How 30 Years of Heart Surgeries Taught My Dad How to Live
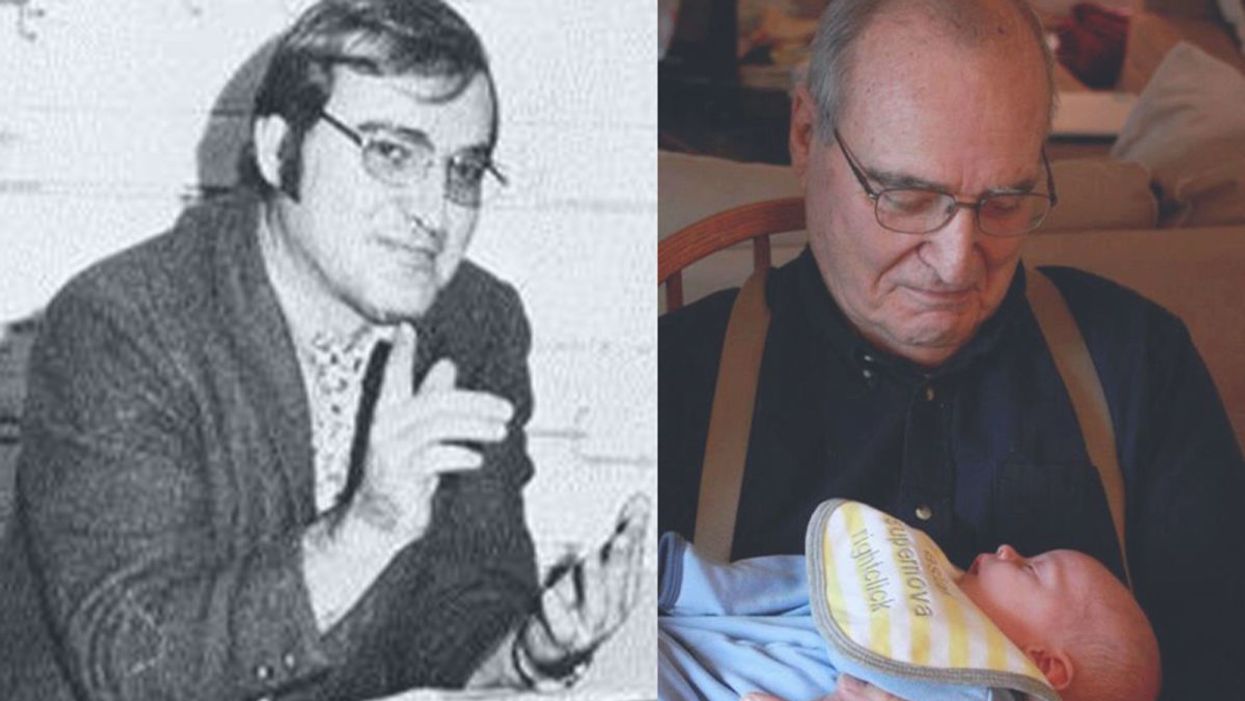
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
A rendering of a female cyborg.
Viv spent nearly an hour choosing her body.
She considered going as her eight year-old self. She would stand eye-to-eye with her father in his hospital bed, shedding tears and crying: please don't go, daddy. But that was too obvious. It would offend him.
He became data coursing through a network, able to embody any form, to outlive physical decay.
She considered her eighteen year-old self. She would lean over him, scrawny and tall, her lips trembling with anger: you're being selfish, dad. But that would lead to shouting.
She considered every form, even reviving people from the past: her mother, her grandfather, her little sister Mary. How would her father react to Mary walking in? He would think himself dead. She could whisper a message to him: Stay alive, dad. God commands it.
In the end, Viv chose the look of her last days as a biological person. Thirty-one years old, her auburn hair cut short, her black eyes full of longing. She watched the body print in silicon over robotic armature.
When it blinked to life, Viv stood in front of a mirror. Her face was appropriately somber, her mind in sync with her new muscles. Without thinking, she stretched her arms, arched her body, twirled on her tiptoes. She had forgotten the pleasure of sensation.
"I should do this…" The voice resonated through her. She could not help but smile. "I should do this more often… often… often." Every repetition thrilled her with sound. She began to sing an old favorite: "Times have changed… and we've often…"
But she stopped herself. This was not a day for singing.
Viv clothed her body in a blue dress, packed her tablet in a briefcase, stood in front of the mirror one last time. "I'll be there in five," she said aloud, though she did not need to.
A man's voice answered in her mind: I'm not coming.
"Gabe…"
There's no point, said the voice. We know what he'll say.
"We have to try."
I won't see him dying, Viv.
The clenching of her jaw felt like the old days. Her brother made a habit of last-minute decisions, without concern for how they affected other people, most often her.
She remembered the day he became an everperson. It was soon after their mother's death. They were supposed to visit their father in mourning, but Gabe disappeared without explanation. Viv took the full burden of solace on herself. She sat with her father in a small room, with an old Persian rug and stale furniture. His mustache was beginning to gray, his eyes beginning to wrinkle. "She's with your sister now," he said. "Your mom and Mary, I can…" He leaned in to whisper, "I can almost hear them, at night, laughing on the other side. They tell me to wait… they tell me to wait." Viv nodded for him, pretending to believe, wishing she could.
Gabe did not return her calls that evening. The next day, she began to worry. The day after, she began to look. He made no effort to hide, he simply neglected to tell her the new plan.
Gabe had taken the money from his inheritance, and booked himself an everence. It was something new back then. Viv did not understand the science, but she knew it was a destructive process. His physical brain was destroyed by lasers that scanned it neuron by neuron, creating a digital replica. He became data coursing through a network, able to embody any form, to outlive physical decay. He became an everperson.
It took three days to complete. Viv went to the facility, a converted warehouse by the Bay Bridge. She watched the new Gabe being printed over robotic armature, taking the form of his last biological self, to help with the transition. When he blinked to life, she did not know if he would be the same person, or an imperfect copy of an imperfect copy. But Gabe was totally oblivious to the pain he caused her by disappearing in that way. No robot, she thought, could be so callous.
When Viv made her own decision to everize, she deliberated for weeks, thinking through the consequences and conversations to come. Afterwards, she sat with her father in that same small room, with the Persian rug older, the furniture staler, a new cat purring at his feet.
"But it's suicide," he said.
"It's the opposite, dad. It's eternal life."
"You'd be a robot. You wouldn't be you."
"Gabe's the same as he ever was," she noted the resentment in her voice. "He's just not… physical, until he wants to be."
Her father exhaled an Arabic phrase he was using more often in his old age. La hawla wa la quwata illa billah. She had never learned his native tongue, but she looked up the phrase to understand him better. It meant something like: there is no power except in God. It was a sigh of resignation.
"Vivian," he said eventually, "Your soul is not your brain. Your soul lives on. If you kill yourself, you... it's unforgivable. Don't you want to see mom in heaven? Mary? Me?"
She wanted to believe. She wanted painfully. But when she spoke, it was barely a whisper. "I don't think that will happen, dad."
Fewer biological people meant little need for hospitals, or doctors. It would close soon.
It was the first she had ever confessed to him about God or Heaven. In as steady a voice as he could manage, her father said: "You're an adult, Viv. You do what you think is best."
She came to visit sometimes, as an everperson. He could not tell at first. But as the years went by, as his eyes wrinkled, and his hair grayed, he noticed that Viv never aged. One day he stopped talking to her. Another she stopped coming.
Now he was waiting out the last days of his life alone in a hospital bed. Viv did not want to say goodbye. It seemed such a waste.
You don't have to, Gabe spoke into her mind. Get him to sign, say anything, say it's for selling the house. Once we have full power of attorney, we can decide for him.
"It's not right." She noticed herself speaking aloud on the hoverbus. Nine nervous faces turned to her.
It's not right, she continued in her mind. Dad never forced us to pray, never forced us to —
That was mom.
But he loved her. He never changed her mind, he raised us to question, and he quietly believed. He has every right to live his way, just like we did.
To live. Not to die... When he's an everperson, he'll thank us.
That gave her pause. It might be true. She remembered her first moments as an everperson, suddenly linked to countless other minds, waking to the full expanse of human knowledge like sunlight through an open window, breathless and unexpected.
Still, she said, it's not right.
So you want him to die?
I want to convince him.
And what if you don't? There was panic in his voice. Gabe steadied himself. You brought your tablet, Viv. You know what it's for. Get him to sign.
And what if I don't?
I'll figure something out, with or without you. I won't let him die, Viv. Not this day and age.
Viv kept quiet the rest of her way there. She played memories in her mind, of every conversation she ever had with her father, every time he read her a verse or taught her a parable. She looked for a way to convince him, some doubt, some chink in his armor of belief. But she got distracted by the world outside.
It was strange to pass for a time through physical space. It took longer than she expected. Now watching the sunlight refract through the hoverbus window, she was mesmerized. Every sensation felt more real, more vivid than her memory. "I should do this more often," she said aloud.
The hospital smelled like death. It had fallen into disrepair since her mother's illness. Fewer biological people meant little need for hospitals, or doctors. It would close soon, she thought. Her footsteps echoed through the halls, along with the sounds of old televisions playing old films to keep the patients company.
The room she entered had no sound, except the whirring machines. No light, except an eerie glow filtering through the curtains. The figure on the bed was her father, his breathing strained, his skin cracked like the desert. She closed the door behind her.
When her father turned, she saw a flicker of joy in his eyes. It disappeared.
"La hawla wa la… I thought it was her."
"I am her."
He winced. "She died some twenty years ago."
Viv sat next to him. The machines whirred around them, keeping his body alive another day, or hour, or minute. "It doesn't look good, dad."
"I know."
"You broke a promise."
He held her gaze. "I did?"
"You said we'd see the bats in Australia."
"You were scared of bats."
"And you said they were cute in Oz, the giant bats, like upside down puppies chewing bananas."
He smiled, but that was a long time ago. "Your mom was alive then… Gabe… You were alive…"
"I'm alive now, dad. Look at me. I'm Viv. Vivian Fatema. Your daughter. Half mom, half you. I'm the same person I was."
His eyes shifted. She sensed he wanted to believe. She held his hand and squeezed it. She felt him squeezing back. "I want you to stay, dad."
"There's nothing for me here."
"I'm here."
"You don't love me, Viv. You're a robot."
His hand let go. "You're there… I don't know where. I have a lot to answer for, Viv. I pray. I pray every day, five times a day, sometimes more. I pray that God forgive you for what you did, forgive me for my part, forgive Gabriel... I wish I could stay, love, but… Everyone I love is on the other side."
It hurt her to say the next words: "It's not real, dad."
"Of course you'd say that." He turned his body away from her.
"Please, dad."
She listened to his breathing.
"I love you," she said.
"You don't love me, Viv. You're a robot."
She lowered her head against the bed. She kneeled for countless breaths. It took all her strength to stand up again.
Viv took her briefcase, pulled out her tablet. She stood tapping at the screen for some time. The clenching of her jaw felt like the old days.
"Before I go, I need you to sign something. It's a power of attorney for the house. We can't sell it without you."
"You're selling the house?"
She shrugged. "It's no use to a robot."
His bony finger signed the screen without reading it. She kissed his forehead goodbye.
"Viv?" She stopped. "Before you go, could you open the curtains?"
She did. Her last image of him was a frail old body gazing at the moving clouds.
On the hoverbus home, Viv turned against the window outside. She pressed the briefcase to her like a hug, her mechanical heart thumping against it. Every heartbeat brought a memory back of her biological life. "I should do this more…" She whispered to herself, not caring who might hear. The sunset turned violet.
You made him sign. Gabe sounded like triumph.
"I did."
You did the right thing.
"I know."
Let me see.
She pulled out her tablet and, with a touch, uploaded the file.
Where's my name? Gabe asked. I only see your name.
"I changed it."
What do you mean you "changed it"?
"I changed my mind last minute, Gabe. I didn't think to tell you."
That's funny, sis. Very funny.
"It's not funny at all, Gabe. It's dead serious. I have power of attorney. I'm going to bury him next to mom and Mary."
No… There's no way.
"It's my choice now."
I can't watch him go, Viv. I can't. Don't be selfish.
"I'll miss him." She felt a pain in her chest. "I'll miss him too." Her voice was different now. "But it's what he wanted."
Gabe left her. She heard nothing but her thoughts. Unbearable thoughts.
Viv turned to the darkening world outside. She found her reflection instead, her reflection in tears. She saw her father's eyes.
The opioid crisis depicted with a map of the USA filled with oxycodone and hydrocodone pills.
The largest ever seizure of fentanyl in the United States – 254 pounds of the white powder, enough to kill 1 in 3 Americans by overdose – was found under a shipment of cucumbers recently.
A policing approach alone is insufficient to take on the opioid crisis.
Those types of stories barely make the headlines any more, in part because illicit drugs are no longer just handsold by drug dealers; these sales have gone online. The neighborhood dealer faces the same evolving environment as other retailers and may soon go the way of Sears.
But opioids themselves are not going away. I could make an opioid purchase online in about 30 seconds and have it sent to my door, says Joe Smyser. The epidemiologist and president of The Public Good Projects isn't bragging, he's simply stating a fact about the opioid crisis that has struck the United States. The U.S Drug Enforcement Agency, social media companies, and some foreign governments have undertaken massive efforts to shut down sites selling illegal drugs, and they have gotten very good at it, shuttering most within a day of their opening.
But it's a Whac-A-Mole situation in which new ones pop up as quickly as older ones are closed; they are promoted through hashtags, social media networks, and ubiquitous email spam to lure visitors to a website or call a WhatsApp number to make a purchase. The online disruption by law enforcement has become simply another cost of doing business for drug sellers. Fentanyl, and similar analogues created to evade detection and the law, are at the center of it. Small amounts can be mixed with other "safer" opioids to get a high, and the growth of online sales have all contributed to the surge of opioid-related deaths: about 17,500 in 2006; 47,600 in 2017; and a projected 82,000 a year by 2025.
All of this has occurred even while authorities have been cracking down on the prescribing of opioids, and prescription-related deaths have declined. Clearly a policing approach alone is insufficient to take on the opioid crisis.
Building the Tools
The Public Good Projects (PGP), a nonprofit organization founded by concerned experts, was set up to better understand public health issues in this new online environment and better shape responses. The first step is to understand what people are hearing and the language they are using by monitoring social media and other forms of public communications. "We're collecting data from every publicly available media source that we can get our hands on. It's broadcast television data, it's radio, it's print newspapers and magazines. And then it's online data; it's online video, social media, blogs, websites," Smyser explains.
The purpose was to better understand the opioid crisis and find out if there were differences between affected rural and urban populations.
"Then our job is to create queries, create searches of all of that data so that we find what is the information that Americans are exposed to about a topic, and then what … Americans [are] sharing amongst themselves about that same topic."
He says it's the same thing business has been doing for years to monitor their "brand health" and be prepared for possible negative issues that might arise about their products and services. He believes PGP is the first group to use those tools for public health.
Looking At Opioids
PGP's work on opioids started with a contract from the Substance Abuse and Mental Health Administration (SAMHSA) through the National Science Foundation. The purpose was simply to better understand the opioid crisis in the United States and in particular find out if there were differences between affected rural and urban populations. A team of data scientists, public health professionals, and cultural anthropologists needed several months to sort out and organize the algorithms from the sheer volume of data.
Drug use is particularly rich in slang, where a specific drug or way of using it can be referred to in multiple ways in different towns and social groups. Traditional media often uses clinical terms, Twitter shorthand, and all of that has to be structured and integrated "so that it isn't just spitting out data that is gobbledygook and of no use to anyone," says Smyser.
The data they gather is both cumulative and in real time, tabulated and visually represented in constantly morphing hashtag and word clouds where the color and size of the word indicates the source and volume of its use.

Popular hashtags on Twitter relating to the opioid crisis.
(Credit: The Public Good Projects)
The visual presentation of data helps to understand what different groups are saying and how they are saying it. For example, compare the hashtag and word clouds. Younger people are more likely to use the hashtags of Twitter, while older people are more likely to use older forms of media, and that is reflected in their concerns and language in those clouds.

Popular words relating to the opioid crisis gathered from older forms of media.
(Credit: The Public Good Projects)
A Ping map shows the origin of messages, while a Spidey map shows the network of how messages are being forwarded and shared among people. These sets of data can be overlaid with zip code, census, and socioeconomic data to provide an even deeper sense of who is saying what. And when integrated together, they provide clues to topics and language that might best engage people in each niche.

A Ping map showing the origin of messages around the opioid crisis.
(Credit: The Public Good Projects)
Opioids Speak
One thing that quickly became apparent to PGP in monitoring the media is that "over half of the information that the American public is exposed to about opioids is a very distant policy debate," says Smyser.
It is political pronouncements in DC, the legal system going after pharmaceutical companies that promoted prescription opioids for pain relief (and more), or mandatory prison terms for offenders. Relatively little is about treatment, the impact on families and communities, and what people can do themselves. That is particularly important in light of another key finding: residents of "Trump-land," the rural areas that supported the president and are being ravaged by opioids, talk about the problem and solutions very differently from urban areas.
"In rural communities there is usually a huge emphasis on self-reliance, and we take care of each other; that's why we enjoy living here. We are a neighborhood, we come together and we fix our own problems," according to Smyser.
In contrast, urban communities tend to be more transient, less likely to live in multigenerational households and neighborhoods, and look to formal institutions rather than themselves for solutions. "The message that we're sending people is one where there is really no role whatsoever for self-efficacy...we're giving them nothing to do" to help solve the problem themselves, says Smyser. "In fact, I could argue it is reducing self-efficacy."
Residents of "Trump-land," the rural areas that supported the president and are being ravaged by opioids, talk about the problem and solutions very differently from urban areas.
The opioid crisis is complex and improving the situation will be too. Smyser believes a top-down policing approach alone will not work; it is better to provide front-line public health officers at the state and local level with more and current intelligence so they can respond in their communities.
"I think that would be enormously impactful. But right now, we just don't have that service." SAMHSA declined multiple requests to discuss this project paid for with federal money. A spokesman concluded with: "That project occurred under the previous administration, and we did not have a direct relationship with PGP. As a result, I am unable to comment on the project."
The Milken Institute Center for Public Health, a think tank that is working to find solutions to the opioid epidemic, had an upbeat response. Director Sabrina Spitaletta said, "PGP's work to provide real-time data that monitors topics of high concern in public health has been very helpful to many of the front-line organizations working to combat this crisis."

