How 30 Years of Heart Surgeries Taught My Dad How to Live
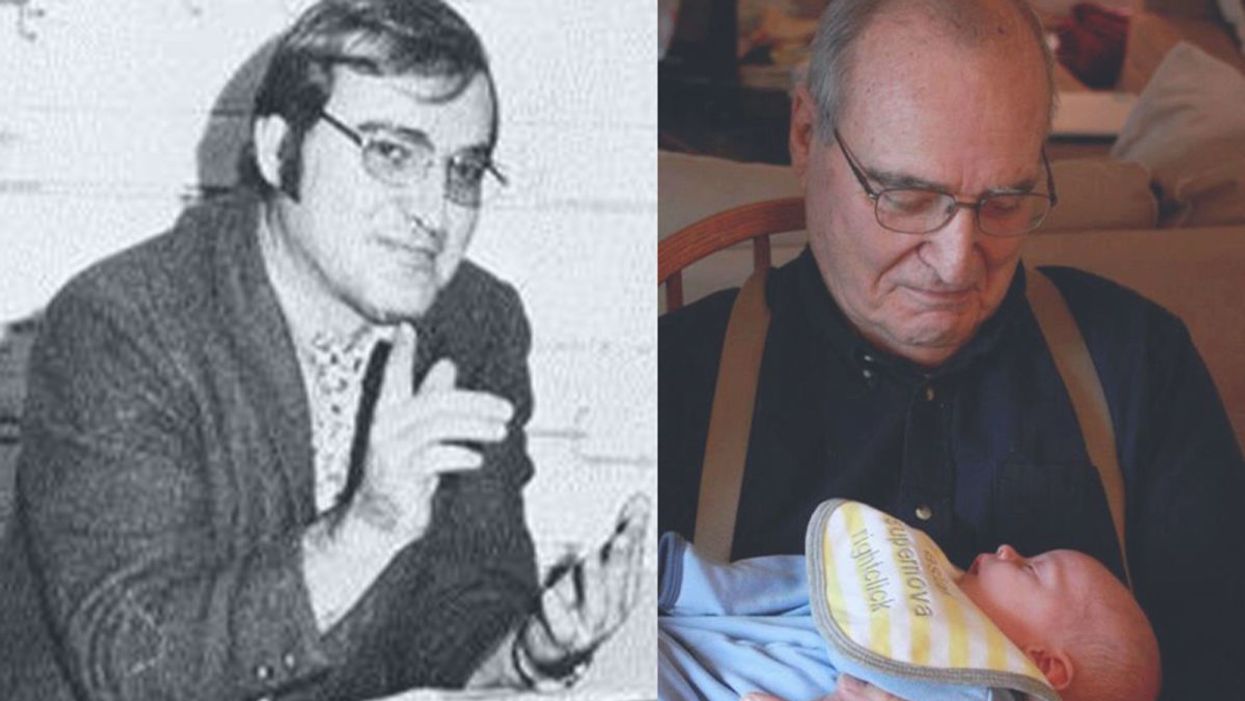
A mid-1970s photo of the author's father, and him holding a grandchild in 2012.
[Editor's Note: This piece is the winner of our 2019 essay contest, which prompted readers to reflect on the question: "How has an advance in science or medicine changed your life?"]
My father did not expect to live past the age of 50. Neither of his parents had done so. And he also knew how he would die: by heart attack, just as his father did.
In July of 1976, he had his first heart attack, days before his 40th birthday.
My dad lived the first 40 years of his life with this knowledge buried in his bones. He started smoking at the age of 12, and was drinking before he was old enough to enlist in the Navy. He had a sarcastic, often cruel, sense of humor that could drive my mother, my sister and me into tears. He was not an easy man to live with, but that was okay by him - he didn't expect to live long.
In July of 1976, he had his first heart attack, days before his 40th birthday. I was 13, and my sister was 11. He needed quadruple bypass surgery. Our small town hospital was not equipped to do this type of surgery; he would have to be transported 40 miles away to a heart center. I understood this journey to mean that my father was seriously ill, and might die in the hospital, away from anyone he knew. And my father knew a lot of people - he was a popular high school English teacher, in a town with only three high schools. He knew generations of students and their parents. Our high school football team did a blood drive in his honor.

During a trip to Disney World in 1974, Dad was suffering from angina the entire time but refused to tell me (left) and my sister, Kris.
Quadruple bypass surgery in 1976 meant that my father's breastbone was cut open by a sternal saw. His ribcage was spread wide. After the bypass surgery, his bones would be pulled back together, and tied in place with wire. The wire would later be pulled out of his body when the bones knitted back together. It would take months before he was fully healed.
Dad was in the hospital for the rest of the summer and into the start of the new school year. Going to visit him was farther than I could ride my bicycle; it meant planning a trip in the car and going onto the interstate. The first time I was allowed to visit him in the ICU, he was lying in bed, and then pushed himself to sit up. The heart monitor he was attached to spiked up and down, and I fainted. I didn't know that heartbeats change when you move; television medical dramas never showed that - I honestly thought that I had driven my father into another heart attack.
Only a few short years after that, my father returned to the big hospital to have his heart checked with a new advance in heart treatment: a CT scan. This would allow doctors to check for clogged arteries and treat them before a fatal heart attack. The procedure identified a dangerous blockage, and my father was admitted immediately. This time, however, there was no need to break bones to get to the problem; my father was home within a month.
During the late 1970's, my father changed none of his habits. He was still smoking, and he continued to drink. But now, he was also taking pills - pills to manage the pain. He would pop a nitroglycerin tablet under his tongue whenever he was experiencing angina (I have a vivid memory of him doing this during my driving lessons), but he never mentioned that he was in pain. Instead, he would snap at one of us, or joke that we were killing him.
I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count.
Being the kind of guy he was, my father never wanted to talk about his health. Any admission of pain implied that he couldn't handle pain. He would try to "muscle through" his angina, as if his willpower would be stronger than his heart muscle. His efforts would inevitably fail, leaving him angry and ready to lash out at anyone or anything. He would blame one of us as a reason he "had" to take valium or pop a nitro tablet. Dinners often ended in shouts and tears, and my father stalking to the television room with a bottle of red wine.
In the 1980's while I was in college, my father had another heart attack. But now, less than 10 years after his first, medicine had changed: our hometown hospital had the technology to run dye through my father's blood stream, identify the blockages, and do preventative care that involved statins and blood thinners. In one case, the doctors would take blood vessels from my father's legs, and suture them to replace damaged arteries around his heart. New advances in cholesterol medication and treatments for angina could extend my father's life by many years.
My father decided it was time to quit smoking. It was the first significant health step I had ever seen him take. Until then, he treated his heart issues as if they were inevitable, and there was nothing that he could do to change what was happening to him. Quitting smoking was the first sign that my father was beginning to move out of his fatalistic mindset - and the accompanying fatal behaviors that all pointed to an early death.
In 1986, my father turned 50. He had now lived longer than either of his parents. The habits he had learned from them could be changed. He had stopped smoking - what else could he do?
It was a painful decade for all of us. My parents divorced. My sister quit college. I moved to the other side of the country and stopped speaking to my father for almost 10 years. My father remarried, and divorced a second time. I stopped counting the number of times he was in and out of the hospital with heart-related issues.
In the early 1990's, my father reached out to me. I think he finally determined that, if he was going to have these extra decades of life, he wanted to make them count. He traveled across the country to spend a week with me, to meet my friends, and to rebuild his relationship with me. He did the same with my sister. He stopped drinking. He was more forthcoming about his health, and admitted that he was taking an antidepressant. His humor became less cruel and sadistic. He took an active interest in the world. He became part of my life again.
The 1990's was also the decade of angioplasty. My father explained it to me like this: during his next surgery, the doctors would place balloons in his arteries, and inflate them. The balloons would then be removed (or dissolve), leaving the artery open again for blood. He had several of these surgeries over the next decade.
When my father was in his 60's, he danced at with me at my wedding. It was now 10 years past the time he had expected to live, and his life was transformed. He was living with a woman I had known since I was a child, and my wife and I would make regular visits to their home. My father retired from teaching, became an avid gardener, and always had a home project underway. He was a happy man.

Dancing with my father at my wedding in 1998.
Then, in the mid 2000's, my father faced another serious surgery. Years of arterial surgery, angioplasty, and damaged heart muscle were taking their toll. He opted to undergo a life-saving surgery at Cleveland Clinic. By this time, I was living in New York and my sister was living in Arizona. We both traveled to the Midwest to be with him. Dad was unconscious most of the time. We took turns holding his hand in the ICU, encouraging him to regain his will to live, and making outrageous threats if he didn't listen to us.
The nursing staff were wonderful. I remember telling them that my father had never expected to live this long. One of the nurses pointed out that most of the patients in their ward were in their 70's and 80's, and a few were in their 90's. She reminded me that just a decade earlier, most hospitals were unwilling to do the kind of surgery my father had received on patients his age. In the first decade of the 21st century, however, things were different: 90-year-olds could now undergo heart surgery and live another decade. My father was on the "young" side of their patients.
The Cleveland Clinic visit would be the last major heart surgery my father would have. Not that he didn't return to his local hospital a few times after that: he broke his neck -- not once, but twice! -- slipping on ice. And in the 2010's, he began to show signs of dementia, and needed more home care. His partner, who had her own health issues, was not able to provide the level of care my father needed. My sister invited him to move in with her, and in 2015, I traveled with him to Arizona to get him settled in.
After a few months, he accepted home hospice. We turned off his pacemaker when the hospice nurse explained to us that the job of a pacemaker is to literally jolt a patient's heart back into beating. The jolts were happening more and more frequently, causing my Dad additional, unwanted pain.

My father in 2015, a few months before his death.
My father died in February 2016. His body carried the scars and implants of 30 years of cardiac surgeries, from the ugly breastbone scar from the 1970's to scars on his arms and legs from borrowed blood vessels, to the tiny red circles of robotic incisions from the 21st century. The arteries and veins feeding his heart were a patchwork of transplanted leg veins and fragile arterial walls pressed thinner by balloons.
And my father died with no regrets or unfinished business. He died in my sister's home, with his long-time partner by his side. Medical advancements had given him the opportunity to live 30 years longer than he expected. But he was the one who decided how to live those extra years. He was the one who made the years matter.
Short-Term Suspended Animation for Humans Is Coming Soon
A man gasps for air through deep ice, in a symbolic representation of human hibernation through induced hypothermia.
At 1 a.m., Tony B. is flown to a shock trauma center of a university hospital. Five minutes earlier, he was picked up unconscious with no blood pressure, having suffered multiple gunshot wounds with severe blood loss. Standard measures alone would not have saved his life, but on the helicopter he was injected with ice-cold fluids intravenously to begin cooling him from the inside, and given special drugs to protect his heart and brain.
Suspended animation is not routine yet, but it's going through clinical trials at the University of Maryland and the University of Pittsburgh.
A surgeon accesses Tony's aorta, allowing his body to be flushed with larger amounts of cold fluids, thereby inducing profound hypothermia -- a body temperature below 10° C (50° F). This is suspended animation, a form of human hibernation, but officially the procedure is called Emergency Preservation and Resuscitation for Cardiac Arrest from Trauma (EPR-CAT).
This chilly state, which constitutes the preservation component of Tony's care, continues for an hour as surgeons repair injuries and connect his circulation to cardiopulmonary bypass (CPB). This allows blood to move through the brain delivering oxygen at low doses appropriate for the sharply reduced metabolic rate that comes with the hypothermia, without depending on the heart and lungs. CPB also enables controlled, gradual re-warming of Tony's body as fluid and appropriate amounts of red blood cells are transfused into him.
After another hour or so, Tony's body temperature reaches the range of 32-34° C (~90-93° F), called mild hypothermia. Having begun the fluid resuscitation process already, the team stops warming Tony, switches his circulation from CPB to his own heart and lungs, and begins cardiac resuscitation with electrical jolts to his heart. With his blood pressure stable, his heart rate slow but appropriate for the mild hypothermia, Tony is maintained at this intermediate temperature for 24 hours; this last step is already standard practice in treatment of people who suffer cardiac arrest without blood loss trauma.
The purpose is to prevent brain damage that might come with the rapid influx of too much oxygen, just as a feast would mean death to a starvation victim. After he is warmed to a normal temperature of 37° C (~99° F), Tony is awakened and ultimately recovers with no brain damage.
Tony's case is fictional; EPR-CAT is not routine yet, but it's going through clinical trials at the University of Maryland and the University of Pittsburgh, under the direction of trauma surgeon Dr. Samuel Tisherman, who spent many years developing the procedure in dogs and pigs. In such cases, patients undergo suspended animation for a couple of hours at most, but other treatments are showing promise in laboratory animals, like the use of hydrogen sulfide gas without active cooling to induce suspended animation in mice. Such interventions could ultimately fuse with EPR-CAT, sending the new technology further into what's still the realm of science fiction – at least for now.
Consider the scenario of a 5-year-old girl diagnosed with a progressive, incurable, terminal disease.
Experts say that extended suspended animation – cooling patients in a stable state for months or years -- could be possible at some point, although no one can predict when the technology will be clinical reality, since hydrogen sulfide and other chemical tactics would have to move into clinical use in humans and prove safe and effective in combination with EPR-CAT, or with a similar cooling approach.
How Could Long-Term Suspended Animation Impact Humanity?
Consider the scenario of a 5-year-old girl diagnosed with a progressive, incurable, terminal disease. Since available treatments would only lengthen the projected survival by a year, she is placed into suspended animation. She is revived partially every few years, as new treatments become available that can have a major impact on her disease. After 35 years of this, she is revived completely as treatments are finally adequate to cure her condition, but biologically she has aged only a few months. Physically, she is normal now, though her parents are in their seventies, and her siblings are grown and married.
Such hypothetical scenarios raise many issues: Where will the resources come from to take care of patients for that long? Who will pay? And how will patients adapt when they emerge into a completely different world?
"Heavy resource utilization is a factor if you've got people hibernating for years or decades," says Bradford Winters, an associate professor of anesthesiology and critical care medicine, and assistant professor of neurological surgery at Johns Hopkins.
Conceivably, special high-tech facilities with robots and artificial intelligence watching over the hibernators might solve the resource issue, but even then, Winters notes that long-term hibernation would entail major disparities between the wealthy and poor. "And then there is the psychological effect of being disconnected from one's family and society for a generation or more," he says. "What happens to that 5-year-old waking to her retired parents and married siblings? Will her younger sister adopt her? What would that be like?"
Probably better than dying is one answer.
Back on Earth, human hibernation would raise daunting policy questions that may take many years to resolve.
Outside of medicine, one application of human hibernation that has intrigued generations of science fiction writers is in long-duration space travel. During a voyage lasting years or decades, space explorers or colonists not only could avoid long periods of potential boredom, but also the aging process. Considering that the alternative to "sleeper ships" would be multi-generation starships so large that they'd be like small worlds, human hibernation in spaceflight could become an enabling technology for interstellar flight.
Big Questions: It's Not Too Early to Ask
Back on Earth, the daunting policy questions may take many years to resolve. Society ought to be aware of them now, before human hibernation technology outpaces its dramatic implications.
"Our current framework of ethical and legal regulation is adequate for cases like the gunshot victim who is chilled deeply for a few hours. Short-term cryopreservation is currently part of the continuum of care," notes David N. Hoffman, a clinical ethicist and health care attorney who teaches at Columbia University, and at Yeshiva University's Benjamin N. Cardozo School of Law and Albert Einstein College of Medicine.
"But we'll need a new framework when there's a capability to cryopreserve people for many years and still bring them back. There's also a legal-ethical issue involving the parties that decide to put the person into hibernation versus the patient wishes in terms of what risk benefit ratio they would accept, and who is responsible for the expense and burdens associated with cases that don't turn out just right?"
To begin thinking about practical solutions, Hoffman characterizes long-term human hibernation as an extension of the ethics of cyro-preserved embryos that are held for potential parents, often for long periods of time. But the human hibernation issue is much more complex.
"The ability of the custodian and patient to enter into a meaningful and beneficial arrangement is fraught, because medical advances necessary to address the person's illness or injury are -- by definition -- unknown," says Hoffman. "It means that you need a third party, a surrogate, to act on opportunities that the patient could never have contemplated."
Such multigenerational considerations might become more manageable, of course, in an era when gene therapy, bionic parts, and genetically engineered replacement organs enable dramatic life extension. But if people will be living for centuries regardless of whether or not they hibernate, then developing the medical technology may be the least of the challenges.
The Mind-Blowing Promise of Neural Implants
A patient with an implanted neural device that connects to a prosthetic arm can sense, while blindfolded, which of the mechanical fingers are being touched.
You may not have heard of DARPA, the research branch of the Pentagon. But you're definitely familiar with some of the technology it has pioneered, like the Internet, Siri, and handheld GPS.
"Now we're going to try to go from this proof-of-concept all the way to commercial technologies that can powerfully affect patients' lives."
Last week in National Harbor, Maryland, DARPA celebrated its 60th anniversary by showcasing its latest breakthroughs and emerging research programs, one of which centers around using neurotechnology to enhance the capabilities of the human brain. This technology is initially being developed to help warfighters and veterans, but its success could have enormous implications for civilian patients and, eventually, mainstream consumers.
The field is moving ahead rapidly. Fifteen years ago, a monkey named Aurora used a brain-machine interface to control a cursor on a computer screen. In 2014, DARPA's mind-controlled prosthetic arm for amputees won approval from the Food and Drug Administration.
Since then, DARPA has continued to push neurotechnology to new heights. Here are three of their research programs that are showing promise in early human testing:
1) A NEURAL IMPLANT HELP MANAGE PSYCHIATRIC ILLNESS
More than 2.2 million veterans and 44 million civilians are living with some form of psychiatric illness, and medications don't work for everyone. DARPA set out to create new options for people living with debilitating anxiety, depression, and PTSD.
"We can get somebody back to normal. It's a whole new set of tools for physicians," said Justin Sanchez, Director of the Biological Technologies Office at DARPA.
He told the audience about a woman living with both epilepsy and extreme anxiety, who has a direct neural interface that reads her brain's signals in real time and can be modulated with stimulation. He shared a recent video of her testing the device:
"Now we're going to try to go from this proof-of-concept all the way to commercial technologies that can powerfully affect patients' lives," Sanchez said.
2) A NEURAL IMPLANT TO HELP IMPROVE MEMORY
"We are right at the cusp" of improving memory recall with direct neural interfaces, Sanchez said.
All day long, our brains shift between poor and good memory states. A brain-computer interface can read the signals of populations of neurons in the lateral temporal cortex. The device continuously monitors the state of the brain and delivers stimulation within a fraction of a second after detecting a poor memory state, to improve the person's memory performance.
The improved memory lasts only seconds, so the system "delivers stimulation as needed in a closed loop to keep the performance in a good state, because of this natural variability of performance," said Dan Rizzuto, founder of NiaTherapeutics, whose technology was developed with support from DARPA and the United States BRAIN Initiative.
Check out this recently shot video of a patient testing the device, which Sanchez called "a breakthrough moment":
About 400 patients have been tested with this technology so far. In a pilot study whose data have not yet been published, patients with traumatic brain injury showed improvement in recall of around 28 percent, according to Rizzuto.
He estimates that potential FDA approval of the device for patients with traumatic brain injury is still 7 to 8 years away. The technology holds the potential to help many other kinds of patients as well.
"We believe this device could also be used to treat Alzheimer's because it's not specific to any brain pathology but based on a deep understanding of the way human memory works," Rizzuto said.
3) A NEURAL IMPLANT TO REVOLUTIONIZE PROSTHETICS FOR WARFIGHTERS AND VETERANS
Since 2006, DARPA has run a program to revolutionize prosthetics. The latest advances allow amputees to actually feel again with their bionic limbs.
Sensors in a prosthetic hand relay information to an interface in the brain that allows the person to detect which of their "fingers" are being touched, while their eyes are closed:
WHAT COMES NEXT?
DARPA is now turning its attention to non-surgical, non-invasive neurotechnology. Researchers hope to use advanced sensor technology to detect signals from neurons without putting any electrodes directly inside the brain. Under the direction of program manager Dr. Al Emondi, the N³ program is about to launch soon and plans to run for four or five years.
"We haven't even scratched the surface of what a human brain's capability is," said Dr. Geoffrey Ling, the Founding Director of the Biological Technologies Office. "When we can make this a non-invasive consumer technology, this will explode. It will take on a life of its own."
Then, inevitably, the hard questions will follow.
As Sanchez put it: "Will society consider some form of neural enhancement a personal choice like braces? Could there be a disturbing gap for people who have neurotech and those who don't? We must come together and all think over the horizon. How the story unfolds ultimately depends on all of us."
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

