How mRNA Could Revolutionize Medicine

In November 2020, messenger RNA catapulted into the public consciousness when the first COVID-19 vaccines were authorized for emergency use. Around the same time, an equally groundbreaking yet relatively unheralded application of mRNA technology was taking place at a London hospital.
Over the past two decades, there's been increasing interest in harnessing mRNA — molecules present in all of our cells that act like digital tape recorders, copying instructions from DNA in the cell nucleus and carrying them to the protein-making structures — to create a whole new class of therapeutics.
Scientists realized that artificial mRNA, designed in the lab, could be used to instruct our cells to produce certain antibodies, turning our bodies into vaccine-making factories, or to recognize and attack tumors. More recently, researchers recognized that mRNA could also be used to make another groundbreaking technology far more accessible to more patients: gene editing. The gene-editing tool CRISPR has generated plenty of hype for its potential to cure inherited diseases. But delivering CRISPR to the body is complicated and costly.
"Most gene editing involves taking cells out of the patient, treating them and then giving them back, which is an extremely expensive process," explains Drew Weissman, professor of medicine at the University of Pennsylvania, who was involved in developing the mRNA technology behind the COVID-19 vaccines.
But last November, a Massachusetts-based biotech company called Intellia Therapeutics showed it was possible to use mRNA to make the CRISPR system inside the body, eliminating the need to extract cells out of the body and edit them in a lab. Just as mRNA can instruct our cells to produce antibodies against a viral infection, it can also teach them to produce one of the two components that make up CRISPR — a cutting protein that snips out a problem gene.
"The pandemic has really shown that not only are mRNA approaches viable, they could in certain circumstances be vastly superior to more traditional technologies."
In Intellia's London-based clinical trial, the company applied this for the first time in a patient with a rare inherited liver disease known as hereditary transthyretin amyloidosis with polyneuropathy. The disease causes a toxic protein to build up in a person's organs and is typically fatal. In a company press release, Intellia's president and CEO John Leonard swiftly declared that its mRNA-based CRISPR therapy could usher in a "new era of potential genome editing cures."
Weissman predicts that turning CRISPR into an affordable therapy will become the next major frontier for mRNA over the coming decade. His lab is currently working on an mRNA-based CRISPR treatment for sickle cell disease. More than 300,000 babies are born with sickle cell every year, mainly in lower income nations.
"There is a FDA-approved cure, but it involves taking the bone marrow out of the person, and then giving it back which is prohibitively expensive," he says. It also requires a patient to have a matched bone marrow done. "We give an intravenous injection of mRNA lipid nanoparticles that target CRISPR to the bone marrow stem cells in the patient, which is easy, and much less expensive."
Cancer Immunotherapy
Meanwhile, the overwhelming success of the COVID-19 vaccines has focused attention on other ways of using mRNA to bolster the immune system against threats ranging from other infectious diseases to cancer.
The practicality of mRNA vaccines – relatively small quantities are required to induce an antibody response – coupled with their adaptable design, mean companies like Moderna are now targeting pathogens like Zika, chikungunya and cytomegalovirus, or CMV, which previously considered commercially unviable for vaccine developers. This is because outbreaks have been relatively sporadic, and these viruses mainly affect people in low-income nations who can't afford to pay premium prices for a vaccine. But mRNA technology means that jabs could be produced on a flexible basis, when required, at relatively low cost.
Other scientists suggest that mRNA could even provide a means of developing a universal influenza vaccine, a goal that's long been the Holy Grail for vaccinologists around the world.
"The mRNA technology allows you to pick out bits of the virus that you want to induce immunity to," says Michael Mulqueen, vice president of business development at eTheRNA, a Belgium-based biotech that's developing mRNA-based vaccines for malaria and HIV, as well as various forms of cancer. "This means you can get the immune system primed to the bits of the virus that don't vary so much between strains. So you could actually have a single vaccine that protects against a whole raft of different variants of the same virus, offering more universal coverage."
Before mRNA became synonymous with vaccines, its biggest potential was for cancer treatments. BioNTech, the German biotech company that collaborated with Pfizer to develop the first authorized COVID-19 vaccine, was initially founded to utilize mRNA for personalized cancer treatments, and the company remains interested in cancers ranging from melanoma to breast cancer.
One of the major hurdles in treating cancer has been the fact that tumors can look very different from one person to the next. It's why conventional approaches, such as chemotherapy or radiation, don't work for every patient. But weaponizing mRNA against cancer primes the immune cells with the tumor's specific genetic sequence, training the patient's body to attack their own unique type of cancer.
"It means you're able to think about personalizing cancer treatments down to specific subgroups of patients," says Mulqueen. "For example, eTheRNA are developing a renal cell carcinoma treatment which will be targeted at around 20% of these patients, who have specific tumor types. We're hoping to take that to human trials next year, but the challenge is trying to identify the right patients for the treatment at an early stage."
Repairing Damaged mRNA
While hopes are high that mRNA could usher in new cancer treatments and make CRISPR more accessible, a growing number of companies are also exploring an alternative to gene editing, known as RNA editing.
In genetic disorders, the mRNA in certain cells is impaired due to a rogue gene defect, and so the body ceases to produce a particular vital protein. Instead of permanently deleting the problem gene with CRISPR, the idea behind RNA editing is to inject small pieces of synthetic mRNA to repair the existing mRNA. Scientists think this approach will allow normal protein production to resume.
Over the past few years, this approach has gathered momentum, as some researchers have recognized that it holds certain key advantages over CRISPR. Companies from Belgium to Japan are now looking at RNA editing to treat all kinds of disorders, from Huntingdon's disease, to amyotrophic lateral sclerosis, or ALS, and certain types of cancer.
"With RNA editing, you don't need to make any changes to the DNA," explains Daniel de Boer, CEO of Dutch biotech ProQR, which is looking to treat rare genetic disorders that cause blindness. "Changes to the DNA are permanent, so if something goes wrong, that may not be desirable. With RNA editing, it's a temporary change, so we dose patients with our drugs once or twice a year."
Last month, ProQR reported a landmark case study, in which a patient with a rare form of blindness called Leber congenital amaurosis, which affects the retina at the back of the eye, recovered vision after three months of treatment.
"We have seen that this RNA therapy restores vision in people that were completely blind for a year or so," says de Boer. "They were able to see again, to read again. We think there are a large number of other genetic diseases we could go after with this technology. There are thousands of different mutations that can lead to blindness, and we think this technology can target approximately 25% of them."
Ultimately, there's likely to be a role for both RNA editing and CRISPR, depending on the disease. "I think CRISPR is ideally suited for illnesses where you would like to permanently correct a genetic defect," says Joshua Rosenthal of the Marine Biology Laboratory in Chicago. "Whereas RNA editing could be used to treat things like pain, where you might want to reset a neural circuit temporarily over a shorter period of time."
Much of this research has been accelerated by the COVID-19 pandemic, which has played a major role in bringing mRNA to the forefront of people's minds as a therapeutic.
"The pandemic has really shown that not only are mRNA approaches viable, they could in certain circumstances be vastly superior to more traditional technologies," says Mulqueen. "In the future, I would not be surprised if many of the top pharma products are mRNA derived."
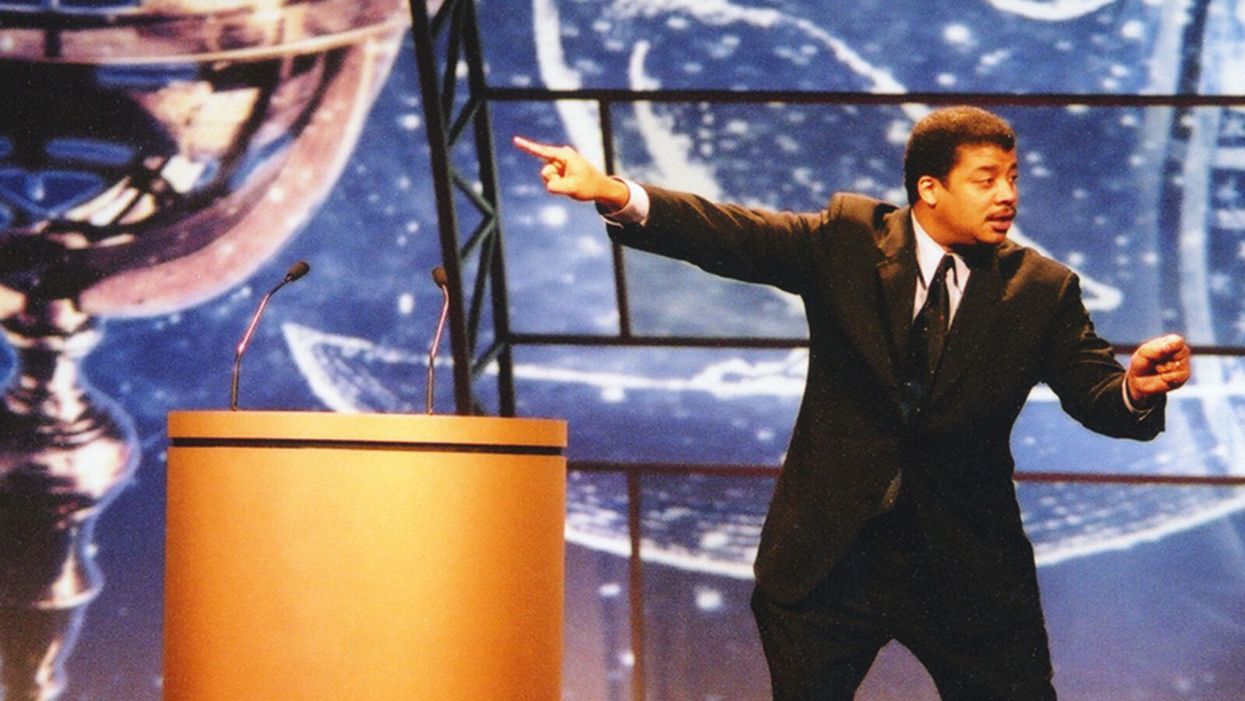
Neil deGrasse Tyson Wants Celebrities to Promote Scientists
Neil de Grasse Tyson wants fellow celebrities to point their followers to experts and organizations who know what they're talking about.
"President Kennedy was the first president to not wear a hat. Have you seen men wearing hats since then?" Neil deGrasse Tyson, one of the world's few astrophysicists with a household name, asks on the phone from his car. Well, no. "If I wear some cowboy hats, it's because it's the outfit, it's not because that's my standard equipment when I leave the home."
"We have classes on 100 things and none of them are on the ability to distinguish what is true and what is not."
But Tyson, who speaks in methodically reasoned paragraphs with lots of semi-rhetorical questions to make sure we're all still listening, isn't really making a point about Mad Men-era men's clothing trends. "Should a president influence fashion?" he says. "I think people sometimes don't know the full power they have over other people. So, that's the first prong in this comment. My second prong is, why would anyone take medical advice from a politician?"
Days before our conversation, news broke that President Trump said he was taking hydroxychloroquine, which he had hyped for months as a surefire magical cure for COVID-19 — the science just hadn't caught up to his predictions. But the science never did catch up; instead, it went the opposite direction, showing that hydroxychloroquine, when used to treat COVID-19 patients, actually led to an increased risk of death.
Alarm spread swiftly around the globe as experts cast the president's professed self-medicating as illogical and dangerous. However, it was just one of a series of wild pieces of medical advice espoused by Trump from his mighty pulpit, like that, hey, maybe disinfectants could cure people when injected into their bodies. (That also leads to death.)
But people do take medical advice from politicians. An Arizona man afraid of COVID-19 died after consuming chloroquine phosphate, which he and his wife had sitting on the back of a shelf after using it to treat koi fish for parasites. The pandemic has exposed many weaknesses in the feedback loop of society, government, the media, and science, including the difficulty of seeding accurate medical information with the masses. Many on the left and right decry a broken political and news media system, but Tyson believes the problem isn't mega-influencers like Trump. Rather it's the general public's desire to take their advice on complex topics – like the science of virology – that such influencers know nothing about.
Tyson's not upset with the public, who follow Trump's advice. "As an educator, I can't get angry with you," he says. Or even Trump himself. "Trump was elected by 60 million people, right? So, you could say all you want about Trump, kick him out of office, whatever. [There's] still the 60 million fellow Americans who walk among us who voted for him. So, what are you going to do with them?"
Tyson also isn't upset with Facebook, Twitter, and other social platforms that serve as today's biggest conduits for misinformation. After all, in the realm of modern media's history, these networks are tadpoles. "As an educator and as a scientist, I'm leaning towards, let's figure out a way to train people in school to not fall victim to false information, and how to judge what is likely to be false relative to what is likely to be true. And that's hard, but you and I have never had a class in that, have we? We've had biology classes, we've had English lit, we've had classes on Shakespeare — we have classes on 100 things and none of them are on the ability to distinguish what is true and what is not."
This is why Tyson himself doesn't engage in Trump bashing on his social feeds, but does try to get people to differentiate factual science from fake news. "I feel responsibility to participate in the enlightenment of culture and of civilization, because I have that access," says Tyson, who has 13.9M followers on Twitter, 1.2M on Instagram, and 4.2M on Facebook. He doesn't tell his followers not to inject themselves with Clorox ("no one likes being told what to do"), but tries to get them to visualize a pandemic's impact by comparing it to, say, a throng of rabbits.
"Left unchecked, 1,000 rabbits in 5 years, become 7-billion, the human population of the World. After 15 years, a 'land-ocean' of rabbits fills to one-kilometer depth across all of Earth's continents. Viruses can reproduce waaaay faster than Rabbits," he tweeted on April 6, after much of the nation had locked down to slow the pandemic's spread. For added viral impact, he attached a photo of an adorable, perhaps appropriately scared-looking, white bunny.
Of course, not all celebrities message responsibly.
Tyson is a rare scientist-turned-celebrity. His appeal isn't acting in movies or singing dance-pop anthems (if only). Rather, his life's work is making science fun and interesting to as many people as possible through his best-selling books on astrophysics and his directorship of the planetarium at the American Museum of Natural History in New York. His longstanding place in popular culture is an exception, not the rule.
And he believes his fellow celebrities, actors and pop music stars and internet influencers, should aid the public's quest for accurate scientific information. And in order to do that, they must point their followers to experts and organizations who know what they're talking about. "It could be to a website, it could be to a talk that was given. I would say that that's where the responsibility lies if you control the interests of a million people," he says.
One example of this is Lady Gaga's March 14 Instagram of herself on her couch with her three dogs with the caption, "So I talked to some doctors and scientists. It's not the easiest for everyone right now but the kindest/healthiest thing we can do is self-quarantine and not hang out with people over 65 and in large groups. I wish I could see my parents and grandmas right now but it's much safer to not so I don't get them sick in case I have it. I'm hanging at home with my dogs." (All the celebrities here in this article are my references, not Tyson's, who does not call out specific people.)
Of course, not all celebrities message responsibly. Jessica Biel and Jenny McCarthy have faced scorn for public stances against vaccines. Gwyneth Paltrow and her media brand GOOP have faced backlash for promoting homeopathic treatments with no basis in science.
"The New Age Movement is a cultural idea, it has nothing to do with religion, has nothing to do with politics, and it's people who were rejecting objectively established science in part or in total because they have a belief system that they want to attach to it, okay? This is how you get the homeopathic remedies," says Tyson. "That's why science exists, so that we don't have to base decisions on belief systems."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
Masks and Distancing Won't Be Enough to Prevent School Outbreaks, Latest Science Suggests
The likely dominant mode of aerosol transmission cannot be ignored in school settings.
Never has the prospect of "back to school" seemed so ominous as it does in 2020. As the number of COVID-19 cases climb steadily in nearly every state, the prospect of in-person classes are filling students, parents, and faculty alike with a corresponding sense of dread.
The notion that children are immune or resistant to SARS-CoV-2 is demonstrably untrue.
The decision to resume classes at primary, secondary, and collegiate levels is not one that should be regarded lightly, particularly as coronavirus cases skyrocket across the United States.
What should be a measured, data-driven discussion that weighs risks and benefits has been derailed by political talking points. President Trump has been steadily advocating for an unfettered return to the classroom, often through imperative "OPEN THE SCHOOLS!!!" tweets. In July, Secretary of Education Betsy DeVos threatened to withhold funding from schools that did not reopen for full-time, in-person classes, despite not having the authority to do so. Like so many public health issues, opening schools in the midst of a generational pandemic has been politicized to the point that the question of whether it is safe to do so has been obscured and confounded. However, this question still deserves to be examined based on evidence.
What We Know About Kids and COVID-19
Some arguments for returning to in-person education have focused on the fact that children and young adults are less susceptible to severe disease. In some cases, people have stated that children cannot be infected, pointing to countries that have resumed in-person education with no associated outbreaks. However, those countries had extremely low community transmission and robust testing and surveillance.
The notion that children are immune or resistant to SARS-CoV-2 is demonstrably untrue: children can be infected, they can become sick, and, in rare cases, they can die. Children can also transmit the virus to others, especially if they are in prolonged proximity to them. A Georgia sleepaway camp was the site of at least 260 cases among mostly children and teenagers, some as young as 6 years old. Children have been shown to shed infectious virus in their nasal secretions and have viral loads comparable to adults. Children can unquestionably be infected with SARS-CoV-2 and spread it to others.
The more data emerges, the more it appears that both primary and secondary schools and universities alike are conducive environments for super-spreading. Mitigating these risks depends heavily on individual schools' ability to enforce reduction measures. So far, the evidence demonstrates that in most cases, schools are unable to adequately protect students or staff. A school superintendent from a small district in Arizona recently described an outbreak that occurred among staff prior to in-person classes resuming. Schools that have opened so far have almost immediately reported new clusters of cases among students or staff.
This is because it is impossible to completely eliminate risk even with the most thoughtful mitigation measures when community transmission is high. Risk can be reduced, but the greater the likelihood that someone will be exposed in the community, the greater the risk they might pass the virus to others on campus or in the classroom.
There are still many unknowns about SARS-CoV-2 transmission, but some environments are known risks for virus transmission: enclosed spaces with crowds of people in close proximity over extended durations. Transmission is thought to occur predominantly through inhaled aerosols or droplets containing SARS-CoV-2, which are produced through common school activities such as breathing, speaking, or singing. Masks reduce but do not eliminate the production of these aerosols. Implementing universal mask-wearing and physical distancing guidelines will furthermore be extraordinarily challenging for very young children.
Smaller particle aerosols can remain suspended in the air and accumulate over time. In an enclosed space where people are gathering, such as a classroom, this renders risk mitigation measures such as physical distancing and masks ineffective. Many classrooms at all levels of education are not conducive to improving ventilation through low-cost measures such as opening windows, much less installing costly air filtration systems.
As a risk reduction measure, ventilation greatly depends on factors like window placement, window type, room size, room occupancy, building HVAC systems, and overall airflow. There isn't much hard data on the specific effects of ventilation on virus transmission, and the models that support ventilation rely on assumptions based on scant experimental evidence that doesn't account for virologic parameters.
There is also no data about how effective air filtration or UV systems would be for SARS-CoV-2 transmission risk reduction, so it's hard to say if this would result in a meaningful risk reduction or not. We don't have enough data outside of a hospital setting to support that ventilation and/or filtration would significantly reduce risk, and it's impractical (and most likely impossible in most schools) to implement hospital ventilation systems, which would likely require massive remodeling of existing HVAC infrastructure. In a close contact situation, the risk reduction might be minimal anyway since it's difficult to avoid exposure to respiratory aerosols and droplets a person is exhaling.
You'd need to get very low rates in the local community to open safely in person regardless of other risk reduction measures, and this would need to be complemented by robust testing and contact tracing capacity.
Efforts to resume in-person education depend heavily on school health and safety plans, which often rely on self-reporting of symptoms due to insufficient testing capacity. Self-reporting is notoriously unreliable, and furthermore, SARS-CoV-2 can be readily transmitted by pre-symptomatic individuals who may be unaware that they are sick, making testing an essential component of any such plan. Primary and secondary schools are faced with limited access to testing and no funds to support it. Even in institutions that include a testing component in their reopening plans, this is still too infrequent to support the full student body returning to campus.
Economic Conflicts of Interest
Rebecca Harrison, a PhD candidate at Cornell University serving on the campus reopening committee, is concerned that her institution's plan places too much faith in testing capacity and is over-reliant on untested models. Harrison says that, as a result, students are being implicitly encouraged to return to campus and "very little has been done to actively encourage students who are safe and able to stay home, to actually stay home."
Harrison also is concerned that her institution "presumably hopes to draw students back from the safety of their parents' basements to (re)join the residential campus experience ... and drive revenue." This is a legitimate concern. Some schools may be actively thwarting safety plans in place to protect students based on financial incentives. Student athletes at Colorado State have alleged that football coaches told them not to report COVID-19 symptoms and are manipulating contact tracing reports.
Public primary and secondary schools are not dependent on student athletics for revenue, but nonetheless are susceptible to state and federal policies that tie reopening to budgets. If schools are forced to make decisions based on a balance sheet, rather than the health and safety of students, teachers, and staff, they will implement health and safety plans that are inadequate. Schools will become ground zero for new clusters of cases.
Looking Ahead: When Will Schools Be Able to Open Again?
One crucial measure is the percent positivity rate in the local community, the number of positive tests based on all the tests that are done. Some states, like California, have implemented policies guiding the reopening of schools that depend in part on a local community's percent positivity rate falling under 8 percent, among other benchmarks including the rate of new daily cases. Currently, statewide, test positivity is below 7%, with an average of 3 new daily cases per 1000 people per day. However, the California department of health acknowledges that new cases per day are underreported. There are 6.3 million students in the California public school system, suggesting that at any given time, there could be nearly 20,000 students who might be contagious, without accounting for presymptomatic teachers and staff. In the classroom environment, just one of those positive cases could spread the virus to many people in one day despite masks, distancing, and ventilation.
You'd need to get very low rates in the local community to open safely in person regardless of other risk reduction measures, and this would need to be complemented by robust testing and contact tracing capacity. Only with rapid identification and isolation of new cases, followed by contact tracing and quarantine, can we break chains of transmission and prevent further spread in the school and the larger community.
None of these safety concerns diminish the many harms associated with the sudden and haphazard way remote learning has been implemented. Online education has not been effective in many cases and is difficult to implement equitably. Young children, in particular, are deprived of the essential social and intellectual development they would normally get in a classroom with teachers and their peers. Parents of young children are equally unprepared and unable to provide full-time instruction. Our federal leadership's catastrophic failure to contain the pandemic like other countries has put us in this terrible position, where we must choose between learning or spreading a deadly pathogen.
Blame aside, parents, educators, and administrators must decide whether to resume in-person classes this fall. Those decisions should be based on evidence, not on politics or economics. The data clearly shows that community transmission is out of control throughout most of the country. Thus, we ignore the risk of school outbreaks at our peril.
[Editor's Note: Here's the other essay in the Back to School series: 5 Key Questions to Consider Before Sending Your Child Back to School.]