How 30 Years of Heart Surgeries Taught My Dad How to Live
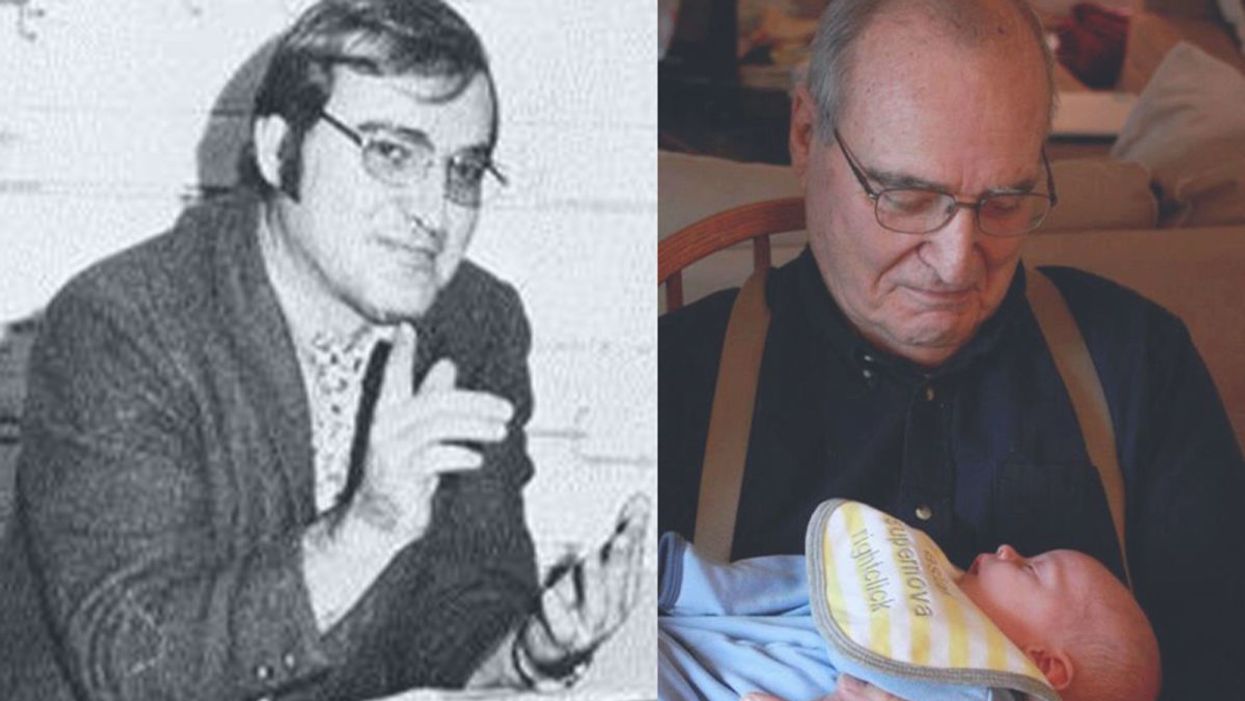
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Dana Lewis, pictured in Mount Vernon in 2017, worked with her engineer husband to design an artificial pancreas system to manage her type 1 diabetes.
For years, a continuous glucose monitor would beep at night if Dana Lewis' blood sugar measured too high or too low. At age 14, she was diagnosed with type 1 diabetes, an autoimmune disease that destroys insulin-producing cells in the pancreas.
The FDA just issued its first warning to the DIY diabetic community, after one patient suffered an accidental insulin overdose.
But being a sound sleeper, the Seattle-based independent researcher, now 30, feared not waking up. That concerned her most when she would run, after which her glucose dropped overnight. Now, she rarely needs a rousing reminder to alert her to out-of-range blood glucose levels.
That's because Lewis and her husband, Scott Leibrand, a network engineer, developed an artificial pancreas system—an algorithm that calculates adjustments to insulin delivery based on data from the continuous glucose monitor and her insulin pump. When the monitor gives a reading, she no longer needs to press a button. The algorithm tells the pump how much insulin to release while she's sleeping.
"Most of the time, it's preventing the frequent occurrences of high or low blood sugars automatically," Lewis explains.
Like other do-it-yourself device innovations, home-designed artificial pancreas systems are not approved by the Food and Drug Administration, so individual users assume any associated risks. Experts recommend that patients consult their doctor before adopting a new self-monitoring approach and to keep the clinician apprised of their progress.
DIY closed-loop systems can be uniquely challenging, according to the FDA. Patients may not fully comprehend how the devices are intended to work or they may fail to recognize the limitations. The systems have not been evaluated under quality control measures and pose risks of inappropriate dosing from the automated algorithm or potential incompatibility with a patient's other medications, says Stephanie Caccomo, an FDA spokeswoman.
Earlier this month, in fact, the FDA issued its first warning to the DIY diabetic community, which includes thousands of users, after one patient suffered an accidental insulin overdose.
Patients who built their own systems from scratch may be more well-versed in the operations, while those who are implementing unapproved designs created by others are less likely to be familiar with their intricacies, she says.
"Malfunctions or misuse of automated-insulin delivery systems can lead to acute complications of hypo- and hyperglycemia that may result in serious injury or death," Caccomo cautions. "FDA provides independent review of complex systems to assess the safety of these nontransparent devices, so that users do not have to be software/hardware designers to get the medical devices they need."
Only one hybrid closed-loop technology—the MiniMed 670G System from Minneapolis-based Medtronic—has been FDA-approved for type 1 use since September 2016. The term "hybrid" indicates that the system is not a fully automatic closed loop; it still requires minimal input from patients, including the need to enter mealtime carbohydrates, manage insulin dosage recommendations, and periodically calibrate the sensor.
Meanwhile, some tech-savvy people with type 1 diabetes have opted to design their own systems. About one-third of the DIY diabetes loopers are children whose parents have built them a closed system, according to Lewis' website.
Lewis began developing her system in 2014, well before Medtronic's device hit the market. "The choice to wait is not a luxury," she says, noting that "diabetes is inherently dangerous," whether an individual relies on a device to inject insulin or administers it with a syringe.
Hybrid closed-loop insulin delivery improves glucose control while decreasing the risk of low blood sugar in patients of various ages with less than optimally controlled type 1 diabetes, according to a study published in The Lancet last October. The multi-center randomized trial, conducted in the United Kingdom and the United States, spanned 12 weeks and included adults, adolescents, and children aged 6 years and older.
"We have compelling data attesting to the benefits of closed-loop systems," says Daniel Finan, research director at JDRF (formerly the Juvenile Diabetes Research Foundation) in New York, a global organization funding the study.
Medtronic's system costs between $6,000 and $9,000. However, end-user pricing varies based on an individual's health plan. It is covered by most insurers, according to the device manufacturer.
To give users more choice, in 2017 JDRF launched the Open Protocol Automated Insulin Delivery Systems initiative to collaborate with the FDA and experts in the do-it-yourself arena. The organization hopes to "forge a new regulatory paradigm," Finan says.
As diabetes management becomes more user-controlled, there is a need for better coordination. "We've had insulin pumps for a very long time, but having sensors that can detect blood sugars in real time is still a very new phenomenon," says Leslie Lam, interim chief in the division of pediatric endocrinology and diabetes at The Children's Hospital at Montefiore in the Bronx, N.Y.
"There's a lag in the integration of this technology," he adds. Innovators are indeed working to bring new products to market, "but on the consumer side, people want that to be here now instead of a year or two later."
The devices aren't foolproof, and mishaps can occur even with very accurate systems. For this reason, there is some reluctance to advocate for universal use in children with type 1 diabetes. Supervision by a parent, school nurse, and sometimes a coach would be a prudent precaution, Lam says.
People engage in "this work because they are either curious about it themselves or not getting the care they need from the health care system, or both."
Remaining aware of blood sugar levels and having a backup plan are essential. "People still need to know how to give injections the old-school way," he says.
To ensure readings are correct on Medtronic's device, users should check their blood sugar with traditional finger pricking at least five or six times per day—before every meal and whenever directed by the system, notes Elena Toschi, an endocrinologist and director of the Young Adult Clinic at Joslin Diabetes Center, an affiliate of Harvard Medical School.
"There can be pump failure and cross-talking failure," she cautions, urging patients not to stop being vigilant because they are using an automated device. "This is still something that can happen; it doesn't eliminate that."
While do-it-yourself devices help promote autonomy and offer convenience, the lack of clinical trial data makes it difficult for clinicians and patients to assess risks versus benefits, says Lisa Eckenwiler, an associate professor in the departments of philosophy and health administration and policy at George Mason University in Fairfax, Va.
"What are the responsibilities of physicians in that context to advise patients?" she questions. Some clinicians foresee the possibility that "down the road, if things go awry" with disease management, that could place them "in a moral quandary."
Whether it's controlling diabetes, obesity, heart disease or asthma, emerging technologies are having a major influence on individuals' abilities to stay on top of their health, says Camille Nebeker, an assistant professor in the School of Medicine at the University of California, San Diego, and founder and director of its Research Center for Optimal Data Ethics.
People engage in "this work because they are either curious about it themselves or not getting the care they need from the health care system, or both," she says. In "citizen science communities," they may partner in participant-led research while gaining access to scientific and technical expertise. Others "may go it alone in solo self-tracking studies or developing do-it-yourself technologies," which raises concerns about whether they are carefully considering potential risks and weighing them against possible benefits.
Dana Lewis admits that "using do-it-yourself systems might not be for everyone. But the advances made in the do-it-yourself community show what's possible for future commercial developments, and give a lot of hope for improved quality of life for those of us living with type 1 diabetes."
The Grim Reaper Can Now Compost Your Body
An artist's rendering of a future Recompose facility in Washington state, with reusable modular vessels that convert human remains to soil.
Ultra-green Seattle isn't just getting serious about living eco-friendly, but dying that way, too. As of this week, Washington is officially the first state to allow citizens to compost their own dead bodies.
Their bodies, including bones, were converted into clean, odorless soil free of harmful pathogens.
The Lowdown
Keep in mind this doesn't mean dumping your relative in a nearby river. Scientists and organizations have ways to help Mother Nature process the remains. For instance, the late actor Luke Perry reportedly was buried in a mushroom suit. Perry's garment is completely biodegradable and the attached microorganisms help the decomposition process cleanly and efficiently.
A biodegradable burial requires only a fraction of the energy used for cremation and can save a metric ton of CO2. The body decomposes in about a month. Besides a mushroom suit, another option coming down the pike in Washington state is to have your body converted directly into soil in a special facility.
A pilot study last summer by a public benefit corporation called Recompose signed up six terminally ill people who donated their remains for such research. Their bodies, including bones, were converted into clean, odorless soil free of harmful pathogens. That soil—about a cubic yard per person--could then be returned after 30 days to the subjects' families.
Green burials open the door to creative memorials. A tree or garden could be planted with your soil. This method provides a climate-friendly alternative to traditional funerals, circumventing toxic embalming fluid, expensive casket materials and other ecological overhead. The fertile soil could also be given to conservationist organizations.
Next Up
The new legislation in Washington will take effect May 1, 2020. The Pacific Northwest state has one of the highest cremation rates in the nation at 78 percent, only second to Nevada. Rising climate change and increased interest in death management will only speed this discussion to the forefront in other states.
A biodegradable burial requires only a fraction of the energy used for cremation and can save a metric ton of CO2.
It's also worth noting Perry wasn't buried in Washington State, but in Tennessee. It is unknown where exactly he was laid to rest, nor if it was done under a legal precedent or special exception.
According to the Green Burial Council, each state varies on how and where you can bury someone. Home burials are usually legal, but to do so requires establishing an official cemetery area on the property. How someone is buried has even more dynamic legislation. There will be new discussions about how neighbors contend with nearby decomposing bodies, legal limitations to private burial techniques, and other issues never addressed before in modern mainstream America.
Open Questions
It's unclear if green burials will be commonplace for those with less financial means or access. Mushroom suits average a couple thousand dollars, making them more expensive than a low-end casket. There are also the less obvious expenses, including designating the place of burial, and getting proper burial support and guidance. In short, you likely won't go to the local funeral home and be taken care of properly. It is still experimental.
As for "natural organic reduction" (converting human remains to soil in reusable modular vessels), Recompose is still figuring out its pricing for Washington residents, but expects the service to cost more than cremation and less than a conventional burial.
For now, environmentally sustainable death care may be comparable to vegetarianism in the 1970s or solar paneling in the 1980s: A discussion among urbanites and upwardly-mobile financial classes, but not yet an accessible option for the average American. It's not a coincidence that the new Washington law received support in Seattle, one of the top 10 wealthiest cities in America. A similar push may take off in less affluent areas if ecological concerns drive a demand for affordable green burial options.
Until then, your neighborhood mortician still has the death business on lock.

