How 30 Years of Heart Surgeries Taught My Dad How to Live
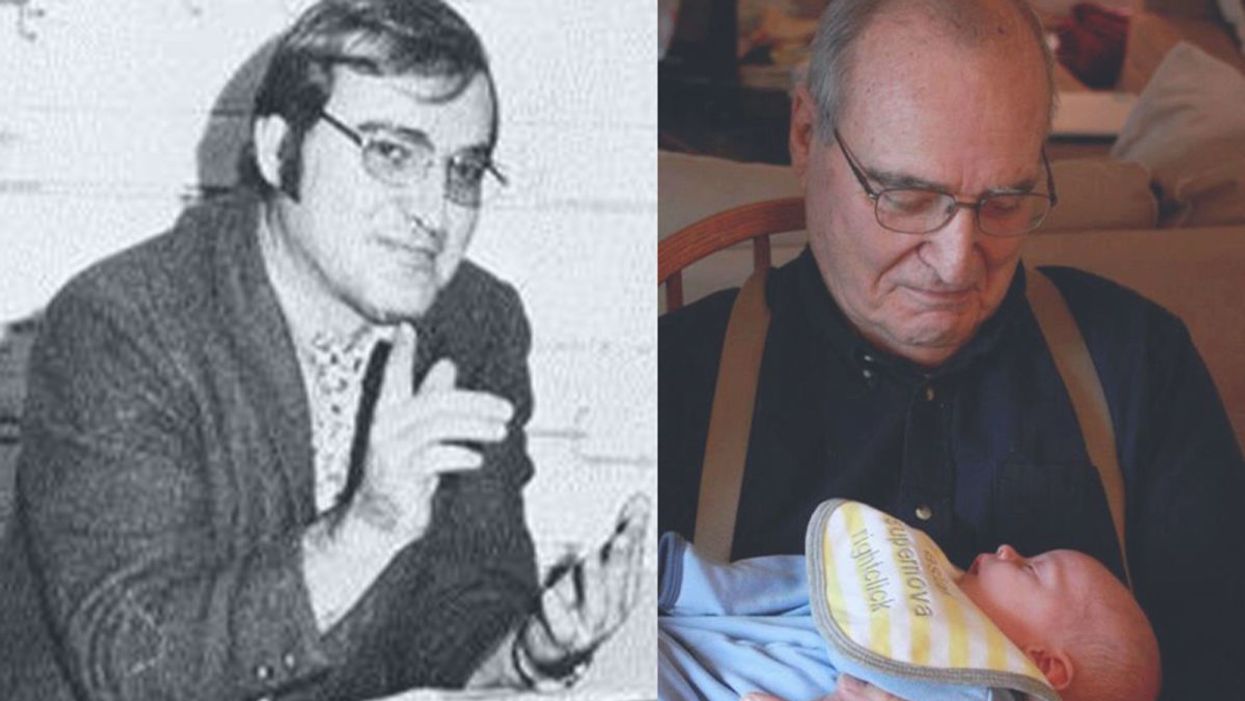
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
The First Mass-Produced Solar Car Is Coming Soon, Sparking Excitement and Uncertainty
Reporter Michaela Haas takes Aptera's Sol car out for a test drive in San Diego, Calif.
The white two-seater car that rolls down the street in the Sorrento Valley of San Diego looks like a futuristic batmobile, with its long aerodynamic tail and curved underbelly. Called 'Sol' (Spanish for "sun"), it runs solely on solar and could be the future of green cars. Its maker, the California startup Aptera, has announced the production of Sol, the world's first mass-produced solar vehicle, by the end of this year. Aptera co-founder Chris Anthony points to the sky as he says, "On this sunny California day, there is ample fuel. You never need to charge the car."
If you live in a sunny state like California or Florida, you might never need to plug in the streamlined Sol because the solar panels recharge while driving and parked. Its 60-mile range is more than the average commuter needs. For cloudy weather, battery packs can be recharged electronically for a range of up to 1,000 miles. The ultra-aerodynamic shape made of lightweight materials such as carbon, Kevlar, and hemp makes the Sol four times more energy-efficient than a Tesla, according to Aptera. "The material is seven times stronger than steel and even survives hail or an angry ex-girlfriend," Anthony promises.
Co-founder Steve Fambro opens the Sol's white doors that fly upwards like wings and I get inside for a test drive. Two dozen square solar panels, each the size of a large square coaster, on the roof, front, and tail power the car. The white interior is spartan; monitors have replaced mirrors and the dashboard. An engineer sits in the driver's seat, hits the pedal, and the low-drag two-seater zooms from 0 to 60 in 3.5 seconds.
It feels like sitting in a race car because the two-seater is so low to the ground but the car is built to go no faster than 100 or 110 mph. The finished car will weigh less than 1,800 pounds, about half of the smallest Tesla. The average car, by comparison, weighs more than double that. "We've built it primarily for energy efficiency," Steve Fambro says, explaining why the Sol has only three wheels. It's technically an "auto-cycle," a hybrid between a motorcycle and a car, but Aptera's designers are also working to design a four-seater.
There has never been a lack of grand visions for the future of the automobile, but until these solar cars actually hit the streets, nobody knows how the promises will hold up.
Transportation is currently the biggest source of greenhouse gases. Developing an efficient solar car that does not burden the grid has been the dream of innovators for decades. Every other year, dozens of innovators race their self-built solar cars 2,000 miles through the Australian desert.
More effective solar panels are finally making the dream mass-compatible, but just like other innovative car ideas, Aptera's vision has been plagued with money problems. Anthony and Fambro were part of the original crew that founded Aptera in 2006 and worked on the first prototype around the same time Tesla built its first roadster, but Aptera went bankrupt in 2011. Anthony and Fambro left a year before the bankruptcy and went on to start other companies. Among other projects, Fambro developed the first USDA organic vertical farm in the United Arab Emirates, and Anthony built a lithium battery company, before the two decided to buy Aptera back. Without a billionaire such as Elon Musk bankrolling the risky process of establishing a whole new car production system from scratch, the huge production costs are almost insurmountable.
But Aptera's founders believe they have found solutions for the entire production process as well as the car design. Most parts of the Sol's body can be made by 3D printers and assembled like a Lego kit. If this makes you think of a toy car, Anthony assures potential buyers that the car aced stress tests and claims it's safer than any vehicle on the market, "because the interior is shaped like an egg and if there is an impact, the pressure gets distributed equally." However, Aptera has yet to release crash test safety data so outside experts cannot evaluate their claims.
Instead of building a huge production facility, Anthony and Fambro envision "micro-factories," each less than 10,000 square feet, where a small crew can assemble cars on demand wherever the orders are highest, be it in California, Canada, or China.
If a part of the Sol breaks, Aptera promises to send replacement parts to any corner of the world within 24 hours, with instructions. So a mechanic in a rural corner in Arkansas or China who never worked on a solar car before simply needs to download the instructions and replace the broken part. At least that's the idea. "The material does not rust nor fatigue," Fambro promises. "You can pass the car onto your grandchildren. When more efficient solar panels hit the market, we simply replace them."
More than 11,000 potential buyers have already signed up; the cheapest model costs around $26,000 USD and Aptera expects the first cars to ship by the end of the year.
Two other solar carmakers are vying for the pole position in the race to be the first to market: The German startup Sono has also announced it will also produce its first solar car by the end of this year. The price tag for the basic model is also around $26,000, but its concept is very different. From the outside, the Sion looks like a conservative minivan for a family; only a closer look reveals that the dark exterior is made of solar panels. Sono, too, nearly went bankrupt a few years ago and was saved through a crowdfunding campaign by enthusiastic fans.
Meanwhile, Norwegian company Lightyear wants to produce a sleek solar-powered luxury sedan by the end of the year, but its price of around $180,000 makes it unaffordable for most buyers.
There has never been a lack of grand visions for the future of the automobile, but until these solar cars actually hit the streets, nobody knows how the promises will hold up. How often will the cars need to be repaired? What happens when snow and ice cover the solar panels? Also, you can't park the car in a garage if you need the sun to charge it.
Critics, including students at the Solar Car team at the University of Michigan, say that mounting solar panels on a moving vehicle will never yield the most efficient results compared to static panels. Also, they are quick to point out that no company has managed to overcome the production hurdles yet. Others in the field also wonder how well the solar panels will actually work.
"It's important to realize that the solar mileage claims by these companies are likely the theoretical best case scenario but in the real world, solar range will be significantly less when you factor in shading, parking in garages, and geographies with lower solar irradiance," says Evan Stumpges, the team coordinator for the American Solar Challenge, a competition in which enthusiasts build and race solar-powered cars. "The encouraging thing is that I have seen videos of real working prototypes for each of these vehicles which is a key accomplishment. That said, I believe the biggest hurdle these companies have yet to face is successfully ramping up to volume production and understanding what their profitability point will be for selling the vehicles once production has stabilized."
Professor Daniel M. Kammen, the founding director of the Renewable and Appropriate Energy Laboratory at the University of California, Berkeley, and one of the world's foremost experts on renewable energy, believes that the technical challenges have been solved, and that solar cars have real advantages over electric vehicles.
"This is the right time to be bullish. Cutting out the charging is a natural solution for long rides," he says. "These vehicles are essentially solar panels and batteries on wheels. These are now record low-cost and can be built from sustainable materials." Apart from Aptera's no-charge technology, he appreciates the move toward no-conflict materials. "Not only is the time ripe but the youth movement is pushing toward conflict-free material and reducing resource waste....A low-cost solar fleet could be really interesting in relieving burden on the grid, or you could easily imagine a city buying a bunch of them and connecting them with mass transit." While he has followed all three new solar companies with interest, he has already ordered an Aptera car for himself, "because it's American and it looks the most different."
After taking a spin in the Sol, it is startling to switch back into a regular four-seater. Rolling out of Aptera's parking lot onto the freeway next to all the oversized gas guzzlers that need to stop every couple of hundreds of miles to fill up, one can't help but think: We've just taken a trip into the future.
Biohackers Made a Cheap and Effective Home Covid Test -- But No One Is Allowed to Use It
A stock image of a home test for COVID-19.
Last summer, when fast and cheap Covid tests were in high demand and governments were struggling to manufacture and distribute them, a group of independent scientists working together had a bit of a breakthrough.
Working on the Just One Giant Lab platform, an online community that serves as a kind of clearing house for open science researchers to find each other and work together, they managed to create a simple, one-hour Covid test that anyone could take at home with just a cup of hot water. The group tested it across a network of home and professional laboratories before being listed as a semi-finalist team for the XPrize, a competition that rewards innovative solutions-based projects. Then, the group hit a wall: they couldn't commercialize the test.
They wanted to keep their project open source, making it accessible to people around the world, so they decided to forgo traditional means of intellectual property protection and didn't seek patents. (They couldn't afford lawyers anyway). And, as a loose-knit group that was not supported by a traditional scientific institution, working in community labs and homes around the world, they had no access to resources or financial support for manufacturing or distributing their test at scale.
But without ethical and regulatory approval for clinical testing, manufacture, and distribution, they were legally unable to create field tests for real people, leaving their inexpensive, $16-per-test, innovative product languishing behind, while other, more expensive over-the-counter tests made their way onto the market.
Who Are These Radical Scientists?
Independent, decentralized biomedical research has come of age. Also sometimes called DIYbio, biohacking, or community biology, depending on whom you ask, open research is today a global movement with thousands of members, from scientists with advanced degrees to middle-grade students. Their motivations and interests vary across a wide spectrum, but transparency and accessibility are key to the ethos of the movement. Teams are agile, focused on shoestring-budget R&D, and aim to disrupt business as usual in the ivory towers of the scientific establishment.
Ethics oversight is critical to ensuring that research is conducted responsibly, even by biohackers.
Initiatives developed within the community, such as Open Insulin, which hopes to engineer processes for affordable, small-batch insulin production, "Slybera," a provocative attempt to reverse engineer a $1 million dollar gene therapy, and the hundreds of projects posted on the collaboration platform Just One Giant Lab during the pandemic, all have one thing in common: to pursue testing in humans, they need an ethics oversight mechanism.
These groups, most of which operate collaboratively in community labs, homes, and online, recognize that some sort of oversight or guidance is useful—and that it's the right thing to do.
But also, and perhaps more immediately, they need it because federal rules require ethics oversight of any biomedical research that's headed in the direction of the consumer market. In addition, some individuals engaged in this work do want to publish their research in traditional scientific journals, which—you guessed it—also require that research has undergone an ethics evaluation. Ethics oversight is critical to ensuring that research is conducted responsibly, even by biohackers.
Bridging the Ethics Gap
The problem is that traditional oversight mechanisms, such as institutional review boards at government or academic research institutions, as well as the private boards utilized by pharmaceutical companies, are not accessible to most independent researchers. Traditional review boards are either closed to the public, or charge fees that are out of reach for many citizen science initiatives. This has created an "ethics gap" in nontraditional scientific research.
Biohackers are seen in some ways as the direct descendents of "white hat" computer hackers, or those focused on calling out security holes and contributing solutions to technical problems within self-regulating communities. In the case of health and biotechnology, those problems include both the absence of treatments and the availability of only expensive treatments for certain conditions. As the DIYbio community grows, there needs to be a way to provide assurance that, when the work is successful, the public is able to benefit from it eventually. The team that developed the one-hour Covid test found a potential commercial partner and so might well overcome the oversight hurdle, but it's been 14 months since they developed the test--and counting.
In short, without some kind of oversight mechanism for the work of independent biomedical researchers, the solutions they innovate will never have the opportunity to reach consumers.
In a new paper in the journal Citizen Science: Theory & Practice, we consider the issue of the ethics gap and ask whether ethics oversight is something nontraditional researchers want, and if so, what forms it might take. Given that individuals within these communities sometimes vehemently disagree with each other, is consensus on these questions even possible?
We learned that there is no "one size fits all" solution for ethics oversight of nontraditional research. Rather, the appropriateness of any oversight model will depend on each initiative's objectives, needs, risks, and constraints.
We also learned that nontraditional researchers are generally willing (and in some cases eager) to engage with traditional scientific, legal, and bioethics experts on ethics, safety, and related questions.
We suggest that these experts make themselves available to help nontraditional researchers build infrastructure for ethics self-governance and identify when it might be necessary to seek outside assistance.
Independent biomedical research has promise, but like any emerging science, it poses novel ethical questions and challenges. Existing research ethics and oversight frameworks may not be well-suited to answer them in every context, so we need to think outside the box about what we can create for the future. That process should begin by talking to independent biomedical researchers about their activities, priorities, and concerns with an eye to understanding how best to support them.
Christi Guerrini, JD, MPH studies biomedical citizen science and is an Associate Professor at Baylor College of Medicine. Alex Pearlman, MA, is a science journalist and bioethicist who writes about emerging issues in biotechnology. They have recently launched outlawbio.org, a place for discussion about nontraditional research.

