Genome Reading and Editing Tools for All
An open book representing the ability to read the human genome.
In 2006, the cover of Scientific American was "Know Your DNA" and the inside story was "Genomes for All." Today, we are closer to that goal than ever. Making it affordable for everyone to understand and change their DNA will fundamentally alter how we manage diseases, how we conduct clinical research, and even how we select a mate.
A frequent line of questions on the topic of making genome reading affordable is: Do we need to read the whole genome in order to accurately predict disease risk?
Since 2006, we have driven the cost of reading a human genome down from $3 billion to $600. To aid interpretation and research to produce new diagnostics and therapeutics, my research team at Harvard initiated the Personal Genome Project and later, Openhumans.org. This has demonstrated international informed consent for human genomes, and diverse environmental and trait data can be distributed freely. This is done with no strings attached in a manner analogous to Wikipedia. Cell lines from that project are similarly freely available for experiments on synthetic biology, gene therapy and human developmental biology. DNA from those cells have been chosen by the US National Institute of Standards and Technology and the Food and Drug Administration to be the key federal standards for the human genome.
A frequent line of questions on the topic of making genome reading affordable is: Do we need to read the whole genome in order to accurately predict disease risk? Can we just do most commonly varying parts of the genome, which constitute only a tiny fraction of a percent? Or just the most important parts encoding the proteins or 'exome,' which constitute about one percent of the genome? The commonly varying parts of the genome are poor predictors of serious genetic diseases and the exomes don't detect DNA rearrangements which often wipe out gene function when they occur in non-coding regions within genes. Since the cost of the exome is not one percent of the whole genome cost, but nearly identical ($600), missing an impactful category of mutants is really not worth it. So the answer is yes, we should read the whole genome to glean comprehensively meaningful information.
In parallel to the reading revolution, we have dropped the price of DNA synthesis by a similar million-fold and made genome editing tools close to free.
WRITING
In parallel to the reading revolution, we have dropped the price of DNA synthesis by a similar million-fold and made genome editing tools like CRISPR, TALE and MAGE close to free by distributing them through the non-profit Addgene.org. Gene therapies are already curing blindness in children and cancer in adults, and hopefully soon infectious diseases and hemoglobin diseases like sickle cell anemia. Nevertheless, gene therapies are (so far) the most expensive class of drugs in history (about $1 million dollars per dose).
This is in large part because the costs of proving safety and efficacy in a randomized clinical trial are high and that cost is spread out only over the people that benefit (aka the denominator). Striking growth is evident in such expensive hyper-personalized therapies ever since the "Orphan Drug Act of 1983." For the most common disease, aging (which kills 90 percent of people in wealthy regions of the world), the denominator is maximal and the cost of the drugs should be low as genetic interventions to combat aging become available in the next ten years. But what can we do about rarer diseases with cheap access to genome reading and editing tools? Try to prevent them in the first place.
A huge fraction of these births is preventable if unaffected carriers of such diseases do not mate.
ARITHMETIC
While the cost of reading has plummeted, the value of knowing your genome is higher than ever. About 5 percent of births result in extreme medical trauma over a person's lifetime due to rare genetic diseases. Even without gene therapy, these cost the family and society more than a million dollars in drugs, diagnostics and instruments, extra general care, loss of income for the affected individual and other family members, plus pain and anxiety of the "medical odyssey" often via dozens of mystified physicians. A huge fraction of these births is preventable if unaffected carriers of such diseases do not mate.
The non-profit genetic screening organization, Dor Yeshorim (established in 1983), has shown that this is feasible by testing for Tay–Sachs disease, Familial dysautonomia, Cystic fibrosis, Canavan disease, Glycogen storage disease (type 1), Fanconi anemia (type C), Bloom syndrome, Niemann–Pick disease, Mucolipidosis type IV. This is often done at the pre-marital, matchmaking phase, which can reduce the frequency of natural or induced abortions. Such matchmaking can be done in such a way that no one knows the carrier status of any individual in the system. In addition to those nine tests, many additional diseases can be picked up by whole genome sequencing. No person can know in advance that they are exempt from these risks.
Furthermore, concerns about rare "false positives" is far less at the stage of matchmaking than at the stage of prenatal testing, since the latter could involve termination of a healthy fetus, while the former just means that you restrict your dating to 90 percent of the population. In order to scale this up from 13 million Ashkenazim and Sephardim to billions in diverse cultures, we will likely see new computer security, encryption, blockchain and matchmaking tools.
Once the diseases are eradicated from our population, the interventions can be said to impact not only the current population, but all subsequent generations.
THE FUTURE
As reading and writing become exponentially more affordable and reliable, we can tackle equitable distribution, but there remain issues of education and security. Society, broadly (insurers, health care providers, governments) should be able to see a roughly 12-fold return on their investment of $1800 per person ($600 each for raw data, interpretation and incentivizing the participant) by saving $1 million per diseased child per 20 families. Everyone will have free access to their genome information and software to guide their choices in precision medicines, mates and participation in biomedical research studies.
In terms of writing and editing, if delivery efficiency and accuracy keep improving, then pill or aerosol formulations of gene therapies -- even non-prescription, veterinary or home-made versions -- are not inconceivable. Preventions tends to be more affordable and more humane than cures. If gene therapies provide prevention of diseases of aging, cancer and cognitive decline, they might be considered "enhancement," but not necessarily more remarkable than past preventative strategies, like vaccines against HPV-cancer, smallpox and polio. Whether we're overcoming an internal genetic flaw or an external infectious disease, the purpose is the same: to minimize human suffering. Once the diseases are eradicated from our population, the interventions can be said to impact not only the current population, but all subsequent generations. This reminds us that we need to listen carefully, educate each other and proactively imagine and deflect likely, and even unlikely, unintended consequences, including stigmatization of the last few unprotected individuals.
Have You Heard of the Best Sport for Brain Health?
In this week's Friday Five, research points to this brain healthiest of sports. Plus, the natural way to reprogram cells to a younger state, the network that could underlie many different mental illnesses, and a new test could diagnose autism in newborns. Plus, scientists 3D print an ear and attach it to woman
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- Reprogram cells to a younger state
- Pick up this sport for brain health
- Do all mental illnesses have the same underlying cause?
- New test could diagnose autism in newborns
- Scientists 3D print an ear and attach it to woman
Can blockchain help solve the Henrietta Lacks problem?
Marielle Gross, a professor at the University of Pittsburgh, shows patients a new app that tracks how their samples are used during biomedical research.
Science has come a long way since Henrietta Lacks, a Black woman from Baltimore, succumbed to cervical cancer at age 31 in 1951 -- only eight months after her diagnosis. Since then, research involving her cancer cells has advanced scientific understanding of the human papilloma virus, polio vaccines, medications for HIV/AIDS and in vitro fertilization.
Today, the World Health Organization reports that those cells are essential in mounting a COVID-19 response. But they were commercialized without the awareness or permission of Lacks or her family, who have filed a lawsuit against a biotech company for profiting from these “HeLa” cells.
While obtaining an individual's informed consent has become standard procedure before the use of tissues in medical research, many patients still don’t know what happens to their samples. Now, a new phone-based app is aiming to change that.
Tissue donors can track what scientists do with their samples while safeguarding privacy, through a pilot program initiated in October by researchers at the Johns Hopkins Berman Institute of Bioethics and the University of Pittsburgh’s Institute for Precision Medicine. The program uses blockchain technology to offer patients this opportunity through the University of Pittsburgh's Breast Disease Research Repository, while assuring that their identities remain anonymous to investigators.
A blockchain is a digital, tamper-proof ledger of transactions duplicated and distributed across a computer system network. Whenever a transaction occurs with a patient’s sample, multiple stakeholders can track it while the owner’s identity remains encrypted. Special certificates called “nonfungible tokens,” or NFTs, represent patients’ unique samples on a trusted and widely used blockchain that reinforces transparency.
Blockchain could be used to notify people if cancer researchers discover that they have certain risk factors.
“Healthcare is very data rich, but control of that data often does not lie with the patient,” said Julius Bogdan, vice president of analytics for North America at the Healthcare Information and Management Systems Society (HIMSS), a Chicago-based global technology nonprofit. “NFTs allow for the encapsulation of a patient’s data in a digital asset controlled by the patient.” He added that this technology enables a more secure and informed method of participating in clinical and research trials.
Without this technology, de-identification of patients’ samples during biomedical research had the unintended consequence of preventing them from discovering what researchers find -- even if that data could benefit their health. A solution was urgently needed, said Marielle Gross, assistant professor of obstetrics, gynecology and reproductive science and bioethics at the University of Pittsburgh School of Medicine.
“A researcher can learn something from your bio samples or medical records that could be life-saving information for you, and they have no way to let you or your doctor know,” said Gross, who is also an affiliate assistant professor at the Berman Institute. “There’s no good reason for that to stay the way that it is.”
For instance, blockchain could be used to notify people if cancer researchers discover that they have certain risk factors. Gross estimated that less than half of breast cancer patients are tested for mutations in BRCA1 and BRCA2 — tumor suppressor genes that are important in combating cancer. With normal function, these genes help prevent breast, ovarian and other cells from proliferating in an uncontrolled manner. If researchers find mutations, it’s relevant for a patient’s and family’s follow-up care — and that’s a prime example of how this newly designed app could play a life-saving role, she said.
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app -- called de-bi, which is short for decentralized biobank -- before undergoing a mastectomy for early-stage breast cancer in November, after it was diagnosed on a routine mammogram. She often takes part in medical research and looks forward to tracking her tissues.
“Anytime there’s a scientific experiment or study, I’m quick to participate -- to advance my own wellness as well as knowledge in general,” said Burton, 49, a life insurance service representative who lives in Carnegie, Pa. “It’s my way of contributing.”
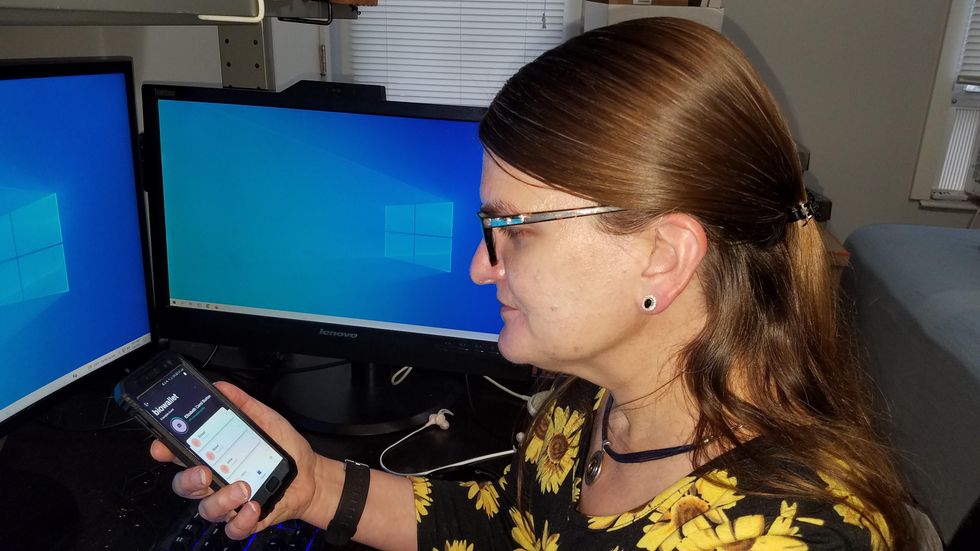
Liz Burton was one of the first patients at the University of Pittsburgh to opt for the app before undergoing a mastectomy for early-stage breast cancer.
Liz Burton
The pilot program raises the issue of what investigators may owe study participants, especially since certain populations, such as Black and indigenous peoples, historically were not treated in an ethical manner for scientific purposes. “It’s a truly laudable effort,” Tamar Schiff, a postdoctoral fellow in medical ethics at New York University’s Grossman School of Medicine, said of the endeavor. “Research participants are beautifully altruistic.”
Lauren Sankary, a bioethicist and associate director of the neuroethics program at Cleveland Clinic, agrees that the pilot program provides increased transparency for study participants regarding how scientists use their tissues while acknowledging individuals’ contributions to research.
However, she added, “it may require researchers to develop a process for ongoing communication to be responsive to additional input from research participants.”
Peter H. Schwartz, professor of medicine and director of Indiana University’s Center for Bioethics in Indianapolis, said the program is promising, but he wonders what will happen if a patient has concerns about a particular research project involving their tissues.
“I can imagine a situation where a patient objects to their sample being used for some disease they’ve never heard about, or which carries some kind of stigma like a mental illness,” Schwartz said, noting that researchers would have to evaluate how to react. “There’s no simple answer to those questions, but the technology has to be assessed with an eye to the problems it could raise.”
To truly make a difference, blockchain must enable broad consent from patients, not just de-identification.
As a result, researchers may need to factor in how much information to share with patients and how to explain it, Schiff said. There are also concerns that in tracking their samples, patients could tell others what they learned before researchers are ready to publicly release this information. However, Bogdan, the vice president of the HIMSS nonprofit, believes only a minimal study identifier would be stored in an NFT, not patient data, research results or any type of proprietary trial information.
Some patients may be confused by blockchain and reluctant to embrace it. “The complexity of NFTs may prevent the average citizen from capitalizing on their potential or vendors willing to participate in the blockchain network,” Bogdan said. “Blockchain technology is also quite costly in terms of computational power and energy consumption, contributing to greenhouse gas emissions and climate change.”
In addition, this nascent, groundbreaking technology is immature and vulnerable to data security flaws, disputes over intellectual property rights and privacy issues, though it does offer baseline protections to maintain confidentiality. To truly make a difference, blockchain must enable broad consent from patients, not just de-identification, said Robyn Shapiro, a bioethicist and founding attorney at Health Sciences Law Group near Milwaukee.
The Henrietta Lacks story is a prime example, Shapiro noted. During her treatment for cervical cancer at Johns Hopkins, Lacks’s tissue was de-identified (albeit not entirely, because her cell line, HeLa, bore her initials). After her death, those cells were replicated and distributed for important and lucrative research and product development purposes without her knowledge or consent.
Nonetheless, Shapiro thinks that the initiative by the University of Pittsburgh and Johns Hopkins has potential to solve some ethical challenges involved in research use of biospecimens. “Compared to the system that allowed Lacks’s cells to be used without her permission, Shapiro said, “blockchain technology using nonfungible tokens that allow patients to follow their samples may enhance transparency, accountability and respect for persons who contribute their tissue and clinical data for research.”
Read more about laws that have prevented people from the rights to their own cells.