Interview with Jamie Metzl: We need a global OS upgrade

Jamie Metzl, author of Hacking Darwin, shares his views with Leaps.org on the future of genetics, tech, healthcare and more.
In this Q&A, leading technology and healthcare futurist Jamie Metzl discusses a range of topics and trend lines that will unfold over the next several decades: whether a version of Moore's Law applies to genetic technologies, the ethics of genetic engineering, the dangers of gene hacking, the end of sex, and much more.
Metzl is a member of the WHO expert advisory committee on human genome editing and the bestselling author of Hacking Darwin.
The conversation was lightly edited by Leaps.org for style and length.
In Hacking Darwin, you describe how we may modify the human body with CRISPR technologies, initially to obtain unsurpassed sports performance and then to enhance other human characteristics. What would such power over human biology mean for the future of our civilization?
After nearly four billion years of evolution, our one species suddenly has the increasing ability to read, write, and hack the code of life. This will have massive implications across the board, including in human health and reproduction, plant and animal agriculture, energy and advanced materials, and data storage and computing, just to name a few. My book Hacking Darwin: Genetic Engineering and the Future of Humanity primarly explored how we are currently deploying and will increasingly use our capabilities to transform human life in novel ways. My next book, The Great Biohack: Recasting Life in an Age of Revolutionary Technology, coming out in May 2024, will examine the broader implications for all of life on Earth.
We humans will, over time, use these technologies on ourselves to solve problems and eventually to enhance our capabilities. We need to be extremely conservative, cautious, and careful in doing so, but doing so will almost certainly be part of our future as a species.
In electronics, Moore's law is an established theory that computing power doubles every 18 months. Is there any parallel to be drawn with genetic technologies?
The increase in speed and decrease in costs of genome sequencing have progressed far faster than Moore’s law. It took thirteen years and cost about a billion dollars to sequence the first human genome. Today it takes just a few hours and can cost as little as a hundred dollars to do a far better job. In 2012, Jennifer Doudna and Emmanuel Charpentier published the basic science paper outlining the CRISPR-cas9 genome editing tool that would eventually win them the Nobel prize. Only six years later, the first CRISPR babies were born in China. If it feels like technology is moving ever-faster, that’s because it is.
Let's turn to the topic of aging. Do you think that the field of genetics will advance fast enough to eventually increase maximal lifespan for a child born this year? How about for a person who is currently age 50?
The science of aging is definitely real, but that doesn’t mean we will live forever. Aging is a biological process subject to human manipulation. Decades of animal research shows that. This does not mean we will live forever, but it does me we will be able to do more to expand our healthspans, the period of our lives where we are able to live most vigorously.
The first thing we need to do is make sure everyone on earth has access to the resources necessary to live up to their potential. I live in New York City, and I can take a ten minute subway ride to a neighborhood where the average lifespan is over a decade shorter than in mine. This is true within societies and between countries as well. Secondly, we all can live more like people in the Blue Zones, parts of the world where people live longer, on average, than the rest of us. They get regular exercise, eat healthy foods, have strong social connections, etc. Finally, we will all benefit, over time, from more scientific interventions to extend our healthspan. This may include small molecule drugs like metformin, rapamycin, and NAD+ boosters, blood serum infusions, and many other things.
Science fiction has depicted a future where we will never get sick again, stay young longer or become immortal. Assuming that any of this is remotely possible, should we be afraid of such changes, even if they seem positive in some regards, because we can’t understand the full implications at this point?
Not all of these promises will be realized in full, but we will use these technologies to help us live healthier, longer lives. We will never become immortal becasue nothing lasts forever. We will always get sick, even if the balance of diseases we face shifts over time, as it has always done. It is healthy, and absolutely necessary, that we feel both hope and fear about this future. If we only feel hope, we will blind ourselves to the very real potential downsides. If we only feel fear, we will deny ourselves the very meaningful benefits these technologies have the potential to provide.
A fascinating chapter in Hacking Darwin is entitled The End of Sex. And you see that as a good thing?
We humans will always be a sexually reproducing species, it’s just that we’ll reproduce increasingly less through the physical act of sex. We’re already seeing this with IVF. As the benefits of technology assisted reproduction increase relative to reproduction through the act of sex, many people will come to see assisted reproduction as a better way to reduce risk and, over time, possibly increase benefits. We’ll still have sex for all the other wonderful reasons we have it today, just less for reproduction. There will always be a critical place in our world for Italian romantics!
What are dangers of genetic hackers, perhaps especially if everyone’s DNA is eventually transcribed for medical purposes and available on the internet and in the cloud?
The sky is really the limit for how we can use gentic technologies to do things we may want, and the sky is also the limit for potential harms. It’s quite easy to imagine scenarios in which malevolent actors create synthetic pathogens designed to wreak havoc, or where people steal and abuse other people’s genetic information. It wouldn’t even need to be malevolent actors. Even well-intentioned researchers making unintended mistakes could cause real harm, as we may have seen with COVID-19 if, as appears likely to me, the pandemic stems for a research related incident]. That’s why we need strong governance and regulatory systems to optimize benefits and minimize potential harms. I was honored to have served on the World Health Organization Expert Advisory Committee on Human Genome Editing, were we developed a proposed framework for how this might best be achieved.
You foresee the equivalent of a genetic arms race between the world's most powerful countries. In what sense are genetic technologies similar to weapons?
Genetic technologies could be used to create incredibly powerful bioweapons or to build gene drives with the potential to crash entire ecosystems. That’s why thoughtful regulation is in order. Because the benefits of mastering and deploying these technologies are so great, there’s also a real danger of a genetics arms race. This could be extremely dangerous and will need to be prevented.
In your book, you express concern that states lacking Western conceptions of human rights are especially prone to misusing the science of genetics. Does this same concern apply to private companies? How much can we trust them to control and wield these technologies?
This is a conversation about science and technology but it’s really a conversation about values. If we don’t agree on what core values should be promoted, it will be nearly impossible to agree on what actions do and do not make sense. We need norms, laws, and values frameworks that apply to everyone, including governments, corporations, researchers, healthcare providers, DiY bio hobbyists, and everyone else.
We have co-evolved with our technology for a very long time. Many of our deepest beliefs have formed in that context and will continue to do so. But as we take for ourselves the powers we have attributed to our various gods, many of these beliefs will be challenged. We can not and must not jettison our beliefs in the face of technology, and must instead make sure our most cherished values guide the application of our most powerful technologies.
A conversation on international norms is in full swing in the field of AI, prompted by the release of ChatGPT4 earlier this year. Are there ways in which it’s inefficient, shortsighted or otherwise problematic for these discussions on gene technologies, AI and other advances to be occurring in silos? In addition to more specific guidelines, is there something to be gained from developing a universal set of norms and values that applies more broadly to all innovation?
AI is yet another technology where the potential to do great good is tied to the potential to inflict signifcant harm. It makes no sense that we tend to treat each technology on its own rather than looking at the entire category of challenges. For sure, we need to very rapidly ramp up our efforts with regard to AI norm-setting, regulations, and governance at all levels. But just doing that will be kind of like generating a flu vaccine for each individual flu strain. Far better to build a universal flu vaccine addressing common elements of all flu viruses of concern.
That’s why we also need to be far more deliberate in both building a global operating systems based around the mutual responsibilities of our global interdependence and, under that umbrella, a broader system for helping us govern and regulate revolutionary technologies. Such a process might begin with a large international conference, the equivalent of Rio 1992 for climate change, but then quickly work to establish and share best practices, help build parallel institutions in all countries so people and governamts can talk with each other, and do everything possible to maximize benefits and minimize risks at all levels in an ongoing and dynamic way.
At what point might genetic enhancements lead to a reclassfication of modified humans as another species?
We’ll still all be fellow humans for a very, very long time. We already have lots of variation between us. That is the essence of biology. Will some humans, at some point in the future, leave Earth and spend generations elsewhere? I believe so. In those new environments, humans will evolve, over time, differently than those if us who remain on this planet? This may sound like science fiction, but the sci-fi future is coming at us faster than most people realize.
Is the concept of human being changing?
Yes. It always has and always will.
Another big question raised in your book: what limits should we impose on the freedom to manipulate genetics?
Different societies will come to different conclusion on this critical question. I am sympathetic to the argument that people should have lots of say over their own bodies, which why I support abortion rights even though I recognize that an abortion can be a violent procedure. But it would be insane and self-defeating to say that individuals have an unlimited right to manipulate their own or their future children’s heritable genetics. The future of human life is all of our concern and must be regulated, albeit wisely.
In some cases, such as when we have the ability to prevent a deadly genetic disroder, it might be highly ethical to manipulate other human beings. In other circumstances, the genetic engineering of humans might be highly unethical. The key point is to avoid asking this question in a binary manner. We need to weigh the costs and benefits of each type of intervention. We need societal and global infrastrucutres to do that well. We don’t yet have those but we need them badly.
Can you tell us more about your next book?
The Great Biohack: Recasting Lifee in an Age of Revolutionary Technology, will come out in May 2024. It explores what the intersecting AI, genetics, and biotechnology revolutions will mean for the future of life on earth, including our healthcare, agriculture, industry, computing, and everything else. We are at a transitional moment for life on earth, equivalent to the dawn of agriculture, electricity, and industrialization. The key differentiator between better and worse outcomes is what we do today, at this early stage of this new transformation. The book describes what’s happening, what’s at stake, and what we each and all can and, frankly, must do to build the type of future we’d like to inhabit.
You’ve been a leader of international efforts calling for a full investigation into COVID-19 origins and are the founder of the global movement OneShared.World. What problem are you trying to solve through OneShared.World?
The biggest challenge we face today is the mismatch between the nature of our biggest problems, global and common, and the absence of a sufficient framework for addressing that entire category of challenges. The totally avoidable COVID-19 pandemic is one example of the extremet costs of the status quo. OneShared.World is our effort to fight for an upgrade in our world’s global operating system, based around the mutual responsibilities of interdependence. We’ve had global OS upgrades before after the Thirty Years War and after World War II, but wouldn’t it be better to make the necessary changes now to prevent a crisis of that level stemming from a nuclear war, ecosystem collapse, or deadlier synthetic biology pandemic rather than waiting until after? Revolutionary science is a global issue that must be wisely managed at every level if it is to be wisely managed at all.
How do we ensure that revolutionary technologies benefit humanity instead of undermining it?
That is the essential question. It’s why I’ve written Hacking Darwin, am writing The Great Biohack, and doing the rest of my work. If we want scietific revolutions to help, rather than hurt, us, we must all play a role building that future. This isn’t just a conversation about science, it’s about how we can draw on our most cherished values to guide the optimal development of science and technology for the common good. That must be everyone’s business.
Portions of this interview were first published in Grassia (Italy) and Zen Portugal.
Jamie Metzl is one of the world’s leading technology and healthcare futurists and author of the bestselling book, Hacking Darwin: Genetic Engineering and the Future of Humanity, which has been translated into 15 languages. In 2019, he was appointed to the World Health Organization expert advisory committee on human genome editing. Jamie is a faculty member of Singularity University and NextMed Health, a Senior Fellow of the Atlantic Council, and Founder and Chair of the global social movement, OneShared.World.
Called “the original COVID-19 whistleblower,” his pioneering role advocating for a full investigation into the origins of the COVID-19 pandemic has been featured in 60 Minutes, the New York Times, and most major media across the globe, and he was the lead witness in the first congressional hearings on this topic. Jamie previously served in the U.S. National Security Council, State Department, and Senate Foreign Relations Committee and with the United Nations in Cambodia. Jamie appears regularly on national and international media and his syndicated columns and other writing in science, technology, and global affairs are featured in publications around the world.
Jamie sits on advisory boards for multiple biotechnology and other companies and is Special Strategist to the WisdomTree BioRevolution Exchange Traded Fund. In addition to Hacking Darwin, he is author of a history of the Cambodian genocide, the historical novel The Depths of the Sea, and the genetics sci-fi thrillers Genesis Code and Eternal Sonata. His next book, The Great Biohack: Recasting Life in an age of Revolutionary Technology, will be published by Hachette in May 2024. Jamie holds a Ph.D. from Oxford, a law degree from Harvard, and an undergraduate degree from Brown and is an avid ironman triathlete and ultramarathon runner.
How the Human Brain Project Built a Mind of its Own
In 2013, the Human Brain Project set out to build a realistic computer model of the brain over ten years. Now, experts are reflecting on HBP's achievements with an eye toward the future.
In 2009, neuroscientist Henry Markram gave an ambitious TED talk. “Our mission is to build a detailed, realistic computer model of the human brain,” he said, naming three reasons for this unmatched feat of engineering. One was because understanding the human brain was essential to get along in society. Another was because experimenting on animal brains could only get scientists so far in understanding the human ones. Third, medicines for mental disorders weren’t good enough. “There are two billion people on the planet that are affected by mental disorders, and the drugs that are used today are largely empirical,” Markram said. “I think that we can come up with very concrete solutions on how to treat disorders.”
Markram's arguments were very persuasive. In 2013, the European Commission launched the Human Brain Project, or HBP, as part of its Future and Emerging Technologies program. Viewed as Europe’s chance to try to win the “brain race” between the U.S., China, Japan, and other countries, the project received about a billion euros in funding with the goal to simulate the entire human brain on a supercomputer, or in silico, by 2023.
Now, after 10 years of dedicated neuroscience research, the HBP is coming to an end. As its many critics warned, it did not manage to build an entire human brain in silico. Instead, it achieved a multifaceted array of different goals, some of them unexpected.
Scholars have found that the project did help advance neuroscience more than some detractors initially expected, specifically in the area of brain simulations and virtual models. Using an interdisciplinary approach of combining technology, such as AI and digital simulations, with neuroscience, the HBP worked to gain a deeper understanding of the human brain’s complicated structure and functions, which in some cases led to novel treatments for brain disorders. Lastly, through online platforms, the HBP spearheaded a previously unmatched level of global neuroscience collaborations.
Simulating a human brain stirs up controversy
Right from the start, the project was plagued with controversy and condemnation. One of its prominent critics was Yves Fregnac, a professor in cognitive science at the Polytechnic Institute of Paris and research director at the French National Centre for Scientific Research. Fregnac argued in numerous articles that the HBP was overfunded based on proposals with unrealistic goals. “This new way of over-selling scientific targets, deeply aligned with what modern society expects from mega-sciences in the broad sense (big investment, big return), has been observed on several occasions in different scientific sub-fields,” he wrote in one of his articles, “before invading the field of brain sciences and neuromarketing.”
"A human brain model can simulate an experiment a million times for many different conditions, but the actual human experiment can be performed only once or a few times," said Viktor Jirsa, a professor at Aix-Marseille University.
Responding to such critiques, the HBP worked to restructure the effort in its early days with new leadership, organization, and goals that were more flexible and attainable. “The HBP got a more versatile, pluralistic approach,” said Viktor Jirsa, a professor at Aix-Marseille University and one of the HBP lead scientists. He believes that these changes fixed at least some of HBP’s issues. “The project has been on a very productive and scientifically fruitful course since then.”
After restructuring, the HBP became a European hub on brain research, with hundreds of scientists joining its growing network. The HBP created projects focused on various brain topics, from consciousness to neurodegenerative diseases. HBP scientists worked on complex subjects, such as mapping out the brain, combining neuroscience and robotics, and experimenting with neuromorphic computing, a computational technique inspired by the human brain structure and function—to name just a few.
Simulations advance knowledge and treatment options
In 2013, it seemed that bringing neuroscience into a digital age would be farfetched, but research within the HBP has made this achievable. The virtual maps and simulations various HBP teams create through brain imaging data make it easier for neuroscientists to understand brain developments and functions. The teams publish these models on the HBP’s EBRAINS online platform—one of the first to offer access to such data to neuroscientists worldwide via an open-source online site. “This digital infrastructure is backed by high-performance computers, with large datasets and various computational tools,” said Lucy Xiaolu Wang, an assistant professor in the Resource Economics Department at the University of Massachusetts Amherst, who studies the economics of the HBP. That means it can be used in place of many different types of human experimentation.
Jirsa’s team is one of many within the project that works on virtual brain models and brain simulations. Compiling patient data, Jirsa and his team can create digital simulations of different brain activities—and repeat these experiments many times, which isn’t often possible in surgeries on real brains. “A human brain model can simulate an experiment a million times for many different conditions,” Jirsa explained, “but the actual human experiment can be performed only once or a few times.” Using simulations also saves scientists and doctors time and money when looking at ways to diagnose and treat patients with brain disorders.
Compiling patient data, scientists can create digital simulations of different brain activities—and repeat these experiments many times.
The Human Brain Project
Simulations can help scientists get a full picture that otherwise is unattainable. “Another benefit is data completion,” added Jirsa, “in which incomplete data can be complemented by the model. In clinical settings, we can often measure only certain brain areas, but when linked to the brain model, we can enlarge the range of accessible brain regions and make better diagnostic predictions.”
With time, Jirsa’s team was able to move into patient-specific simulations. “We advanced from generic brain models to the ability to use a specific patient’s brain data, from measurements like MRI and others, to create individualized predictive models and simulations,” Jirsa explained. He and his team are working on this personalization technique to treat patients with epilepsy. According to the World Health Organization, about 50 million people worldwide suffer from epilepsy, a disorder that causes recurring seizures. While some epilepsy causes are known others remain an enigma, and many are hard to treat. For some patients whose epilepsy doesn’t respond to medications, removing part of the brain where seizures occur may be the only option. Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
“We apply such personalized models…to precisely identify where in a patient’s brain seizures emerge,” Jirsa explained. “This guides individual surgery decisions for patients for which surgery is the only treatment option.” He credits the HBP for the opportunity to develop this novel approach. “The personalization of our epilepsy models was only made possible by the Human Brain Project, in which all the necessary tools have been developed. Without the HBP, the technology would not be in clinical trials today.”
Personalized simulations can significantly advance treatments, predict the outcome of specific medical procedures and optimize them before actually treating patients. Jirsa is watching this happen firsthand in his ongoing research. “Our technology for creating personalized brain models is now used in a large clinical trial for epilepsy, funded by the French state, where we collaborate with clinicians in hospitals,” he explained. “We have also founded a spinoff company called VB Tech (Virtual Brain Technologies) to commercialize our personalized brain model technology and make it available to all patients.”
The Human Brain Project created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own.
Other experts believe it’s too soon to tell whether brain simulations could change epilepsy treatments. “The life cycle of developing treatments applicable to patients often runs over a decade,” Wang stated. “It is still too early to draw a clear link between HBP’s various project areas with patient care.” However, she admits that some studies built on the HBP-collected knowledge are already showing promise. “Researchers have used neuroscientific atlases and computational tools to develop activity-specific stimulation programs that enabled paraplegic patients to move again in a small-size clinical trial,” Wang said. Another intriguing study looked at simulations of Alzheimer’s in the brain to understand how it evolves over time.
Some challenges remain hard to overcome even with computer simulations. “The major challenge has always been the parameter explosion, which means that many different model parameters can lead to the same result,” Jirsa explained. An example of this parameter explosion could be two different types of neurodegenerative conditions, such as Parkinson’s and Huntington’s diseases. Both afflict the same area of the brain, the basal ganglia, which can affect movement, but are caused by two different underlying mechanisms. “We face the same situation in the living brain, in which a large range of diverse mechanisms can produce the same behavior,” Jirsa said. The simulations still have to overcome the same challenge.
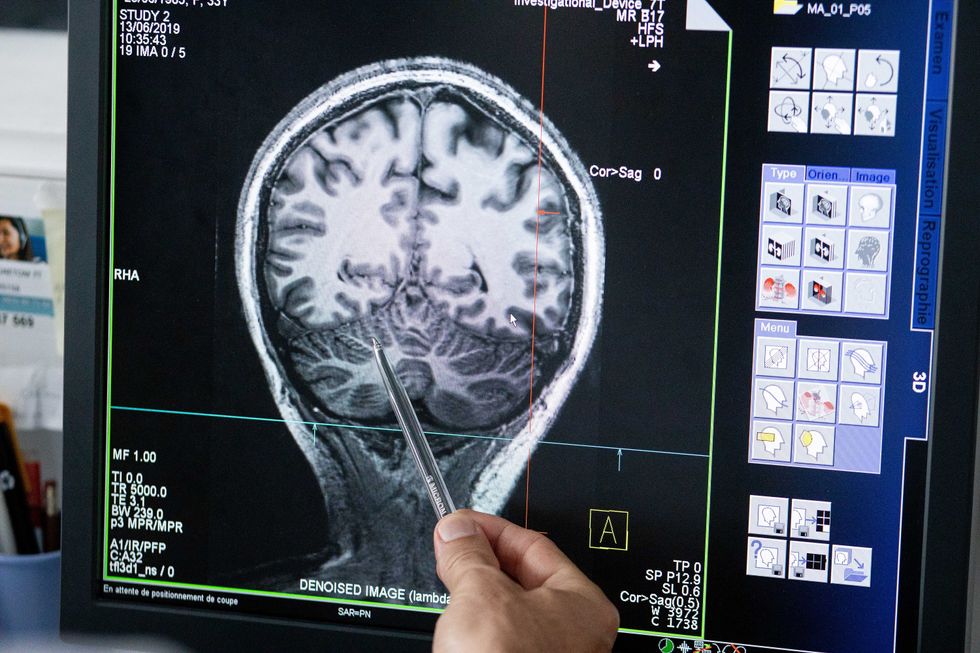
Understanding where in the patients’ brains seizures arise can give scientists a better idea of how to treat them and whether to use surgery versus medications.
The Human Brain Project
A network not unlike the brain’s own
Though the HBP will be closing this year, its legacy continues in various studies, spin-off companies, and its online platform, EBRAINS. “The HBP is one of the earliest brain initiatives in the world, and the 10-year long-term goal has united many researchers to collaborate on brain sciences with advanced computational tools,” Wang said. “Beyond the many research articles and projects collaborated on during the HBP, the online neuroscience research infrastructure EBRAINS will be left as a legacy even after the project ends.”
Those who worked within the HBP see the end of this project as the next step in neuroscience research. “Neuroscience has come closer to very meaningful applications through the systematic link with new digital technologies and collaborative work,” Jirsa stated. “In that way, the project really had a pioneering role.” It also created a level of interconnectedness within the neuroscience research community that never existed before—a network not unlike the brain’s own. “Interconnectedness is an important advance and prerequisite for progress,” Jirsa said. “The neuroscience community has in the past been rather fragmented and this has dramatically changed in recent years thanks to the Human Brain Project.”
According to its website, by 2023 HBP’s network counted over 500 scientists from over 123 institutions and 16 different countries, creating one of the largest multi-national research groups in the world. Even though the project hasn’t produced the in-silico brain as Markram envisioned it, the HBP created a communal mind with immense potential. “It has challenged us to think beyond the boundaries of our own laboratories,” Jirsa said, “and enabled us to go much further together than we could have ever conceived going by ourselves.”
Regenerative medicine has come a long way, baby
After a cloned baby sheep, what started as one of the most controversial areas in medicine is now promising to transform it.
The field of regenerative medicine had a shaky start. In 2002, when news spread about the first cloned animal, Dolly the sheep, a raucous debate ensued. Scary headlines and organized opposition groups put pressure on government leaders, who responded by tightening restrictions on this type of research.
Fast forward to today, and regenerative medicine, which focuses on making unhealthy tissues and organs healthy again, is rewriting the code to healing many disorders, though it’s still young enough to be considered nascent. What started as one of the most controversial areas in medicine is now promising to transform it.
Progress in the lab has addressed previous concerns. Back in the early 2000s, some of the most fervent controversy centered around somatic cell nuclear transfer (SCNT), the process used by scientists to produce Dolly. There was fear that this technique could be used in humans, with possibly adverse effects, considering the many medical problems of the animals who had been cloned.
But today, scientists have discovered better approaches with fewer risks. Pioneers in the field are embracing new possibilities for cellular reprogramming, 3D organ printing, AI collaboration, and even growing organs in space. It could bring a new era of personalized medicine for longer, healthier lives - while potentially sparking new controversies.
Engineering tissues from amniotic fluids
Work in regenerative medicine seeks to reverse damage to organs and tissues by culling, modifying and replacing cells in the human body. Scientists in this field reach deep into the mechanisms of diseases and the breakdowns of cells, the little workhorses that perform all life-giving processes. If cells can’t do their jobs, they take whole organs and systems down with them. Regenerative medicine seeks to harness the power of healthy cells derived from stem cells to do the work that can literally restore patients to a state of health—by giving them healthy, functioning tissues and organs.
Modern-day regenerative medicine takes its origin from the 1998 isolation of human embryonic stem cells, first achieved by John Gearhart at Johns Hopkins University. Gearhart isolated the pluripotent cells that can differentiate into virtually every kind of cell in the human body. There was a raging controversy about the use of these cells in research because at that time they came exclusively from early-stage embryos or fetal tissue.
Back then, the highly controversial SCNT cells were the only way to produce genetically matched stem cells to treat patients. Since then, the picture has changed radically because other sources of highly versatile stem cells have been developed. Today, scientists can derive stem cells from amniotic fluid or reprogram patients’ skin cells back to an immature state, so they can differentiate into whatever types of cells the patient needs.
In the context of medical history, the field of regenerative medicine is progressing at a dizzying speed. But for those living with aggressive or chronic illnesses, it can seem that the wheels of medical progress grind slowly.
The ethical debate has been dialed back and, in the last few decades, the field has produced important innovations, spurring the development of whole new FDA processes and categories, says Anthony Atala, a bioengineer and director of the Wake Forest Institute for Regenerative Medicine. Atala and a large team of researchers have pioneered many of the first applications of 3D printed tissues and organs using cells developed from patients or those obtained from amniotic fluid or placentas.
His lab, considered to be the largest devoted to translational regenerative medicine, is currently working with 40 different engineered human tissues. Sixteen of them have been transplanted into patients. That includes skin, bladders, urethras, muscles, kidneys and vaginal organs, to name just a few.
These achievements are made possible by converging disciplines and technologies, such as cell therapies, bioengineering, gene editing, nanotechnology and 3D printing, to create living tissues and organs for human transplants. Atala is currently overseeing clinical trials to test the safety of tissues and organs engineered in the Wake Forest lab, a significant step toward FDA approval.
In the context of medical history, the field of regenerative medicine is progressing at a dizzying speed. But for those living with aggressive or chronic illnesses, it can seem that the wheels of medical progress grind slowly.
“It’s never fast enough,” Atala says. “We want to get new treatments into the clinic faster, but the reality is that you have to dot all your i’s and cross all your t’s—and rightly so, for the sake of patient safety. People want predictions, but you can never predict how much work it will take to go from conceptualization to utilization.”
As a surgeon, he also treats patients and is able to follow transplant recipients. “At the end of the day, the goal is to get these technologies into patients, and working with the patients is a very rewarding experience,” he says. Will the 3D printed organs ever outrun the shortage of donated organs? “That’s the hope,” Atala says, “but this technology won’t eliminate the need for them in our lifetime.”
New methods are out of this world
Jeanne Loring, another pioneer in the field and director of the Center for Regenerative Medicine at Scripps Research Institute in San Diego, says that investment in regenerative medicine is not only paying off, but is leading to truly personalized medicine, one of the holy grails of modern science.
This is because a patient’s own skin cells can be reprogrammed to become replacements for various malfunctioning cells causing incurable diseases, such as diabetes, heart disease, macular degeneration and Parkinson’s. If the cells are obtained from a source other than the patient, they can be rejected by the immune system. This means that patients need lifelong immunosuppression, which isn’t ideal. “With Covid,” says Loring, “I became acutely aware of the dangers of immunosuppression.” Using the patient’s own cells eliminates that problem.
Microgravity conditions make it easier for the cells to form three-dimensional structures, which could more easily lead to the growing of whole organs. In fact, Loring's own cells have been sent to the ISS for study.
Loring has a special interest in neurons, or brain cells that can be developed by manipulating cells found in the skin. She is looking to eventually treat Parkinson’s disease using them. The manipulated cells produce dopamine, the critical hormone or neurotransmitter lacking in the brains of patients. A company she founded plans to start a Phase I clinical trial using cell therapies for Parkinson’s soon, she says.
This is the culmination of many years of basic research on her part, some of it on her own cells. In 2007, Loring had her own cells reprogrammed, so there’s a cell line that carries her DNA. “They’re just like embryonic stem cells, but personal,” she said.
Loring has another special interest—sending immature cells into space to be studied at the International Space Station. There, microgravity conditions make it easier for the cells to form three-dimensional structures, which could more easily lead to the growing of whole organs. In fact, her own cells have been sent to the ISS for study. “My colleagues and I have completed four missions at the space station,” she says. “The last cells came down last August. They were my own cells reprogrammed into pluripotent cells in 2009. No one else can say that,” she adds.
Future controversies and tipping points
Although the original SCNT debate has calmed down, more controversies may arise, Loring thinks.
One of them could concern growing synthetic embryos. The embryos are ultimately derived from embryonic stem cells, and it’s not clear to what stage these embryos can or will be grown in an artificial uterus—another recent invention. The science, so far done only in animals, is still new and has not been widely publicized but, eventually, “People will notice the production of synthetic embryos and growing them in an artificial uterus,” Loring says. It’s likely to incite many of the same reactions as the use of embryonic stem cells.
Bernard Siegel, the founder and director of the Regenerative Medicine Foundation and executive director of the newly formed Healthspan Action Coalition (HSAC), believes that stem cell science is rapidly approaching tipping point and changing all of medical science. (For disclosure, I do consulting work for HSAC). Siegel says that regenerative medicine has become a new pillar of medicine that has recently been fast-tracked by new technology.
Artificial intelligence is speeding up discoveries and the convergence of key disciplines, as demonstrated in Atala’s lab, which is creating complex new medical products that replace the body’s natural parts. Just as importantly, those parts are genetically matched and pose no risk of rejection.
These new technologies must be regulated, which can be a challenge, Siegel notes. “Cell therapies represent a challenge to the existing regulatory structure, including payment, reimbursement and infrastructure issues that 20 years ago, didn’t exist.” Now the FDA and other agencies are faced with this revolution, and they’re just beginning to adapt.
Siegel cited the 2021 FDA Modernization Act as a major step. The Act allows drug developers to use alternatives to animal testing in investigating the safety and efficacy of new compounds, loosening the agency’s requirement for extensive animal testing before a new drug can move into clinical trials. The Act is a recognition of the profound effect that cultured human cells are having on research. Being able to test drugs using actual human cells promises to be far safer and more accurate in predicting how they will act in the human body, and could accelerate drug development.
Siegel, a longtime veteran and founding father of several health advocacy organizations, believes this work helped bring cell therapies to people sooner rather than later. His new focus, through the HSAC, is to leverage regenerative medicine into extending not just the lifespan but the worldwide human healthspan, the period of life lived with health and vigor. “When you look at the HSAC as a tree,” asks Siegel, “what are the roots of that tree? Stem cell science and the huge ecosystem it has created.” The study of human aging is another root to the tree that has potential to lengthen healthspans.
The revolutionary science underlying the extension of the healthspan needs to be available to the whole world, Siegel says. “We need to take all these roots and come up with a way to improve the life of all mankind,” he says. “Everyone should be able to take advantage of this promising new world.”

