How Bacteria-Killing Viruses May Save Us From Antibiotic Resistance
Dr. Adalja is focused on emerging infectious disease, pandemic preparedness, and biosecurity. He has served on US government panels tasked with developing guidelines for the treatment of plague, botulism, and anthrax in mass casualty settings and the system of care for infectious disease emergencies, and as an external advisor to the New York City Health and Hospital Emergency Management Highly Infectious Disease training program, as well as on a FEMA working group on nuclear disaster recovery. Dr. Adalja is an Associate Editor of the journal Health Security. He was a coeditor of the volume Global Catastrophic Biological Risks, a contributing author for the Handbook of Bioterrorism and Disaster Medicine, the Emergency Medicine CorePendium, Clinical Microbiology Made Ridiculously Simple, UpToDate's section on biological terrorism, and a NATO volume on bioterrorism. He has also published in such journals as the New England Journal of Medicine, the Journal of Infectious Diseases, Clinical Infectious Diseases, Emerging Infectious Diseases, and the Annals of Emergency Medicine. He is a board-certified physician in internal medicine, emergency medicine, infectious diseases, and critical care medicine. Follow him on Twitter: @AmeshAA

Hand-counting bacteriophage plaques during a titer test.
In my hometown of Pittsburgh, it is not uncommon to read about cutting-edge medical breakthroughs, because Pittsburgh is the home of many innovations in medical science, from the polio vaccine to pioneering organ transplantation. However, medical headlines from Pittsburgh last November weren't heralding a new discovery for once. They were carrying a plea—for a virus.
Phages are weapons of bacterial destruction, but despite recognition of their therapeutic potential for over 100 years, there are zero phage products commercially available to medicine in the United States.
Specifically, a bacteria-killing virus that could attack and control a certain highly drug-resistant bacterial infection ravaging the newly transplanted lungs of a 25-year-old woman named Mallory Smith. The culprit bacteria, Burkholderia cepacia, is a notoriously vicious bacterium that preys on patients with cystic fibrosis who, throughout their life, are exposed to course after course of antibiotics, often fostering a population of highly resistant bacteria that can become too formidable for modern medicine to combat.
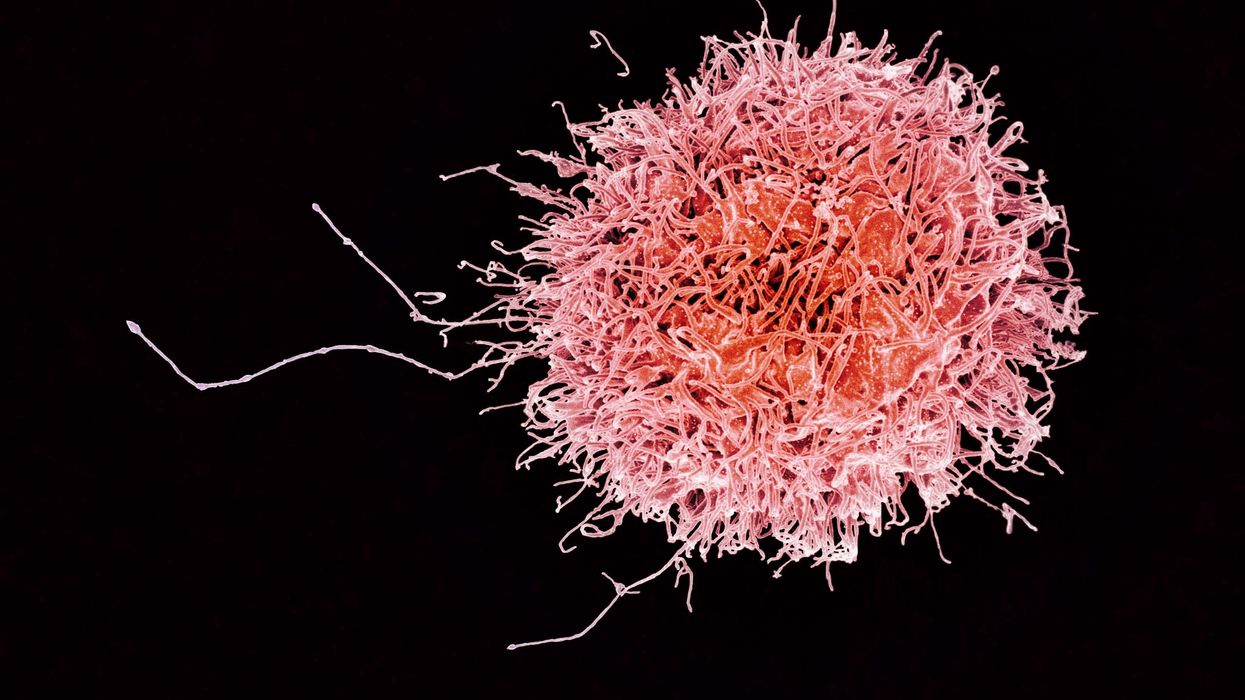
What Smith and her physicians desperately needed was a tool that would move beyond failed courses of antibiotics. What they sought was called a bacteriophage. These are naturally occurring ubiquitous viruses that target not humans, but bacteria. The world literally teems with "phages" and one cannot take a bite or drink of anything without encountering them. These weapons of bacterial destruction are exquisitely evolved to target bacteria and, as such, are not harmful to humans. However, despite recognition of their therapeutic potential for over 100 years, there are zero bacteriophage products commercially available to medicine in the United States, at a time when antibiotic resistance is arguably our most pressing public health crisis. Just this week, a new study was published in the Proceedings of the National Academy of Sciences detailing the global scope of the problem.
Why Were These Promising Tools Forgotten?
Phages weren't always relegated to this status. In fact, in the early 20th century phages could be found on American drug store shelves and were used for a variety of ailments. However, the path-breaking discovery and development of antimicrobials agents such as the sulfa drugs and, later the antibiotic penicillin, supplanted the world of phage therapeutics in the United States and many other places.
Fortunately, phage therapy never fully disappeared, and research and clinical use continued in Eastern European nations such as Georgia and Poland.
The antibiotic age revolutionized medicine in a way that arguably no other innovation has. Not only did antibiotics tame many once-deadly infectious diseases, but they made much of modern medicine – from cancer chemotherapy to organ transplantation to joint replacement – possible. Antibiotics, unlike the exquisitely evolved bacteriophage, possessed a broader spectrum of activity and were active against a range of bacteria. This non-specificity facilitated antibiotic use without the need for a specific diagnosis. A physician does not need to know the specific bacterial genus and species causing, for example, a skin infection or pneumonia, but can select an antibiotic that covers the likely culprits and use it empirically, fully expecting the infection to be controlled. Unfortunately, this non-specificity engendered the overuse of antibiotics whose consequences we are now suffering. A bacteriophage, on the other hand, will work against one specific bacterial species and is evolved for just that role.
Phages to the Rescue
As the march of antibiotic resistance has predictably continued since the dawn of the antibiotic age, the prospect of resurrecting phage therapy has been increasingly viewed as one solution. Fortunately, phage therapy never fully disappeared, and research and clinical use continued in Eastern European nations such as Georgia and Poland. However, much of that experience has remained opaque to the medical community at large and questions about dosage, toxicity, efficacy, and method of delivery left many questions without full answers.
Though real questions remained regarding phage use, dire circumstances of prolific antibiotic resistance necessitated their use in the U.S. in two prominent instances involving life-threatening infections. The first case involved an Acinetobacter baumanii infection of the pancreas in a San Diego man in which phages were administered intravenously in 2016. The other case, also in 2016, involved the instillation of phages, fished out of a pond, into the chest cavity of man with a Pseudmonas aeruginosa infection of a prosthetic graft of the aorta. Both cases were successful and were what fueled the Pittsburgh-based plea for Burkholderia phages.
The phages you begin with may not be the ones you end up with, as Darwinian evolutionary pressures will alter the phage in order to keep up with the ongoing evolution of its bacterial target.
How Phages Differ from Other Medical Products
It might seem surprising that in light of the urgent need for new treatments for drug-resistant infections, the pharmaceutical armamentarium is not teeming with phages like a backyard pond. However, phages have been difficult to fit into the current regulatory framework that operates in most developed countries such as the U.S. because of their unique characteristics.
Phages are not one homogenous product like a tablet of penicillin, but a cocktail of viruses that change and evolve as they replicate. The phages you begin with may not be the ones you end up with, as Darwinian evolutionary pressures will alter the phage in order to keep up with the ongoing evolution of its bacterial target. The cocktail may not just contain one specific phage, but a range of phages that all target some specific bacteria in order to increase efficacy. These phage cocktails might also need adjusting to keep pace with bacterial resistance. Additionally, the concentration of phage in a human body after administration is not so easy to predict as phage numbers will rise and fall based on the number of target bacteria that are present.
All of these characteristics make phages very unique when viewed through a regulatory lens, and necessitate the creation of new methods to evaluate them, given that regulatory approval is required. Using phages in the U.S. now requires FDA permission through an investigational new drug application, which can be expedited during an emergency situation. FDA scientists are actively involved in understanding the best means to evaluate bacteriophage therapy and several companies are in early-stage development, though no major clinical trials in the U.S. are currently underway.
One FDA-approved application of phages has seen them used on food products at delis and even in slaughterhouses to diminish the quantity of bacteria on certain meat products.
Would That Humans Were As Lucky As Bologna
Because of the regulatory difficulties with human-use approval, some phage companies have taken another route to develop phage products: food safety. Food safety is a major public health endeavor, and keeping food that people consume safe from E.coli, Listeria, and Salmonella, for example, are rightfully major priorities of industry. One FDA-approved application of phages has seen them used on food products at delis and even in slaughterhouses to diminish the quantity of bacteria on certain meat products.
This use, unlike that for human therapeutic purposes, has found success with regulators: phages, not surprisingly, have been granted the "generally regarded as safe (GRAS)" designation.
A Phage Directory
Tragically Mallory Smith succumbed to her infection despite getting a dose of phages culled from sludge in the Philippines and Fiji. However, her death and last-minute crusade to obtain phages has prompted the call for a phage directory. This directory could catalog the various phages being studied and the particular bacteria they target. Such a searchable index will facilitate the rapid identification and – hopefully – delivery of phages to patients.
If phage therapy is to move from a last-ditch emergency measure to a routine tool for infectious disease physicians, it will be essential that the hurdles they face are eliminated.
Moving Beyond Antibiotics
As we move increasingly toward a post-antibiotic age in infectious disease, moving outside of the traditional paradigm of broad-spectrum antibiotics to non-traditional therapeutics such as bacteriophages and other novel products will become increasingly necessary. Already, clinical trials are underway in various populations, including a major trial in European burn patients.
It is important to understand that there are important scientific and therapeutic questions regarding dose, route of administration and other related questions that need to be addressed before phage use becomes more routine, and it is only through clinical trials conducted with the hope of eventual commercialization that these answers will be found. If phage therapy is to move from a last-ditch emergency measure to a routine tool for infectious disease physicians, it will be essential that the hurdles they face are eliminated.
Dr. Adalja is focused on emerging infectious disease, pandemic preparedness, and biosecurity. He has served on US government panels tasked with developing guidelines for the treatment of plague, botulism, and anthrax in mass casualty settings and the system of care for infectious disease emergencies, and as an external advisor to the New York City Health and Hospital Emergency Management Highly Infectious Disease training program, as well as on a FEMA working group on nuclear disaster recovery. Dr. Adalja is an Associate Editor of the journal Health Security. He was a coeditor of the volume Global Catastrophic Biological Risks, a contributing author for the Handbook of Bioterrorism and Disaster Medicine, the Emergency Medicine CorePendium, Clinical Microbiology Made Ridiculously Simple, UpToDate's section on biological terrorism, and a NATO volume on bioterrorism. He has also published in such journals as the New England Journal of Medicine, the Journal of Infectious Diseases, Clinical Infectious Diseases, Emerging Infectious Diseases, and the Annals of Emergency Medicine. He is a board-certified physician in internal medicine, emergency medicine, infectious diseases, and critical care medicine. Follow him on Twitter: @AmeshAA
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
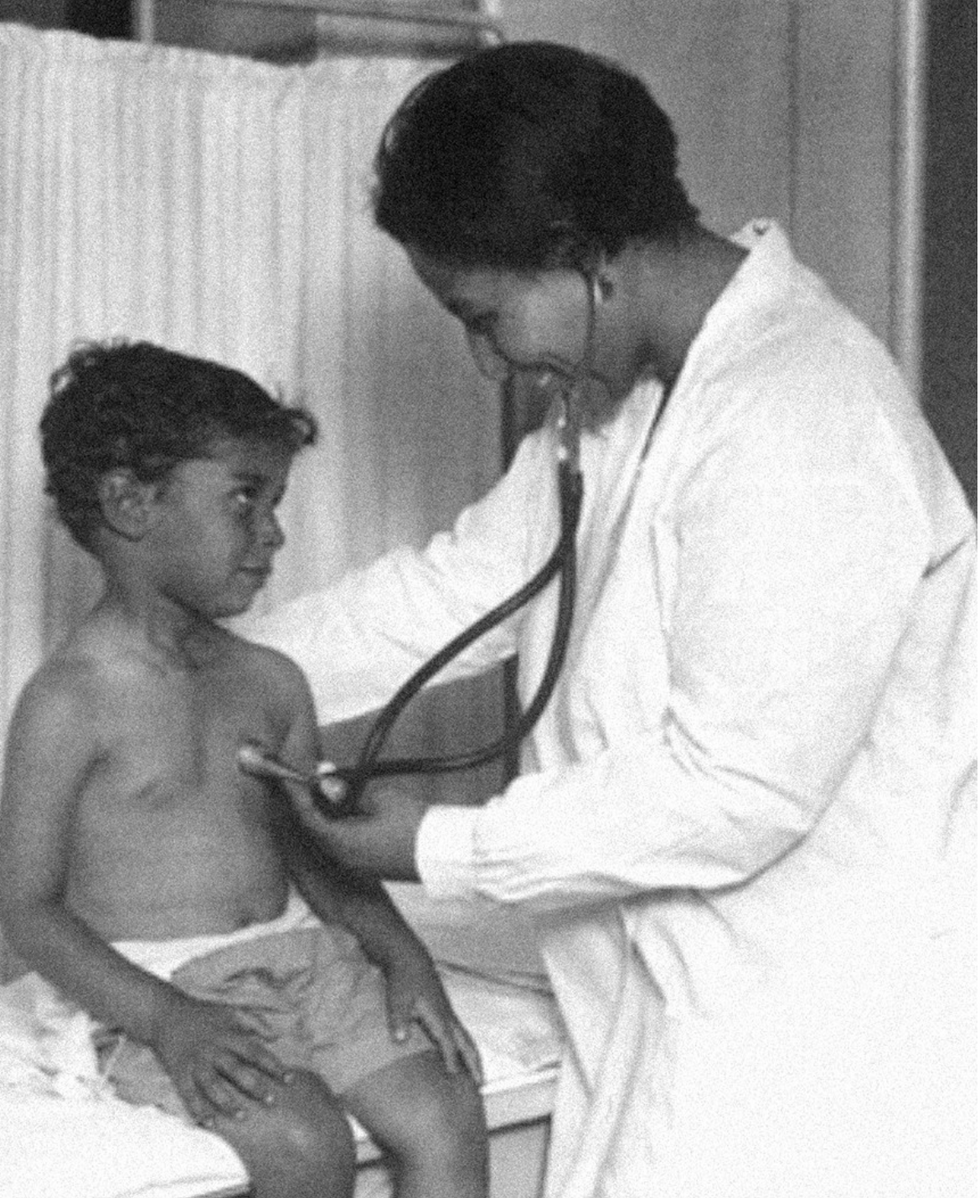
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business