A vaccine for Lyme disease could be coming. But will patients accept it?

Hiking is one of Marci Flory's favorite activities, but her chronic Lyme disease sometimes renders her unable to walk. Biotech companies Pfizer and Valneva are testing a vaccine for Lyme disease in a Phase III clinical trial.
For more than two decades, Marci Flory, a 40-year-old emergency room nurse from Lawrence, Kan., has battled the recurring symptoms of chronic Lyme disease, an illness which she believes began after being bitten by a tick during her teenage years.
Over the years, Flory has been plagued by an array of mysterious ailments, ranging from fatigue to crippling pain in her eyes, joints and neck, and even postural tachycardia syndrome or PoTS, an abnormal increase in heart rate after sitting up or standing. Ten years ago, she began to experience the onset of neurological symptoms which ranged from brain fog to sudden headaches, and strange episodes of leg weakness which would leave her unable to walk.
“Initially doctors thought I had ALS, or less likely, multiple sclerosis,” she says. “But after repeated MRI scans for a year, they concluded I had a rare neurological condition called acute transverse myelitis.”
But Flory was not convinced. After ordering a variety of private blood tests, she discovered she was infected with a range of bacteria in the genus Borrelia that live in the guts of ticks, the infectious agents responsible for Lyme disease.
“It made sense,” she says. “Looking back, I was bitten in high school and misdiagnosed with mononucleosis. This was probably the start, and my immune system kept it under wraps for a while. The Lyme bacteria can burrow into every tissue in the body, go into cyst form and become dormant before reactivating.”
The reason why cases of Lyme disease are increasing is down to changing weather patterns, triggered by climate change, meaning that ticks are now found across a much wider geographic range than ever before.
When these species of bacteria are transmitted to humans, they can attack the nervous system, joints and even internal organs which can lead to serious health complications such as arthritis, meningitis and even heart failure. While Lyme disease can sometimes be successfully treated with antibiotics if spotted early on, not everyone responds to these drugs, and for patients who have developed chronic symptoms, there is no known cure. Flory says she knows of fellow Lyme disease patients who have spent hundreds of thousands of dollars seeking treatments.
Concerningly, statistics show that Lyme and other tick-borne diseases are on the rise. Recently released estimates based on health insurance records suggest that at least 476,000 Americans are diagnosed with Lyme disease every year, and many experts believe the true figure is far higher.
The reason why the numbers are growing is down to changing weather patterns, triggered by climate change, meaning that ticks are now found across a much wider geographic range than ever before. Health insurance data shows that cases of Lyme disease have increased fourfold in rural parts of the U.S. over the last 15 years, and 65 percent in urban regions.
As a result, many scientists who have studied Lyme disease feel that it is paramount to bring some form of protective vaccine to market which can be offered to people living in the most at-risk areas.
“Even the increased awareness for Lyme disease has not stopped the cases,” says Eva Sapi, professor of cellular and molecular biology at the University of New Haven. “Some of these patients are looking for answers for years, running from one doctor to another, so that is obviously a very big cost for our society at so many levels.”
Emerging vaccines – and backlash
But with the rising case numbers, interest has grown among the pharmaceutical industry and research communities. Vienna-based biotech Valneva have partnered with Pfizer to take their vaccine – a seasonal jab which offers protection against the six most common strains of Lyme disease in the northern hemisphere – into a Phase III clinical trial which began in August. Involving 6,000 participants in a number of U.S. states and northern Europe where Lyme disease is endemic, it could lead to a licensed vaccine by 2025, if it proves successful.
“For many years Lyme was considered a small market vaccine,” explains Monica E. Embers, assistant professor of parasitology at Tulane University in New Orleans. “Now we know that this is a much bigger problem, Pfizer has stepped up to invest in preventing this disease and other pharmaceutical companies may as well.”
Despite innovations, patient communities and their representatives remain ambivalent about the idea of a vaccine. Some of this skepticism dates back to the failed LYMErix vaccine which was developed in the late 1990s before being withdrawn from the market.
At the same time, scientists at Yale University are developing a messenger RNA vaccine which aims to train the immune system to respond to tick bites by exposing it to 19 proteins found in tick saliva. Whereas the Valneva vaccine targets the bacteria within ticks, the Yale vaccine attempts to provoke an instant and aggressive immune response at the site of the bite. This causes the tick to fall off and limits the potential for transmitting dangerous infections.
But despite these innovations, patient communities and their representatives remain ambivalent about the idea of a vaccine. Some of this skepticism dates back to the failed LYMErix vaccine which was developed in the late 1990s before being withdrawn from the market in 2002 after concerns were raised that it might induce autoimmune reactions in humans.
While this theory was ultimately disproved, the lingering stigma attached to LYMErix meant that most vaccine manufacturers chose to stay away from the disease for many years, something which Gregory Poland, head of the Mayo Clinic’s Vaccine Research Group in Minnesota, describes as a tragedy.
“Since 2002, we have not had a human Lyme vaccine in the U.S. despite the increasing number of cases,” says Poland. “Pretty much everyone in the field thinks they’re ten times higher than the official numbers, so you’re probably talking at least 400,000 each year. It’s an incredible burden but because of concerns about anti-vax protestors, until very recently, no manufacturer has wanted to touch this.”
Such was the backlash surrounding the failed LYMErix program that scientists have even explored the most creative of workarounds for protecting people in tick-populated regions, without needing to actually vaccinate them. One research program at the University of Tennessee came up with the idea of leaving food pellets containing a vaccine in woodland areas with the idea that rodents would eat the pellets, and the vaccine would then kill Borrelia bacteria within any ticks which subsequently fed on the animals.
Even the Pfizer-Valneva vaccine has been cautiously designed to try and allay any lingering concerns, two decades after LYMErix. “The concept is the same as the original LYMErix vaccine, but it has been made safer by removing regions that had the potential to induce autoimmunity,” says Embers. “There will always be individuals who oppose vaccines, Lyme or otherwise, but it will be a tremendous boost to public health to have the option.”
Vaccine alternatives
Researchers are also considering alternative immunization approaches in case sufficiently large numbers of people choose to reject any Lyme vaccine which gets approved. Researchers at UMass Chan Medical School have developed an artificially generated antibody, administered via an annual injection, which is capable of killing Borrelia bacteria in the guts of ticks before they can get into the human host.
So far animal studies have shown it to be 100 percent effective, while the scientists have completed a Phase I trial in which they tested it for safety on 48 volunteers in Nebraska. Because this approach provides the antibody directly, rather than triggering the human immune system to produce the antibody like a vaccine would, Embers predicts that it could be a viable alternative for the vaccine hesitant as well as providing an option for immunocompromised individuals who cannot produce enough of their own antibodies.
At the same time, many patient groups still raise concerns over the fact that numerous diagnostic tests for Lyme disease have been reported to have a poor accuracy. Without this, they argue that it is difficult to prove whether vaccines or any other form of immunization actually work. “If the disease is not understood enough to create a more accurate test and a universally accepted treatment protocol, particularly for those who weren’t treated promptly, how can we be sure about the efficacy of a vaccine?” says Natasha Metcalf, co-founder of the organization Lyme Disease UK.
Flory points out that there are so many different types of Borrelia bacteria which cause Lyme disease, that the immunizations being developed may only stop a proportion of cases. In addition, she says that chronic Lyme patients often report a whole myriad of co-infections which remain poorly understood and are likely to also be involved in the disease process.

Marci Flory undergoes an infusion in an attempt to treat her Lyme disease symptoms.
Marci Flory
“I would love to see an effective Lyme vaccine but I have my reservations,” she says. “I am infected with four types of Borrelia bacteria, plus many co-infections – Babesia, Bartonella, Erlichiosis, Rickettsia, and Mycoplasma – all from a single Douglas County Kansas tick bite. Lyme never travels alone and the vaccine won’t protect against all the many strains of Borrelia and co-infections.”
Valneva CEO Thomas Lingelbach admits that the Pfizer-Valneva vaccine is not perfect, but predicts that it will still have significant impact if approved.
“We expect the vaccine to have 75 percent plus efficacy,” he says. “There is this legacy around the old Lyme vaccines, but the world is very, very different today. The number of clinical manifestations known to be caused by infection with Lyme Borreliosis has significantly increased, and the understanding around severity has certainly increased.”
Embers agrees that while it will still be important for doctors to monitor for other tick-borne infections which are not necessarily covered by the vaccine, having any clinically approved jab would still represent a major step forward in the fight against the disease.
“I think that any vaccine must be properly vetted, and these companies are performing extensive clinical trials to do just that,” she says. “Lyme is the most common tick-borne disease in the U.S. so the public health impact could be significant. However, clinicians and the general public must remain aware of all of the other tick-borne diseases such as Babesia and Anaplasma, and continue to screen for those when a tick bite is suspected.”
The Nation’s Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored?
Morale at federal science agencies -- and public trust in their guidance -- is at a concerning low right now.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
It didn't have to be this way. More than 200,000 Americans dead, seven million infected, with numbers continuing to climb, an economy in shambles with millions out of work, hundreds of thousands of small businesses crushed with most of the country still under lockdown. And all with no end in sight. This catastrophic result is due in large part to the willful disregard of scientific evidence and of muzzling policy experts by the Trump White House, which has spent its entire time in office attacking science.
One of the few weapons we had to combat the spread of Covid-19—wearing face masks—has been politicized by the President, who transformed this simple public health precaution into a first amendment issue to rally his base. Dedicated public health officials like Dr. Anthony Fauci, the highly respected director of the National Institute of Allergies and Infectious Diseases, have received death threats, which have prompted many of them around the country to resign.
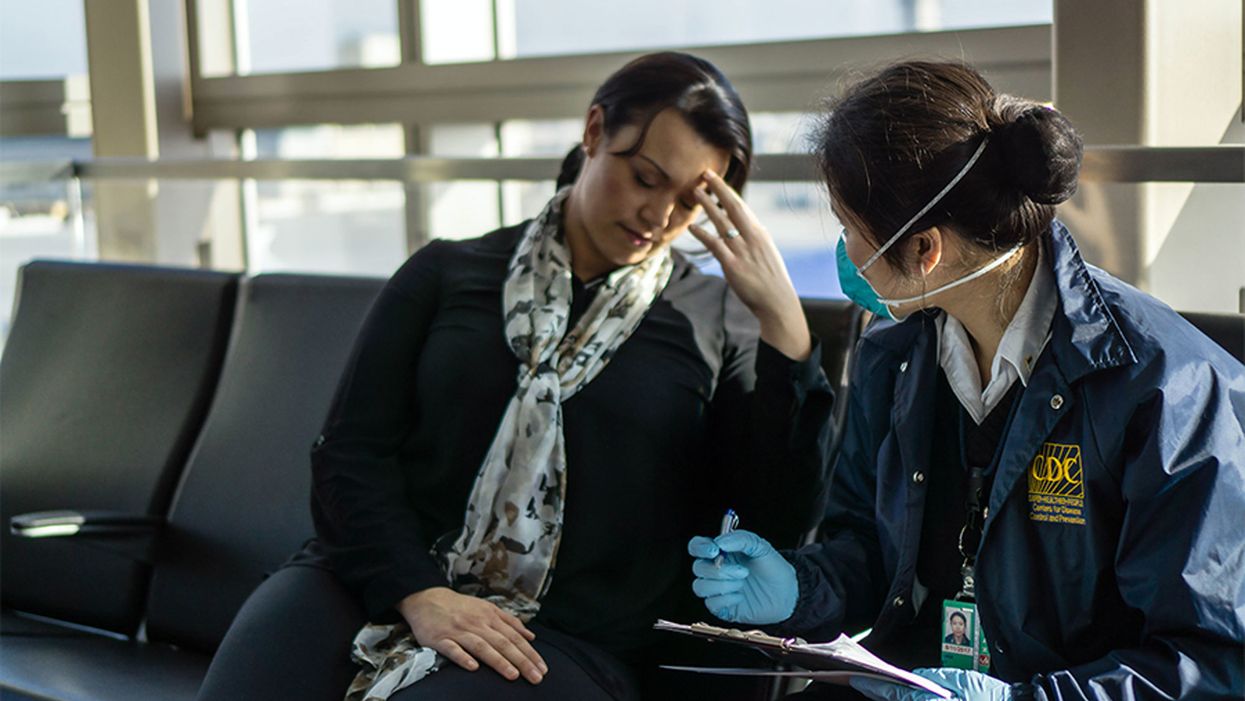
Over the summer, the Trump White House pressured the Centers for Disease Control, which is normally in charge of fighting epidemics, to downplay COVID risks among young people and encourage schools to reopen. And in late September, the CDC was forced to pull federal teams who were going door-to-door doing testing surveys in Minnesota because of multiple incidents of threats and abuse. This list goes on and on.
Still, while the Trump administration's COVID failures are the most visible—and deadly—the nation's entire federal science infrastructure has been undermined in ways large and small.
The White House has steadily slashed monies for science—the 2021 budget cuts funding by 10–30% or more for crucial agencies like National Oceanic and Atmospheric Administration (NOAA) and the Environmental Protection Agency (EPA)—and has gutted health and science agencies across the board, including key agencies of the Department of Energy and the Interior, especially in divisions that deal with issues they oppose ideologically like climate change.
Even farmers can't get reliable information about how climate change affects planting seasons because the White House moved the entire staff at the U.S. Department of Agriculture agency who does this research, relocating them from Maryland to Kansas City, Missouri. Many of these scientists couldn't uproot their families and sell their homes, so the division has had to pretty much start over from scratch with a skeleton crew.
More than 1,600 federal scientists left government in the first two years of the Trump Administration, according to data compiled by the Washington Post, and one-fifth of top positions in science are vacant, depriving agencies of the expertise they need to fulfill their vital functions. Industry executives and lobbyists have been installed as gatekeepers—HHS Secretary Alex Azar was previously president of Eli Lilly, and three climate change deniers were appointed to key posts at the National Oceanic and Atmospheric Administration, to cite just a couple of examples. Trump-appointed officials have sidelined, bullied, or even vilified those who dare to speak out, which chills the rigorous debate that is the essential to sound, independent science.
"The CDC needs to be able to speak regularly to the American people to explain what it knows and how it knows it."
Linda Birnbaum knows firsthand what it's like to become a target. The microbiologist recently retired after more than a decade as the director of the National Institute of Environmental Health Sciences, which is the world's largest environmental health organization and the greatest funder of environmental health and toxicology research, a position that often put her agency at odds with the chemical and fossil fuel industry. There was an attempt to get her fired, she says, "because I had the nerve to write that science should be used in making policy. The chemical industry really went after me, and my last two years were not so much fun under this administration. I'd like to believe it was because I was making a difference—if I wasn't, they wouldn't care."
Little wonder that morale at federal agencies is low. "We're very frustrated," says Dr. William Schaffner, a veteran infectious disease specialist and a professor of medicine at the Vanderbilt University School of Medicine in Nashville. "My colleagues within these agencies, the CDC rank and file, are keeping their heads down doing the best they can, and they hope to weather this storm."
The cruel irony is that the United States was once a beacon of scientific innovation. In the heady post World War II years, while Europe lay in ruins, the successful development of penicillin and the atomic bomb—which Americans believed helped vanquish the Axis powers—unleashed a gusher of public money into research, launching an unprecedented era of achievement in American science. Scientists conquered polio, deciphered the genetic code, harnessed the power of the atom, invented lasers, transistors, microchips and computers, sent missions beyond Mars, and landed men on the moon. A once-inconsequential hygiene laboratory was transformed into the colossus the National Institutes of Health has become, which remains today the world's flagship medical research center, unrivaled in size and scope.
At the same time, a tiny public health agency headquartered in Atlanta, which had been in charge of eradicating the malaria outbreaks that plagued impoverished rural areas in the Deep South until the late 1940s, evolved into the Centers for Disease Control and Prevention. The CDC became the world's leader in fighting disease outbreaks, and the agency's crack team of epidemiologists—members of the vaunted Epidemic Intelligence Service—were routinely dispatched to battle global outbreaks of contagions such as Ebola and malaria and help lead the vaccination campaigns to eradicate killers like polio and small pox that have saved millions of lives.
What will it take to rebuild our federal science infrastructure and restore not only the public's confidence but the respect of the world's scientific community? There are some hopeful signs that there is pushback against the current national leadership, and non-profit watchdog groups like the Union of Concerned Scientists have mapped out comprehensive game plans to restore public trust and the integrity of science.
These include methods of protecting science from political manipulation; restoring the oversight role of independent federal advisory committees, whose numbers were decimated by recent executive orders; strengthening scientific agencies that have been starved by budget cuts and staff attrition; and supporting whistleblower protections and allowing scientists to do their jobs without political meddling to restore integrity to the process. And this isn't just a problem at the CDC. A survey of 1,600 EPA scientists revealed that more than half had been victims of political interference and were pressured to skew their findings, according to research released in April by the Union of Concerned Scientists.
"Federal agencies are staffed by dedicated professionals," says Andrew Rosenberg, director of the Center for Science and Democracy at the Union of Concerned Scientists and a former fisheries biologist for NOAA. "Their job is not to serve the president but the public interest. Inspector generals are continuing to do what they're supposed to, but their findings are not being adhered to. But they need to hold agencies accountable. If an agency has not met its mission or engaged in misconduct, there needs to be real consequences."
On other fronts, last month nine vaccine makers, including Sanofi, Pfizer, and AstraZeneca, took the unprecedented stop of announcing that their COVID-19 vaccines would be thoroughly vetted before they were released. In their implicit refusal to bow to political pressure from the White House to have a vaccine available before the election, their goal was to restore public confidence in vaccine safety, and ensure that enough Americans would consent to have the shot when it was eventually approved so that we'd reach the long-sought holy grail of herd immunity.
"That's why it's really important that all of the decisions need to be made with complete transparency and not taking shortcuts," says Dr. Tom Frieden, president and CEO of Resolve to Save Lives and former director of the CDC during the H1N1, Ebola, and Zika emergencies. "A vaccine is our most important tool, and we can't break that tool by meddling in the science approval process."
In late September, Senate Democrats introduced a new bill to halt political meddling in public health initiatives by the White House. Called Science and Transparency Over Politics Act (STOP), the legislation would create an independent task force to investigate political interference in the federal response to the coronavirus pandemic. "The Trump administration is still pushing the president's political priorities rather than following the science to defeat this virus," Senate Minority Leader Chuck Schumer said in a press release.
To effectively bring the pandemic under control and restore public confidence, the CDC must assume the leadership role in fighting COVID-19. During previous outbreaks, the top federal infectious disease specialists like Drs. Fauci and Frieden would have daily press briefings, and these need to resume. "The CDC needs to be able to speak regularly to the American people to explain what it knows and how it knows it," says Frieden, who cautions that a vaccine won't be a magic bullet. "There is no one thing that is going to make this virus go away. We need to continue to limit indoor exposures, wear masks, and do strategic testing, isolation, and quarantine. We need a comprehensive approach, and not just a vaccine."
We must also appoint competent and trustworthy leaders, says Rosenberg of the Union of Concerned Scientists. Top posts in too many science agencies are now filled by former industry executives and lobbyists with a built-in bias, as well as people lacking relevant scientific experience, many of whom were never properly vetted because of the current administration's penchant for bypassing Congress and appointing "acting" officials. "We've got great career people who have hung in, but in so much of the federal government, they just put in 'acting' people," says Linda Birnbaum. "They need to bring in better, qualified senior leadership."
Open positions need to be filled, too. Federal science agencies have been seriously crippled by staffing attrition, and the Trump Administration instituted a hiring freeze when it first came in. Staffing levels remain at least ten percent down from previous levels, says Birnbaum and in many agencies, like the EPA, "everything has come to a screeching halt, making it difficult to get anything done."
But in the meantime, the critical first step may be at the ballot box in November. Even Scientific American, the esteemed consumer science publication, for the first time in its 175-year history felt "compelled" to endorse a presidential candidate, Joe Biden, because of the enormity of the damage they say Donald Trump has inflicted on scientists, their legal protections, and on the federal science agencies.
"If the current administration continues, the national political leadership will be emboldened and will be even more assertive of their executive prerogatives and less concerned about traditional niceties, leading to further erosion of the activities of many federal agencies," says Vanderbilt's William Schaffner. "But the reality is, if the team is losing, you change the coach. Then agencies really have to buckle down because it will take some time to restore their hard-earned reputations."
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Announcing "The Future of Science in America: The Election Issue"
This special magazine explores what's at stake for science & policy over the next four years.
As reviewed in The Washington Post, "Tomorrow's challenges in science and politics: Magazine offers in-depth takes on these U.S. issues":
"Is it time for a new way to help make adults more science-literate? What should the next president know about science? Could science help strengthen American democracy? "The Future of Science in America: The Election Issue" has answers. The free, online magazine is packed with interesting takes on how science can serve the common good. And just in time. This year has challenged leaders, researchers and the public with thorny scientific questions, from the coronavirus pandemic to widespread misinformation on scientific issues. The magazine is a collaboration of the Aspen Institute, a think tank that brings together a variety of public figures and private individuals to tackle thorny social issues, the digital science magazine Leapsmag and GOOD, a social impact company. It's packed with 15 in-depth articles about science with a view toward our campaign year."
The Future of Science in America: The Election Issue offers wide-ranging perspectives on challenges and opportunities for science as we elect our next national and local leaders. The fast-striking COVID-19 pandemic and the more slowly moving pandemic of climate change have brought into sharp focus how reliant we will be on science and public policy to work together to rescue us from crisis. Doing so will require cooperation between both political parties, as well as significant public trust in science as a beacon to light the path forward.
In spite of its unfortunate emergence as a flash point between two warring parties, we believe that science is the driving force for universal progress. No endeavor is more noble than the quest to rigorously understand our world and apply that knowledge to further human flourishing. This magazine aspires to promote roadmaps for science as a tool for health, a vehicle for progress, and a unifier of our nation.
This special issue is a collaboration among LeapsMag, the Aspen Institute Science & Society Program, and GOOD, with support from the Gordon and Betty Moore Foundation and the Rita Allen Foundation.
It is available as a free, beautifully designed digital magazine for both desktop and mobile.
TABLE OF CONTENTS:
- SCIENTISTS:
Award-Winning Scientists Offer Advice to the Next President of the United States - PUBLIC OPINION:
National Survey Reveals Americans' Most Important Scientific Priorities - GOVERNMENT:
The Nation's Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored? - TELEVISION:
To Make Science Engaging, We Need a Sesame Street for Adults - IMMIGRATION:
Immigrant Scientists—and America's Edge—Face a Moment of Truth This Election - RACIAL JUSTICE:
Democratize the White Coat by Honoring Black, Indigenous, and People of Color in Science - EDUCATION:
I'm a Black, Genderqueer Medical Student: Here's My Hard-Won Wisdom for Students and Educational Institutions - TECHNOLOGY:
"Deep Fake" Video Technology Is Advancing Faster Than Our Policies Can Keep Up - VOTERS:
Mind the (Vote) Gap: Can We Get More STEM Students to the Polls? - EXPERTS:
Who Qualifies as an "Expert" and How Can We Decide Who Is Trustworthy? - SOCIAL MEDIA:
Why Your Brain Falls for Misinformation—And How to Avoid It - YOUTH:
Youth Climate Activists Expand Their Focus and Collaborate to Get Out the Vote - SUPREME COURT:
Abortions Before Fetal Viability Are Legal: Might Science and a Change on the Supreme Court Undermine That? - NAVAJO NATION:
An Environmental Scientist and an Educator Highlight Navajo Efforts to Balance Tradition with Scientific Priorities - CIVIC SCIENCE:
Want to Strengthen American Democracy? The Science of Collaboration Can Help
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.