Genetic Testing Companies Are Facing a Racial Bias Problem in Disease Risk Tests

The large genetic studies underlying certain disease risk tests have primarily been done in populations of European ancestry, limiting their accuracy.
Earlier this year, California-based Ambry Genetics announced that it was discontinuing a test meant to estimate a person's risk of developing prostate or breast cancer. The test looks for variations in a person's DNA that are known to be associated with these cancers.
Known as a polygenic risk score, this type of test adds up the effects of variants in many genes — often in the dozens or hundreds — and calculates a person's risk of developing a particular health condition compared to other people. In this way, polygenic risk scores are different from traditional genetic tests that look for mutations in single genes, such as BRCA1 and BRCA2, which raise the risk of breast cancer.
Traditional genetic tests look for mutations that are relatively rare in the general population but have a large impact on a person's disease risk, like BRCA1 and BRCA2. By contrast, polygenic risk scores scan for more common genetic variants that, on their own, have a small effect on risk. Added together, however, they can raise a person's risk for developing disease.
These scores could become a part of routine healthcare in the next few years. Researchers are developing polygenic risk scores for cancer, heart, disease, diabetes and even depression. Before they can be rolled out widely, they'll have to overcome a key limitation: racial bias.
"The issue with these polygenic risk scores is that the scientific studies which they're based on have primarily been done in individuals of European ancestry," says Sara Riordan, president of the National Society of Genetics Counselors. These scores are calculated by comparing the genetic data of people with and without a particular disease. To make these scores accurate, researchers need genetic data from tens or hundreds of thousands of people.
Myriad's old test would have shown that a Black woman had twice as high of a risk for breast cancer compared to the average woman even if she was at low or average risk.
A 2018 analysis found that 78% of participants included in such large genetic studies, known as genome-wide association studies, were of European descent. That's a problem, because certain disease-associated genetic variants don't appear equally across different racial and ethnic groups. For example, a particular variant in the TTR gene, known as V1221, occurs more frequently in people of African descent. In recent years, the variant has been found in 3 to 4 percent of individuals of African ancestry in the United States. Mutations in this gene can cause protein to build up in the heart, leading to a higher risk of heart failure. A polygenic risk score for heart disease based on genetic data from mostly white people likely wouldn't give accurate risk information to African Americans.
Accuracy in genetic testing matters because such polygenic risk scores could help patients and their doctors make better decisions about their healthcare.
For instance, if a polygenic risk score determines that a woman is at higher-than-average risk of breast cancer, her doctor might recommend more frequent mammograms — X-rays that take a picture of the breast. Or, if a risk score reveals that a patient is more predisposed to heart attack, a doctor might prescribe preventive statins, a type of cholesterol-lowering drug.
"Let's be clear, these are not diagnostic tools," says Alicia Martin, a population and statistical geneticist at the Broad Institute of MIT and Harvard. "We can't use a polygenic score to say you will or will not get breast cancer or have a heart attack."
But combining a patient's polygenic risk score with other factors that affect disease risk — like age, weight, medication use or smoking status — may provide a better sense of how likely they are to develop a specific health condition than considering any one risk factor one its own. The accuracy of polygenic risk scores becomes even more important when considering that these scores may be used to guide medication prescription or help patients make decisions about preventive surgery, such as a mastectomy.
In a study published in September, researchers used results from large genetics studies of people with European ancestry and data from the UK Biobank to calculate polygenic risk scores for breast and prostate cancer for people with African, East Asian, European and South Asian ancestry. They found that they could identify individuals at higher risk of breast and prostate cancer when they scaled the risk scores within each group, but the authors say this is only a temporary solution. Recruiting more diverse participants for genetics studies will lead to better cancer detection and prevent, they conclude.
Recent efforts to do just that are expected to make these scores more accurate in the future. Until then, some genetics companies are struggling to overcome the European bias in their tests.
Acknowledging the limitations of its polygenic risk score, Ambry Genetics said in April that it would stop offering the test until it could be recalibrated. The company launched the test, known as AmbryScore, in 2018.
"After careful consideration, we have decided to discontinue AmbryScore to help reduce disparities in access to genetic testing and to stay aligned with current guidelines," the company said in an email to customers. "Due to limited data across ethnic populations, most polygenic risk scores, including AmbryScore, have not been validated for use in patients of diverse backgrounds." (The company did not make a spokesperson available for an interview for this story.)
In September 2020, the National Comprehensive Cancer Network updated its guidelines to advise against the use of polygenic risk scores in routine patient care because of "significant limitations in interpretation." The nonprofit, which represents 31 major cancer cancers across the United States, said such scores could continue to be used experimentally in clinical trials, however.
Holly Pederson, director of Medical Breast Services at the Cleveland Clinic, says the realization that polygenic risk scores may not be accurate for all races and ethnicities is relatively recent. Pederson worked with Salt Lake City-based Myriad Genetics, a leading provider of genetic tests, to improve the accuracy of its polygenic risk score for breast cancer.
The company announced in August that it had recalibrated the test, called RiskScore, for women of all ancestries. Previously, Myriad did not offer its polygenic risk score to women who self-reported any ancestry other than sole European or Ashkenazi ancestry.
"Black women, while they have a similar rate of breast cancer to white women, if not lower, had twice as high of a polygenic risk score because the development and validation of the model was done in white populations," Pederson said of the old test. In other words, Myriad's old test would have shown that a Black woman had twice as high of a risk for breast cancer compared to the average woman even if she was at low or average risk.
To develop and validate the new score, Pederson and other researchers assessed data from more than 275,000 women, including more than 31,000 African American women and nearly 50,000 women of East Asian descent. They looked at 56 different genetic variants associated with ancestry and 93 associated with breast cancer. Interestingly, they found that at least 95% of the breast cancer variants were similar amongst the different ancestries.
The company says the resulting test is now more accurate for all women across the board, but Pederson cautions that it's still slightly less accurate for Black women.
"It's not only the lack of data from Black women that leads to inaccuracies and a lack of validation in these types of risk models, it's also the pure genomic diversity of Africa," she says, noting that Africa is the most genetically diverse continent on the planet. "We just need more data, not only in American Black women but in African women to really further characterize that continent."
Martin says it's problematic that such scores are most accurate for white people because they could further exacerbate health disparities in traditionally underserved groups, such as Black Americans. "If we were to set up really representative massive genetic studies, we would do a much better job at predicting genetic risk for everybody," she says.
Earlier this year, the National Institutes of Health awarded $38 million to researchers to improve the accuracy of polygenic risk scores in diverse populations. Researchers will create new genome datasets and pool information from existing ones in an effort to diversify the data that polygenic scores rely on. They plan to make these datasets available to other scientists to use.
"By having adequate representation, we can ensure that the results of a genetic test are widely applicable," Riordan says.
DNA- and RNA-based electronic implants may revolutionize healthcare
The test tubes contain tiny DNA/enzyme-based circuits, which comprise TRUMPET, a new type of electronic device, smaller than a cell.
Implantable electronic devices can significantly improve patients’ quality of life. A pacemaker can encourage the heart to beat more regularly. A neural implant, usually placed at the back of the skull, can help brain function and encourage higher neural activity. Current research on neural implants finds them helpful to patients with Parkinson’s disease, vision loss, hearing loss, and other nerve damage problems. Several of these implants, such as Elon Musk’s Neuralink, have already been approved by the FDA for human use.
Yet, pacemakers, neural implants, and other such electronic devices are not without problems. They require constant electricity, limited through batteries that need replacements. They also cause scarring. “The problem with doing this with electronics is that scar tissue forms,” explains Kate Adamala, an assistant professor of cell biology at the University of Minnesota Twin Cities. “Anytime you have something hard interacting with something soft [like muscle, skin, or tissue], the soft thing will scar. That's why there are no long-term neural implants right now.” To overcome these challenges, scientists are turning to biocomputing processes that use organic materials like DNA and RNA. Other promised benefits include “diagnostics and possibly therapeutic action, operating as nanorobots in living organisms,” writes Evgeny Katz, a professor of bioelectronics at Clarkson University, in his book DNA- And RNA-Based Computing Systems.
While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output.
Adamala’s research focuses on developing such biocomputing systems using DNA, RNA, proteins, and lipids. Using these molecules in the biocomputing systems allows the latter to be biocompatible with the human body, resulting in a natural healing process. In a recent Nature Communications study, Adamala and her team created a new biocomputing platform called TRUMPET (Transcriptional RNA Universal Multi-Purpose GatE PlaTform) which acts like a DNA-powered computer chip. “These biological systems can heal if you design them correctly,” adds Adamala. “So you can imagine a computer that will eventually heal itself.”
The basics of biocomputing
Biocomputing and regular computing have many similarities. Like regular computing, biocomputing works by running information through a series of gates, usually logic gates. A logic gate works as a fork in the road for an electronic circuit. The input will travel one way or another, giving two different outputs. An example logic gate is the AND gate, which has two inputs (A and B) and two different results. If both A and B are 1, the AND gate output will be 1. If only A is 1 and B is 0, the output will be 0 and vice versa. If both A and B are 0, the result will be 0. While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output. In this case, the DNA enters the logic gate as a single or double strand.
If the DNA is double-stranded, the system “digests” the DNA or destroys it, which results in non-fluorescence or “0” output. Conversely, if the DNA is single-stranded, it won’t be digested and instead will be copied by several enzymes in the biocomputing system, resulting in fluorescent RNA or a “1” output. And the output for this type of binary system can be expanded beyond fluorescence or not. For example, a “1” output might be the production of the enzyme insulin, while a “0” may be that no insulin is produced. “This kind of synergy between biology and computation is the essence of biocomputing,” says Stephanie Forrest, a professor and the director of the Biodesign Center for Biocomputing, Security and Society at Arizona State University.
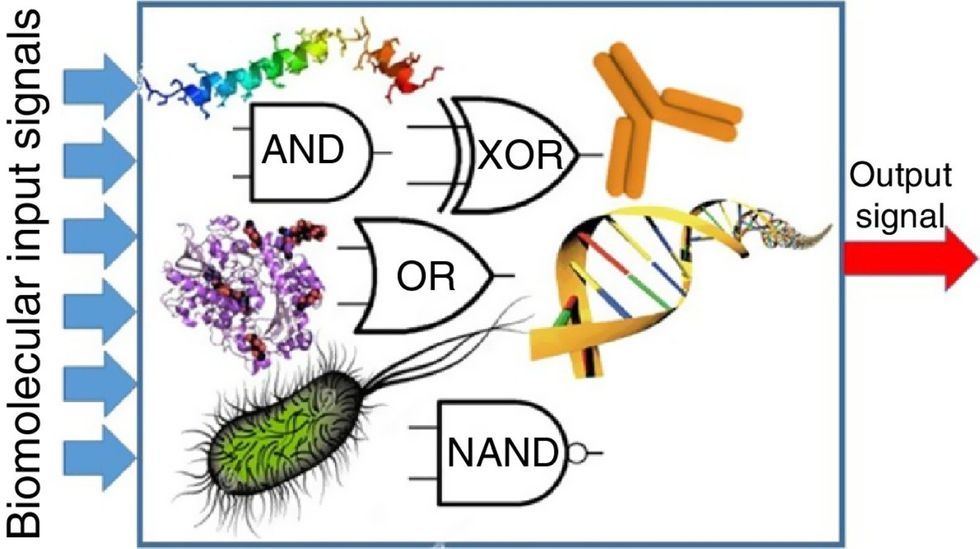
Biocomputing circles are made of DNA, RNA, proteins and even bacteria.
Evgeny Katz
The TRUMPET’s promise
Depending on whether the biocomputing system is placed directly inside a cell within the human body, or run in a test-tube, different environmental factors play a role. When an output is produced inside a cell, the cell's natural processes can amplify this output (for example, a specific protein or DNA strand), creating a solid signal. However, these cells can also be very leaky. “You want the cells to do the thing you ask them to do before they finish whatever their businesses, which is to grow, replicate, metabolize,” Adamala explains. “However, often the gate may be triggered without the right inputs, creating a false positive signal. So that's why natural logic gates are often leaky." While biocomputing outside a cell in a test tube can allow for tighter control over the logic gates, the outputs or signals cannot be amplified by a cell and are less potent.
TRUMPET, which is smaller than a cell, taps into both cellular and non-cellular biocomputing benefits. “At its core, it is a nonliving logic gate system,” Adamala states, “It's a DNA-based logic gate system. But because we use enzymes, and the readout is enzymatic [where an enzyme replicates the fluorescent RNA], we end up with signal amplification." This readout means that the output from the TRUMPET system, a fluorescent RNA strand, can be replicated by nearby enzymes in the platform, making the light signal stronger. "So it combines the best of both worlds,” Adamala adds.
These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body.
The TRUMPET biocomputing process is relatively straightforward. “If the DNA [input] shows up as single-stranded, it will not be digested [by the logic gate], and you get this nice fluorescent output as the RNA is made from the single-stranded DNA, and that's a 1,” Adamala explains. "And if the DNA input is double-stranded, it gets digested by the enzymes in the logic gate, and there is no RNA created from the DNA, so there is no fluorescence, and the output is 0." On the story's leading image above, if the tube is "lit" with a purple color, that is a binary 1 signal for computing. If it's "off" it is a 0.
While still in research, TRUMPET and other biocomputing systems promise significant benefits to personalized healthcare and medicine. These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body. The study’s lead author and graduate student Judee Sharon is already beginning to research TRUMPET's ability for earlier cancer diagnoses. Because the inputs for TRUMPET are single or double-stranded DNA, any mutated or cancerous DNA could theoretically be detected from the platform through the biocomputing process. Theoretically, devices like TRUMPET could be used to detect cancer and other diseases earlier.
Adamala sees TRUMPET not only as a detection system but also as a potential cancer drug delivery system. “Ideally, you would like the drug only to turn on when it senses the presence of a cancer cell. And that's how we use the logic gates, which work in response to inputs like cancerous DNA. Then the output can be the production of a small molecule or the release of a small molecule that can then go and kill what needs killing, in this case, a cancer cell. So we would like to develop applications that use this technology to control the logic gate response of a drug’s delivery to a cell.”
Although platforms like TRUMPET are making progress, a lot more work must be done before they can be used commercially. “The process of translating mechanisms and architecture from biology to computing and vice versa is still an art rather than a science,” says Forrest. “It requires deep computer science and biology knowledge,” she adds. “Some people have compared interdisciplinary science to fusion restaurants—not all combinations are successful, but when they are, the results are remarkable.”
Crickets are low on fat, high on protein, and can be farmed sustainably. They are also crunchy.
In today’s podcast episode, Leaps.org Deputy Editor Lina Zeldovich speaks about the health and ecological benefits of farming crickets for human consumption with Bicky Nguyen, who joins Lina from Vietnam. Bicky and her business partner Nam Dang operate an insect farm named CricketOne. Motivated by the idea of sustainable and healthy protein production, they started their unconventional endeavor a few years ago, despite numerous naysayers who didn’t believe that humans would ever consider munching on bugs.
Yet, making creepy crawlers part of our diet offers many health and planetary advantages. Food production needs to match the rise in global population, estimated to reach 10 billion by 2050. One challenge is that some of our current practices are inefficient, polluting and wasteful. According to nonprofit EarthSave.org, it takes 2,500 gallons of water, 12 pounds of grain, 35 pounds of topsoil and the energy equivalent of one gallon of gasoline to produce one pound of feedlot beef, although exact statistics vary between sources.
Meanwhile, insects are easy to grow, high on protein and low on fat. When roasted with salt, they make crunchy snacks. When chopped up, they transform into delicious pâtes, says Bicky, who invents her own cricket recipes and serves them at industry and public events. Maybe that’s why some research predicts that edible insects market may grow to almost $10 billion by 2030. Tune in for a delectable chat on this alternative and sustainable protein.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Further reading:
More info on Bicky Nguyen
https://yseali.fulbright.edu.vn/en/faculty/bicky-n...
The environmental footprint of beef production
https://www.earthsave.org/environment.htm
https://www.watercalculator.org/news/articles/beef-king-big-water-footprints/
https://www.frontiersin.org/articles/10.3389/fsufs.2019.00005/full
https://ourworldindata.org/carbon-footprint-food-methane
Insect farming as a source of sustainable protein
https://www.insectgourmet.com/insect-farming-growing-bugs-for-protein/
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/insect-farming
Cricket flour is taking the world by storm
https://www.cricketflours.com/
https://talk-commerce.com/blog/what-brands-use-cricket-flour-and-why/

Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

