaceutical industry: counterfeit medications. These pills, patches, and other medical products might look just like the real thing. But they’re often stuffed with fillers that dilute the medication’s potency or they’re simply substituted for lookalikes that contain none of the prescribed medication at all.
Now, bioengineer William Grover at the University of California, Riverside, may have a solution. Inspired by the tiny, multi-colored sprinkles called nonpareils that decorate baked goods and candies, Grover created CandyCodes pill coatings to prevent counterfeits.
The idea was borne out of pandemic boredom. Confined to his home, Grover was struck by the patterns of nonpareils he saw on candies, and found himself counting the number of little balls on each one. “It’s random, how they’re applied,” he says. “I wondered if it ever repeats itself or if each of these candies is unique in the entire world.” He suspected the latter, and some quick math proved his hypothesis: Given dozens of nonpareils per candy in a handful of different colors, it’s highly unlikely that the sprinklings on any two candies would be identical.
He quickly realized his finding could have practical applications: pills or capsules could be coated with similar “sprinkles,” with the manufacturer photographing each pill or capsule before selling its products. Consumers looking to weed out fakes could potentially take a photo with their cell phones and go online to compare images of their own pills to the manufacturer’s database, with the help of an algorithm that would determine their authenticity. Or, a computer could generate another type of unique identifier, such as a text-based code, tracking to the color and location of the sprinkles. This would allow for a speedier validation than a photo-based comparison, Grover says. “It could be done very quickly, in a fraction of a second.”
Researchers and manufacturers have already developed some anti-counterfeit tools, including built-in identifiers like edible papers with scannable QR codes. But such methods, while functional, can be costly to implement, Grover says.
It wouldn’t be paranoid to take such precautions. Counterfeits are a growing problem, according to Young Kim, a biomedical engineer at Purdue University who was not involved in the CandyCodes study. “There are approximately 40,000 online pharmacies that one can access via the Internet,” he says. “Only three to four percent of them are operated legally.” Purchases from online pharmacies rose dramatically during the pandemic, and Kim expects a boom in counterfeit medical products alongside it.
The FDA warns that U.S. consumers can be exposed to counterfeits through online purchases, in particular. The problem is magnified in low- to middle-income nations, where one in 10 medical products are counterfeit, according to a World Health Organization estimate. Cost doesn’t seem to be a factor, either; antimalarials and antibiotics are most often reported as counterfeits or fakes, and generic medications are swapped as often as brand-name drugs, according to the same WHO report.
Counterfeits weren’t tracked globally until 2013; since then, there have been 1,500 reports to the WHO, with actual incidences of counterfeiting likely much higher. Fake medicines have been estimated to result in costs of $200 billion each year, and are blamed for more than 72,000 pneumonia- and 116,000 malaria-related deaths.
Researchers and manufacturers have already developed some anti-counterfeit tools, including built-in identifiers like edible papers with scannable QR codes or barcodes that are stamped onto or otherwise incorporated into pills and other medical products. But such methods, while functional, can be costly to implement, Grover says.

CandyCodes could provide unique identifiers for at least 41 million pills for every person on the planet.
William Grover
“Putting universal codes on each pill and each dosage is attractive,” he says. “The challenge is, how can we do it in a way that requires as little modification to the existing manufacturing process as possible? That's where I hope CandyCodes have an edge. It's not zero modification, but I hope it is as minor a modification of the manufacturing process as possible.”
Kim calls the concept “a clever idea to introduce entropy for high-level security” even if it may not be as close to market as other emerging technologies, including some edible watermarks he’s helped develop. He points out that CandyCodes still needs to be tested for reproducibility and readability.
The possibilities are already intriguing, though. Grover’s recent research, published in Scientific Reports, predicts that unique codes could be used for at least 41 million pills for every person on the planet.
Sadly, CandyCodes’ multicolored bits probably won’t taste like candy. They must be made of non-caloric ingredients to meet the international regulatory standards that govern food dyes and colorants. But Grover hopes CandyCodes represent a simple, accessible solution to a heart-wrenching issue. “This feels like trying to track down and go after bad guys,” he says. “Someone who would pass off a medicine intended for a child or a sick person and pass it off as something effective, I can't imagine anything much more evil than that. It's fun and, and a little fulfilling to try to develop technologies that chip away at that.”

