Podcast: Tech for Mental Wellbeing with Nanea Reeves, CEO of TRIPP

An image from one of TRIPP's virtual reality experiences for mental wellness. Nanea Reeves is TRIPP's CEO.
The "Making Sense of Science" podcast features interviews with leading experts about health innovations and the ethical questions they raise. The podcast is hosted by Matt Fuchs, editor of Leaps.org, the award-winning science outlet.
My guest today is Nanea Reeves, the CEO of TRIPP, a wellness platform with some big differences from meditation apps you may have tried like Calm and Headspace. TRIPP's experiences happen in virtual reality, and its realms are designed based on scientific findings about states of mindfulness. Users report feelings of awe and wonder and even mystical experiences. Nanea brings over 15 years of leadership in digital distribution, apps and video game technologies. Before co-founding TRIPP, she had several other leadership roles in tech with successful companies like textPlus and Machinima. Read her full bio below in the links section.

Nanea Reeves, CEO of TRIPP.
TRIPP
Listen to the Episode
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
This conversation coincided with National Brain Awareness Week. The topic is a little different from the Making Sense of Science podcast’s usual focus on breakthroughs in treating and preventing disease, but there’s a big overlap when it comes to breakthroughs in optimal health. Nanea’s work is at the leading edge of health, technology and the science of wellness.
With TRIPP, you might find yourself deep underwater, looking up at the sunlight shimmering on the ocean surface, or in the cosmos staring down at a planet glowing with an arresting diversity of colors. Using TRIPP for the past six months has been a window for me into the future of science-informed wellness and an overall fascinating experience, as was my conversation with Nanea.
Show notes:
Nanea and I discuss her close family members' substance addictions and her own struggle with mental illness as a teen, which led to her first meditation experiences, and much more:
- The common perception that technology is an obstacle for mental well-being, a narrative that overlooks how tech can also increase wellness when it’s designed right.
- Emerging ways of measuring meditation experiences by recording brain waves - and the shortcomings of the ‘measured self’ movement.
- Why TRIPP’s users multiplied during the stress and anxiety of the pandemic, and how TRIPP can can be used to enhance emotional states.
- Ways in which TRIPP’s visuals and targeted sound frequencies have been informed by innovative research from psychologists like Johns Hopkins’ Matthew Johnson.
- Ways to design apps and other technologies to better fulfill the true purpose of mindfulness meditation. (Hint: not simply relaxation.)
- And of course, because the topic is mental wellness and tech, I had to get Nanea's thoughts on Elon Musk, Neuralink and brain machine interfaces.
Here are links for learning more about TRIPP:
- TRIPP website: https://www.tripp.com/about/
- Nanea Reeves bio: https://www.tripp.com/team/nanea-reeves/
- Study of data collected by UK's Office for National Statistics on behavior during the pandemic, which suggests that TRIPP enhanced users' psychological and emotional mindsets: https://link.springer.com/chapter/10.1007/978-3-03...
- Research that's informed TRIPP: https://www.tripp.com/research/
- Washington Post Top Pick at CES: https://www.washingtonpost.com/technology/2019/01/...
- TRIPP's new offering, PsyAssist, to provide support for ketamine-assisted therapy: https://www.mobihealthnews.com/news/tripp-acquires...
- Randomized pilot trial involving TRIPP: https://bmjopen.bmj.com/content/bmjopen/11/4/e0441...
In this week's Friday Five, an old diabetes drug finds an exciting new purpose. Plus, how to make the cities of the future less toxic, making old mice younger with EVs, a new reason for mysterious stillbirths - and much more.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here is the promising research covered in this week's Friday Five:
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
- How to make cities of the future less noisy
- An old diabetes drug could have a new purpose: treating an irregular heartbeat
- A new reason for mysterious stillbirths
- Making old mice younger with EVs
- No pain - or mucus - no gain
And an honorable mention this week: How treatments for depression can change the structure of the brain
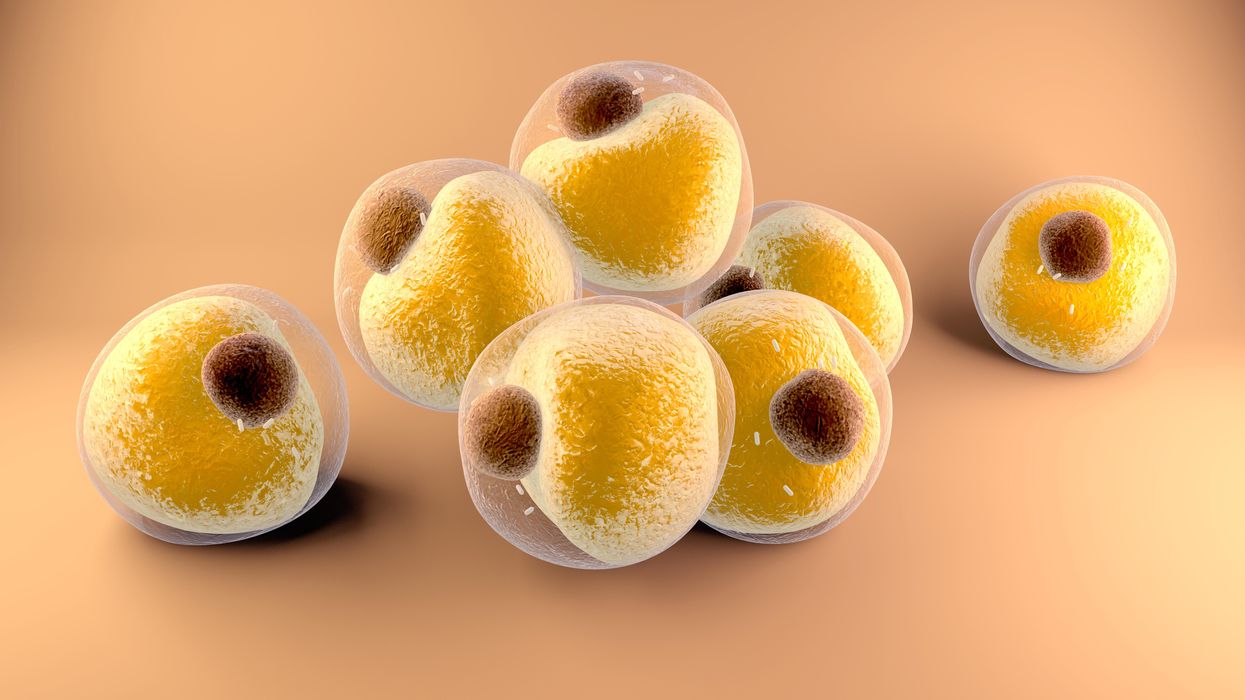
Researchers at Stanford have found that the virus that causes Covid-19 can infect fat cells, which could help explain why obesity is linked to worse outcomes for those who catch Covid-19.
Obesity is a risk factor for worse outcomes for a variety of medical conditions ranging from cancer to Covid-19. Most experts attribute it simply to underlying low-grade inflammation and added weight that make breathing more difficult.
Now researchers have found a more direct reason: SARS-CoV-2, the virus that causes Covid-19, can infect adipocytes, more commonly known as fat cells, and macrophages, immune cells that are part of the broader matrix of cells that support fat tissue. Stanford University researchers Catherine Blish and Tracey McLaughlin are senior authors of the study.
Most of us think of fat as the spare tire that can accumulate around the middle as we age, but fat also is present closer to most internal organs. McLaughlin's research has focused on epicardial fat, “which sits right on top of the heart with no physical barrier at all,” she says. So if that fat got infected and inflamed, it might directly affect the heart.” That could help explain cardiovascular problems associated with Covid-19 infections.
Looking at tissue taken from autopsy, there was evidence of SARS-CoV-2 virus inside the fat cells as well as surrounding inflammation. In fat cells and immune cells harvested from health humans, infection in the laboratory drove "an inflammatory response, particularly in the macrophages…They secreted proteins that are typically seen in a cytokine storm” where the immune response runs amok with potential life-threatening consequences. This suggests to McLaughlin “that there could be a regional and even a systemic inflammatory response following infection in fat.”
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
The macrophages studied by McLaughlin and Blish were spewing out inflammatory proteins, While the the virus within them was replicating, the new viral particles were not able to replicate within those cells. It was a different story in the fat cells. “When [the virus] gets into the fat cells, it not only replicates, it's a productive infection, which means the resulting viral particles can infect another cell,” including microphages, McLaughlin explains. It seems to be a symbiotic tango of the virus between the two cell types that keeps the cycle going.
It is easy to see how the airborne SARS-CoV-2 virus infects the nose and lungs, but how does it get into fat tissue? That is a mystery and the source of ample speculation.
Macrophages are mobile; they engulf and carry invading pathogens to lymphoid tissue in the lymph nodes, tonsils and elsewhere in the body to alert T cells of the immune system to the pathogen. Perhaps some of them also carry the virus through the bloodstream to more distant tissue.
ACE2 receptors are the means by which SARS-CoV-2 latches on to and enters most cells. They are not thought to be common on fat cells, so initially most researchers thought it unlikely they would become infected.
However, while some cell receptors always sit on the surface of the cell, other receptors are expressed on the surface only under certain conditions. Philipp Scherer, a professor of internal medicine and director of the Touchstone Diabetes Center at the University of Texas Southwestern Medical Center, suggests that, in people who have obesity, “There might be higher levels of dysfunctional [fat cells] that facilitate entry of the virus,” either through transiently expressed ACE2 or other receptors. Inflammatory proteins generated by macrophages might contribute to this process.
Another hypothesis is that viral RNA might be smuggled into fat cells as cargo in small bits of material called extracellular vesicles, or EVs, that can travel between cells. Other researchers have shown that when EVs express ACE2 receptors, they can act as decoys for SARS-CoV-2, where the virus binds to them rather than a cell. These scientists are working to create drugs that mimic this decoy effect as an approach to therapy.
Do fat cells play a role in Long Covid? “Fat cells are a great place to hide. You have all the energy you need and fat cells turn over very slowly; they have a half-life of ten years,” says Scherer. Observational studies suggest that acute Covid-19 can trigger the onset of diabetes especially in people who are overweight, and that patients taking medicines to regulate their diabetes “were actually quite protective” against acute Covid-19. Scherer has funding to study the risks and benefits of those drugs in animal models of Long Covid.
McLaughlin says there are two areas of potential concern with fat tissue and Long Covid. One is that this tissue might serve as a “big reservoir where the virus continues to replicate and is sent out” to other parts of the body. The second is that inflammation due to infected fat cells and macrophages can result in fibrosis or scar tissue forming around organs, inhibiting their function. Once scar tissue forms, the tissue damage becomes more difficult to repair.
Current Covid-19 treatments work by stopping the virus from entering cells through the ACE2 receptor, so they likely would have no effect on virus that uses a different mechanism. That means another approach will have to be developed to complement the treatments we already have. So the best advice McLaughlin can offer today is to keep current on vaccinations and boosters and lose weight to reduce the risk associated with obesity.