How mRNA Could Revolutionize Medicine

In November 2020, messenger RNA catapulted into the public consciousness when the first COVID-19 vaccines were authorized for emergency use. Around the same time, an equally groundbreaking yet relatively unheralded application of mRNA technology was taking place at a London hospital.
Over the past two decades, there's been increasing interest in harnessing mRNA — molecules present in all of our cells that act like digital tape recorders, copying instructions from DNA in the cell nucleus and carrying them to the protein-making structures — to create a whole new class of therapeutics.
Scientists realized that artificial mRNA, designed in the lab, could be used to instruct our cells to produce certain antibodies, turning our bodies into vaccine-making factories, or to recognize and attack tumors. More recently, researchers recognized that mRNA could also be used to make another groundbreaking technology far more accessible to more patients: gene editing. The gene-editing tool CRISPR has generated plenty of hype for its potential to cure inherited diseases. But delivering CRISPR to the body is complicated and costly.
"Most gene editing involves taking cells out of the patient, treating them and then giving them back, which is an extremely expensive process," explains Drew Weissman, professor of medicine at the University of Pennsylvania, who was involved in developing the mRNA technology behind the COVID-19 vaccines.
But last November, a Massachusetts-based biotech company called Intellia Therapeutics showed it was possible to use mRNA to make the CRISPR system inside the body, eliminating the need to extract cells out of the body and edit them in a lab. Just as mRNA can instruct our cells to produce antibodies against a viral infection, it can also teach them to produce one of the two components that make up CRISPR — a cutting protein that snips out a problem gene.
"The pandemic has really shown that not only are mRNA approaches viable, they could in certain circumstances be vastly superior to more traditional technologies."
In Intellia's London-based clinical trial, the company applied this for the first time in a patient with a rare inherited liver disease known as hereditary transthyretin amyloidosis with polyneuropathy. The disease causes a toxic protein to build up in a person's organs and is typically fatal. In a company press release, Intellia's president and CEO John Leonard swiftly declared that its mRNA-based CRISPR therapy could usher in a "new era of potential genome editing cures."
Weissman predicts that turning CRISPR into an affordable therapy will become the next major frontier for mRNA over the coming decade. His lab is currently working on an mRNA-based CRISPR treatment for sickle cell disease. More than 300,000 babies are born with sickle cell every year, mainly in lower income nations.
"There is a FDA-approved cure, but it involves taking the bone marrow out of the person, and then giving it back which is prohibitively expensive," he says. It also requires a patient to have a matched bone marrow done. "We give an intravenous injection of mRNA lipid nanoparticles that target CRISPR to the bone marrow stem cells in the patient, which is easy, and much less expensive."
Cancer Immunotherapy
Meanwhile, the overwhelming success of the COVID-19 vaccines has focused attention on other ways of using mRNA to bolster the immune system against threats ranging from other infectious diseases to cancer.
The practicality of mRNA vaccines – relatively small quantities are required to induce an antibody response – coupled with their adaptable design, mean companies like Moderna are now targeting pathogens like Zika, chikungunya and cytomegalovirus, or CMV, which previously considered commercially unviable for vaccine developers. This is because outbreaks have been relatively sporadic, and these viruses mainly affect people in low-income nations who can't afford to pay premium prices for a vaccine. But mRNA technology means that jabs could be produced on a flexible basis, when required, at relatively low cost.
Other scientists suggest that mRNA could even provide a means of developing a universal influenza vaccine, a goal that's long been the Holy Grail for vaccinologists around the world.
"The mRNA technology allows you to pick out bits of the virus that you want to induce immunity to," says Michael Mulqueen, vice president of business development at eTheRNA, a Belgium-based biotech that's developing mRNA-based vaccines for malaria and HIV, as well as various forms of cancer. "This means you can get the immune system primed to the bits of the virus that don't vary so much between strains. So you could actually have a single vaccine that protects against a whole raft of different variants of the same virus, offering more universal coverage."
Before mRNA became synonymous with vaccines, its biggest potential was for cancer treatments. BioNTech, the German biotech company that collaborated with Pfizer to develop the first authorized COVID-19 vaccine, was initially founded to utilize mRNA for personalized cancer treatments, and the company remains interested in cancers ranging from melanoma to breast cancer.
One of the major hurdles in treating cancer has been the fact that tumors can look very different from one person to the next. It's why conventional approaches, such as chemotherapy or radiation, don't work for every patient. But weaponizing mRNA against cancer primes the immune cells with the tumor's specific genetic sequence, training the patient's body to attack their own unique type of cancer.
"It means you're able to think about personalizing cancer treatments down to specific subgroups of patients," says Mulqueen. "For example, eTheRNA are developing a renal cell carcinoma treatment which will be targeted at around 20% of these patients, who have specific tumor types. We're hoping to take that to human trials next year, but the challenge is trying to identify the right patients for the treatment at an early stage."
Repairing Damaged mRNA
While hopes are high that mRNA could usher in new cancer treatments and make CRISPR more accessible, a growing number of companies are also exploring an alternative to gene editing, known as RNA editing.
In genetic disorders, the mRNA in certain cells is impaired due to a rogue gene defect, and so the body ceases to produce a particular vital protein. Instead of permanently deleting the problem gene with CRISPR, the idea behind RNA editing is to inject small pieces of synthetic mRNA to repair the existing mRNA. Scientists think this approach will allow normal protein production to resume.
Over the past few years, this approach has gathered momentum, as some researchers have recognized that it holds certain key advantages over CRISPR. Companies from Belgium to Japan are now looking at RNA editing to treat all kinds of disorders, from Huntingdon's disease, to amyotrophic lateral sclerosis, or ALS, and certain types of cancer.
"With RNA editing, you don't need to make any changes to the DNA," explains Daniel de Boer, CEO of Dutch biotech ProQR, which is looking to treat rare genetic disorders that cause blindness. "Changes to the DNA are permanent, so if something goes wrong, that may not be desirable. With RNA editing, it's a temporary change, so we dose patients with our drugs once or twice a year."
Last month, ProQR reported a landmark case study, in which a patient with a rare form of blindness called Leber congenital amaurosis, which affects the retina at the back of the eye, recovered vision after three months of treatment.
"We have seen that this RNA therapy restores vision in people that were completely blind for a year or so," says de Boer. "They were able to see again, to read again. We think there are a large number of other genetic diseases we could go after with this technology. There are thousands of different mutations that can lead to blindness, and we think this technology can target approximately 25% of them."
Ultimately, there's likely to be a role for both RNA editing and CRISPR, depending on the disease. "I think CRISPR is ideally suited for illnesses where you would like to permanently correct a genetic defect," says Joshua Rosenthal of the Marine Biology Laboratory in Chicago. "Whereas RNA editing could be used to treat things like pain, where you might want to reset a neural circuit temporarily over a shorter period of time."
Much of this research has been accelerated by the COVID-19 pandemic, which has played a major role in bringing mRNA to the forefront of people's minds as a therapeutic.
"The pandemic has really shown that not only are mRNA approaches viable, they could in certain circumstances be vastly superior to more traditional technologies," says Mulqueen. "In the future, I would not be surprised if many of the top pharma products are mRNA derived."
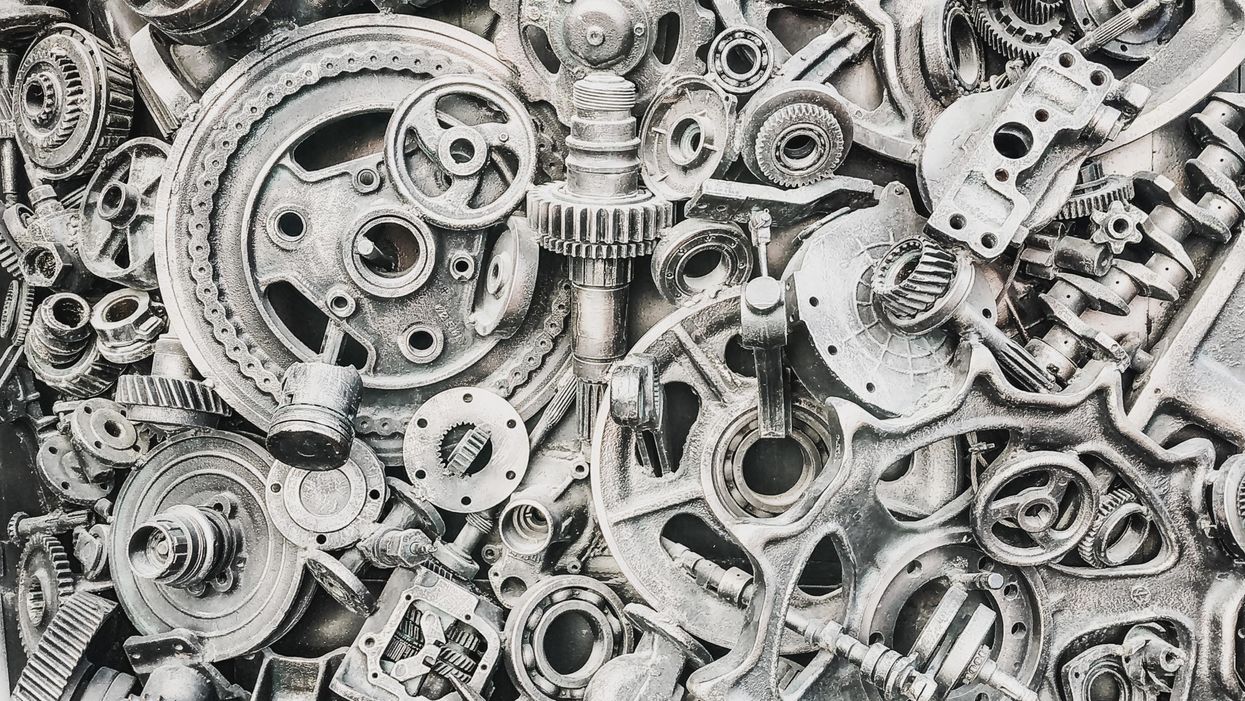
Two students had an idea at a scrapyard. They went on to "upcycle" 80,000 airbags, 100,000 seatbelts and 28,000 belt buckles – the equivalent of 60 tons of car trash
Luckily, two college freshmen at the Rotterdam School of Management, Erasmus University, were naïve enough to take their bicycles to the scrapyard. In a previous stroke of fortune, the freshmen, Adrian Goosses and Michael Widmann, had been assigned as roommates and had quickly hit it off. Now they were looking for a cool recycling project for their first semester “strategic entrepreneurship” course—maybe they could turn old tires into comfortable lounge chairs, they thought.
“Everybody gets around by bike in Rotterdam,” says Goosses, now 32, from his home in Cologne, Germany. “The tires were way too heavy and cumbersome to transport by bike,” Widmann chimes in via Zoom from Bolzano, Italy, where he lives.
Sifting through the car trash for something handier led the two students to an idea that has since flourished: Could the airbag and seatbelts from a banged up compact car be salvaged and turned into a sustainable backpack? The size of the airbag was already a natural fit. The seatbelts made perfect shoulder straps. After returning from the scrapyard, “We stitched the prototype together by hand with a needle and yarn,” says Goosses. “Yet we didn’t even know how to sew!”
Much to their surprise, their classmates responded with so much enthusiasm to their “trash bag” concept that it convinced the two innovators to keep going. Every semester, they improved the prototype further. With the help of YouTube videos, they taught themselves how to sew. Because modern electric sewing machines had a difficult time breaking through the tough nylon of the airbags, Goosses and Widmann went to a second-hand shop and purchased an ancient Singer from 1880 for 10 Euros. They dyed the first airbags in a saucepan in the garden outside of the apartment they shared.
“By the time we graduated, we had a presentable prototype and a business plan,” Goosses says.
Despite their progress, Goosses and Widmann are up against a problem that’s immense: Cars are notoriously difficult to recycle because many parts are considered toxic waste.
It’s an example of “upcycling,” when you spot a potential new use in something that’s been trashed, shelved or otherwise retired. The approach has received increasing attention and support from the U.S. Environmental Protection Agency and others to boost sustainability in all kinds of areas, from fashion (where even luxury brands like Balenciaga or Coach repurpose vintage clothing and bags) to architecture, where reusing wood, steel and bricks significantly reduces a building’s carbon footprint.
In addition to helping the planet, those who do it well can make a living from it. These days, Goosses and Widmann own a flourishing company: Airpaq. A crowdfunding campaign in 2017 yielded 70,000 Euros to get them started. Since then, they have upcycled 80,000 airbags, 100,000 seatbelts and 28,000 belt buckles – the equivalent of 60 tons of car trash.
For the successful upcycling, they received the 2021 German Design Award and, earlier this year, the renowned German Sustainability Award. The jurors evaluating the product commented that the startup “convinced us not only because of their uncompromising quality and functionality but also because of their ecological and ethical values….How well the startup translates upcycling and green fashion into an urban lifestyle brand is impressive.”
Despite their progress, Goosses and Widmann are up against a problem that’s immense: Cars are notoriously difficult to recycle because many parts are considered toxic waste. Therefore, up to 25% of vehicle scraps get shredded every year in Germany alone, the equivalent of over 501,000 tons. Because airbags and seatbelts are nearly indestructible, they are costly to recycle and almost always end up in landfills. Given that airbags and seatbelts save lives, they are subject to stringent security regulations, and manufacturers have a sky-high reject rate. “If a tiny filament protrudes somewhere, the manufacturer will throw out the entire output,” Widmann explains.
The nearly indestructible qualities that make this material very difficult to recycle render it an excellent resource for backpacks. “The material is so durable, you almost cannot tear it,” Goosses adds and demonstrates with a hard tug that even when the material already has a hole, it won’t rip it further. The material is also water repellent and extremely light.
The antique Singer is still in their Cologne headquarters but only as decoration. Their company with 12 employees is producing 500 backpacks and fanny packs every week in Romania, where the parts are professionally cut by laser, dyed and sewed. Airpaq still procures the belt buckles at scrapyards but they get most of the airbags directly from the reject pile of a nearby airbag producer. “We process the materials where they are produced,” Goosses explains. Only about 15 miles lie between one of Europe’s biggest airbag manufacturers and the Airpaq seamsters in Romania.

Co-founders Adrian Goosses and Michael Widmann demonstrate their company's equation: airbag plus seatbelt equals a backpack that's durable and eco-friendly.
Airpaq
The founders are aware that with price tags ranging from 100 to 160 Euro - a cost that reflects their intensive production process - Airpaq’s bags are hardly competitive. After all, anybody can buy a discount backpack for a fraction of the cost. So they recently added fanny packs for 30 Euro to their product line. Goosses and Widmann know they will need to lower their prices in the long run if they want to expand. Among other things, they didn’t pay themselves salaries during the first two years after founding the company.
Money-making isn’t their only objective. “Of course, it would be cheaper if we did what almost all textile producers do and move production to Asia,” Goosses says. That wasn’t an option for him. “Ship trash to Vietnam and let seamsters sew it together for cheap? No way, that would be anything but sustainable,” he says.
Michael Widmann’s family was already operating a textile production in Romania, mainly producing thin, elastic sports fashion. The family allowed Widmann and Goosses to produce their first professional prototypes there, but then the two youngsters had to buy their own machines, acquire the necessary knowhow, and hire their staff. They both moved to Romania for six months “to get to know the people behind the machines.” The founders emphasize that they pay fair wages, use eco-certified dyes and clean their own wastewater. “Normal production uses five to six liters of water per kilo material,” Widmann explains. “We only need a fraction because we massage the dye into the material by hand: 100 ml water for washing and dying per kilo.”
However, every time they return to the scrapyard, the abundance of trash sparks new ideas. “When you see how much material ends up there…” Widmann says, shaking his head without finishing the sentence. Goosses picks up the train of thought: “We want to make upcycling the new standard. You just have to be creative to get upcycling into the mainstream.”
And maybe they’ll return to their roots and finally find an idea for the tires after all. “One could turn the rubber into soles for comfortable shoes,” Widmann thinks out loud.
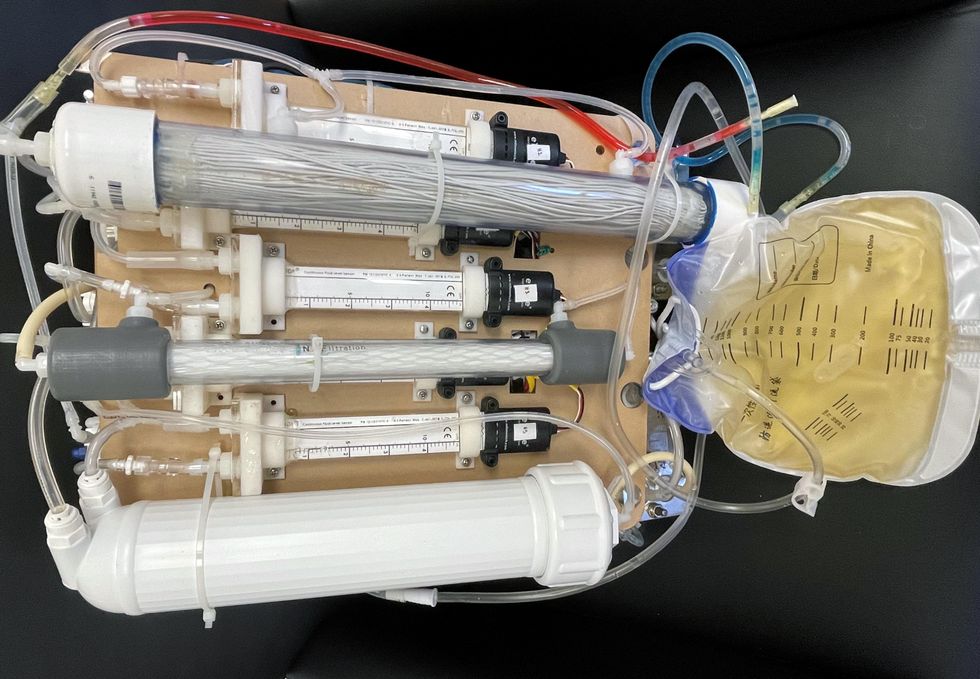
Recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now
Like all those whose kidneys have failed, Scott Burton’s life revolves around dialysis. For nearly two decades, Burton has been hooked up (or, since 2020, has hooked himself up at home) to a dialysis machine that performs the job his kidneys normally would. The process is arduous, time-consuming, and expensive. Except for a brief window before his body rejected a kidney transplant, Burton has depended on machines to take the place of his kidneys since he was 12-years-old. His whole life, the 39-year-old says, revolves around dialysis.
“Whenever I try to plan anything, I also have to plan my dialysis,” says Burton says, who works as a freelance videographer and editor. “It’s a full-time job in itself.”
Many of those on dialysis are in line for a kidney transplant that would allow them to trade thrice-weekly dialysis and strict dietary limits for a lifetime of immunosuppressants. Burton’s previous transplant means that his body will likely reject another donated kidney unless it matches perfectly—something he’s not counting on. It’s why he’s enthusiastic about the development of artificial kidneys, small wearable or implantable devices that would do the job of a healthy kidney while giving users like Burton more flexibility for traveling, working, and more.
Still, the devices aren’t ready for testing in humans—yet. But recent advancements in engineering mean that the first preclinical trials for an artificial kidney could happen as soon as 18 months from now, according to Jonathan Himmelfarb, a nephrologist at the University of Washington.
“It would liberate people with kidney failure,” Himmelfarb says.
An engineering marvel
Compared to the heart or the brain, the kidney doesn’t get as much respect from the medical profession, but its job is far more complex. “It does hundreds of different things,” says UCLA’s Ira Kurtz.
Kurtz would know. He’s worked as a nephrologist for 37 years, devoting his career to helping those with kidney disease. While his colleagues in cardiology and endocrinology have seen major advances in the development of artificial hearts and insulin pumps, little has changed for patients on hemodialysis. The machines remain bulky and require large volumes of a liquid called dialysate to remove toxins from a patient’s blood, along with gallons of purified water. A kidney transplant is the next best thing to someone’s own, functioning organ, but with over 600,000 Americans on dialysis and only about 100,000 kidney transplants each year, most of those in kidney failure are stuck on dialysis.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. Each of the 45 different cell types in the kidney do something different.
Part of the lack of progress in artificial kidney design is the sheer complexity of the kidney’s job. To build an artificial heart, Kurtz says, you basically need to engineer a pump. An artificial pancreas needs to balance blood sugar levels with insulin secretion. While neither of these tasks is simple, they are fairly straightforward. The kidney, on the other hand, does more than get rid of waste products like urea and other toxins. Each of the 45 different cell types in the kidney do something different, helping to regulate electrolytes like sodium, potassium, and phosphorous; maintaining blood pressure and water balance; guiding the body’s hormonal and inflammatory responses; and aiding in the formation of red blood cells.

There's been little progress for patients during Ira Kurtz's 37 years as a nephrologist. Artificial kidneys would change that.
UCLA
Dialysis primarily filters waste, and does so well enough to keep someone alive, but it isn’t a true artificial kidney because it doesn’t perform the kidney’s other jobs, according to Kurtz, such as sensing levels of toxins, wastes, and electrolytes in the blood. Due to the size and water requirements of existing dialysis machines, the equipment isn’t portable. Physicians write a prescription for a certain duration of dialysis and assess how well it’s working with semi-regular blood tests. The process of dialysis itself, however, is conducted blind. Doctors can’t tell how much dialysis a patient needs based on kidney values at the time of treatment, says Meera Harhay, a nephrologist at Drexel University in Philadelphia.
But it’s the impact of dialysis on their day-to-day lives that creates the most problems for patients. Only one-quarter of those on dialysis are able to remain employed (compared to 85% of similar-aged adults), and many report a low quality of life. Having more flexibility in life would make a major different to her patients, Harhay says.
“Almost half their week is taken up by the burden of their treatment. It really eats away at their freedom and their ability to do things that add value to their life,” she says.
Art imitates life
The challenge for artificial kidney designers was how to compress the kidney’s natural functions into a portable, wearable, or implantable device that wouldn’t need constant access to gallons of purified and sterilized water. The other universal challenge they faced was ensuring that any part of the artificial kidney that would come in contact with blood was kept germ-free to prevent infection.
As part of last year’s KidneyX Prize, a partnership between the U.S. Department of Health and Human Services and the American Society of Nephrology, inventors were challenged to create prototypes for artificial kidneys. Himmelfarb’s team at the University of Washington’s Center for Dialysis Innovation won the prize by focusing on miniaturizing existing technologies to create a portable dialysis machine. The backpack sized AKTIV device (Ambulatory Kidney to Increase Vitality) will recycle dialysate in a closed loop system that removes urea from blood and uses light-based chemical reactions to convert the urea to nitrogen and carbon dioxide, which allows the dialysate to be recirculated.
Himmelfarb says that the AKTIV can be used when at home, work, or traveling, which will give users more flexibility and freedom. “If you had a 30-pound device that you could put in the overhead bins when traveling, you could go visit your grandkids,” he says.
Kurtz’s team at UCLA partnered with the U.S. Kidney Research Corporation and Arkansas University to develop a dialysate-free desktop device (about the size of a small printer) as the first phase of a progression that will he hopes will lead to something small and implantable. Part of the reason for the artificial kidney’s size, Kurtz says, is the number of functions his team are cramming into it. Not only will it filter urea from blood, but it will also use electricity to help regulate electrolyte levels in a process called electrodeionization. Kurtz emphasizes that these additional functions are what makes his design a true artificial kidney instead of just a small dialysis machine.
One version of an artificial kidney.
UCLA
“It doesn't have just a static function. It has a bank of sensors that measure chemicals in the blood and feeds that information back to the device,” Kurtz says.
Other startups are getting in on the game. Nephria Bio, a spinout from the South Korean-based EOFlow, is working to develop a wearable dialysis device, akin to an insulin pump, that uses miniature cartridges with nanomaterial filters to clean blood (Harhay is a scientific advisor to Nephria). Ian Welsford, Nephria’s co-founder and CTO, says that the device’s design means that it can also be used to treat acute kidney injuries in resource-limited settings. These potentials have garnered interest and investment in artificial kidneys from the U.S. Department of Defense.
For his part, Burton is most interested in an implantable device, as that would give him the most freedom. Even having a regular outpatient procedure to change batteries or filters would be a minor inconvenience to him.
“Being plugged into a machine, that’s not mimicking life,” he says.