How a Deadly Fire Gave Birth to Modern Medicine
The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
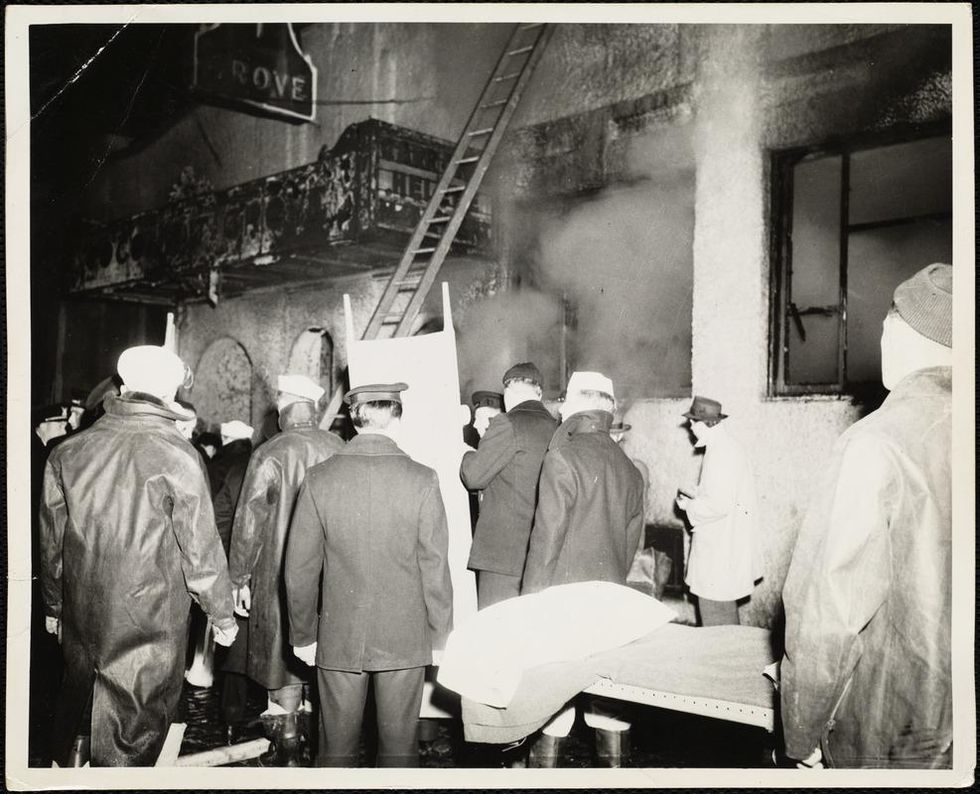
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
New Hope for Organ Transplantation: Life Without Anti-Rejection Drugs
Kidney transplant patient Robert Waddell, center, with his wife and children after being off immunosuppresants; photo aken last summer in Perdido Key, FL. Left to right: Christian, Bailey, Rob, Karen (wife), Robby and Casey.
Rob Waddell dreaded getting a kidney transplant. He suffers from a genetic condition called polycystic kidney disease that causes the uncontrolled growth of cysts that gradually choke off kidney function. The inherited defect has haunted his family for generations, killing his great grandmother, grandmother, and numerous cousins, aunts and uncles.
But he saw how difficult it was for his mother and sister, who also suffer from this condition, to live with the side effects of the drugs they needed to take to prevent organ rejection, which can cause diabetes, high blood pressure and cancer, and even kidney failure because of their toxicity. Many of his relatives followed the same course, says Waddell: "They were all on dialysis, then a transplant and ended up usually dying from cancers caused by the medications."
When the Louisville native and father of four hit 40, his kidneys barely functioned and the only alternative was either a transplant or the slow death of dialysis. But in 2009, when Waddell heard about an experimental procedure that could eliminate the need for taking antirejection drugs, he jumped at the chance to be their first patient. Devised by scientists at the University of Louisville and Northwestern University, the innovative approach entails mixing stem cells from the live kidney donor with that of the recipient to create a hybrid immune system, known as a chimera, that would trick the immune system and prevent it from attacking the implanted kidney.
The procedure itself was done at Northwestern Memorial Hospital in Chicago, using a live kidney donated by a neighbor of Waddell's, who camped out in Chicago during his recovery. Prior to surgery, Waddell underwent a conditioning treatment that consisted of low dose radiation and chemotherapy to weaken his own immune system and make room for the infusion of stem cells.
"The low intensity chemo and radiation conditioning regimen create just enough space for the donor stem cells to gain a foothold in the bone marrow and the donor's immune system takes over," says Dr. Joseph Levanthal, the transplant surgeon who performed the operation and director of kidney and pancreas transplantation at Northwestern University Feinberg School of Medicine. "That way the recipient develops an immune system that doesn't see the donor organ as foreign."
"As a surgeon, I saw what my patients had to go through—taking 25 pills a day, dying at an early age from heart disease, or having a 35% chance of dying every year on dialysis."
A week later, Waddell had the kidney transplant. The following day, he was infused with a complex cellular cocktail that included blood-forming stem cells derived from his donor's bone marrow mixed what are called tolerance inducing facilitator cells (FCs); these cells help the foreign stem cells get established in the recipient's bone marrow.
Over the course of the following year, he was slowly weaned off of antirejection medications—a precaution in case the procedure didn't work—and remarkably, hasn't needed them since. "I felt better than I had in decades because my kidneys [had been] degrading," recalls Waddell, now 54 and a CPA for a global beverage company. And what's even better is that this new approach offers hope for one of his sons who has also inherited the disorder.
Kidney transplants are the most frequent organ transplants in the world and more than 23,000 of these procedures were done in the United States in 2019, according to the United Network for Organ Sharing. Of this, about 7,000 operations are done annually using live organ donors; the remainder use organs from people who are deceased. Right now, this revolutionary new approach—as well as a similar strategy formulated by Stanford University scientists--is in the final phase of clinical trials. Ultimately, this research may pave the way towards realizing the holy grail of organ transplantation: preventing organ rejection by creating a tolerant state in which the recipient's immune system is compatible with the donor, which would eliminate the need for a lifetime of medications.
"As a surgeon, I saw what my patients had to go through—taking 25 pills a day, dying at an early age from heart disease, or having a 35% chance of dying every year on dialysis," says Dr. Suzanne Ildstad, a transplant surgeon and director of the Institute for Cellular Therapeutics at the University of Louisville, whose discovery of facilitator cells were the basis for this therapeutic platform. Ildstad, who has spent more than two decades searching for a better way, says, "This is something I have worked for my entire life."
The Louisville group uses a combination of chemo and radiation to replace the recipient's immune and blood forming cells with that of the donor. In contrast, the Stanford protocol involves harvesting the donor's blood stem cells and T-cells, which are the foot soldiers of the immune system that fight off infections and would normally orchestrate the rejection of the transplanted organ. Their transplant recipients undergo a milder form of "conditioning" that only radiates discrete parts of the body and selectively targets the recipient's T-cells, creating room for both sets of T-cells, a strategy these researchers believe has a better safety profile and less of a chance of rejection.
"We try to achieve immune tolerance by a true chimerism," says Dr. Samuel Strober, a professor of medicine for immunology and rheumatology at Stanford University and a leader of this research team. "The recipients immune system cells are maintained but mixed in the blood with that of the donor."
Studies suggest both approaches work. In a 2018 clinical trial conducted by Talaris Therapeutics, a Louisville-based biotech founded by Ildstad, 26 of 37 (70%) of the live donor kidney transplant recipients no longer need immunosuppressants.Last fall, Talaris began the final phase of clinical tests that will eventually encompass more than 120 such patients.
The Stanford group's cell-based immunotherapy, which is called MDR-101 and is sponsored by the South San Francisco biotech, Medeor Therapeutics, has had similar results in patients who received organs from live donors who were either well matched, such as one from siblings, meaning they were immunologically identical, or partially matched; Talaris uses unrelated donors where there is only a partial match.
In their 2020 clinical trial of 51 patients, 29 were fully matched and 22 were a partial match; 22 of the fully matched recipients didn't need antirejection drugs and ten of the partial matches were able to stop taking some of these medications without rejection. "With our fully matched, roughly 80% have been completely off drugs up to 14 years later," says Strober, "and reducing the number of drugs from three to one [in the partial matches] means you have far fewer side effects. The goal is to get them off of all drugs."
But these protocols are limited to a small number of patients—living donor kidney recipients. As a consequence, both teams are experimenting with ways to broaden their approach so they can use cadaver organs from deceased donors, with human tests planned in the coming year. Here's how that would work: after the other organs are removed from a deceased donor, stem cells are harvested from the donor's vertebrae in the spinal column and then frozen for storage.
"We do the transplant and give the patient a chance to recover and maintain them on drugs," says Ildstad. "Then we do the tolerance conditioning at a later stage."
If this strategy is successful, it would be a genuine game changer, and open the door to using these protocols for transplanting other cadaver organs, including the heart, lungs and liver. While the overall procedure is complex and costly, in the long run it's less expensive than repeated transplant surgeries, the cost of medications and hospitalizations for complications caused by the drugs, or thrice weekly dialysis treatments, says Ildstad.
And she adds, you can't put a price tag on the vast improvement in quality of life.
The Nation’s Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored?
Morale at federal science agencies -- and public trust in their guidance -- is at a concerning low right now.
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
It didn't have to be this way. More than 200,000 Americans dead, seven million infected, with numbers continuing to climb, an economy in shambles with millions out of work, hundreds of thousands of small businesses crushed with most of the country still under lockdown. And all with no end in sight. This catastrophic result is due in large part to the willful disregard of scientific evidence and of muzzling policy experts by the Trump White House, which has spent its entire time in office attacking science.
One of the few weapons we had to combat the spread of Covid-19—wearing face masks—has been politicized by the President, who transformed this simple public health precaution into a first amendment issue to rally his base. Dedicated public health officials like Dr. Anthony Fauci, the highly respected director of the National Institute of Allergies and Infectious Diseases, have received death threats, which have prompted many of them around the country to resign.
Over the summer, the Trump White House pressured the Centers for Disease Control, which is normally in charge of fighting epidemics, to downplay COVID risks among young people and encourage schools to reopen. And in late September, the CDC was forced to pull federal teams who were going door-to-door doing testing surveys in Minnesota because of multiple incidents of threats and abuse. This list goes on and on.
Still, while the Trump administration's COVID failures are the most visible—and deadly—the nation's entire federal science infrastructure has been undermined in ways large and small.
The White House has steadily slashed monies for science—the 2021 budget cuts funding by 10–30% or more for crucial agencies like National Oceanic and Atmospheric Administration (NOAA) and the Environmental Protection Agency (EPA)—and has gutted health and science agencies across the board, including key agencies of the Department of Energy and the Interior, especially in divisions that deal with issues they oppose ideologically like climate change.
Even farmers can't get reliable information about how climate change affects planting seasons because the White House moved the entire staff at the U.S. Department of Agriculture agency who does this research, relocating them from Maryland to Kansas City, Missouri. Many of these scientists couldn't uproot their families and sell their homes, so the division has had to pretty much start over from scratch with a skeleton crew.
More than 1,600 federal scientists left government in the first two years of the Trump Administration, according to data compiled by the Washington Post, and one-fifth of top positions in science are vacant, depriving agencies of the expertise they need to fulfill their vital functions. Industry executives and lobbyists have been installed as gatekeepers—HHS Secretary Alex Azar was previously president of Eli Lilly, and three climate change deniers were appointed to key posts at the National Oceanic and Atmospheric Administration, to cite just a couple of examples. Trump-appointed officials have sidelined, bullied, or even vilified those who dare to speak out, which chills the rigorous debate that is the essential to sound, independent science.
"The CDC needs to be able to speak regularly to the American people to explain what it knows and how it knows it."
Linda Birnbaum knows firsthand what it's like to become a target. The microbiologist recently retired after more than a decade as the director of the National Institute of Environmental Health Sciences, which is the world's largest environmental health organization and the greatest funder of environmental health and toxicology research, a position that often put her agency at odds with the chemical and fossil fuel industry. There was an attempt to get her fired, she says, "because I had the nerve to write that science should be used in making policy. The chemical industry really went after me, and my last two years were not so much fun under this administration. I'd like to believe it was because I was making a difference—if I wasn't, they wouldn't care."
Little wonder that morale at federal agencies is low. "We're very frustrated," says Dr. William Schaffner, a veteran infectious disease specialist and a professor of medicine at the Vanderbilt University School of Medicine in Nashville. "My colleagues within these agencies, the CDC rank and file, are keeping their heads down doing the best they can, and they hope to weather this storm."
The cruel irony is that the United States was once a beacon of scientific innovation. In the heady post World War II years, while Europe lay in ruins, the successful development of penicillin and the atomic bomb—which Americans believed helped vanquish the Axis powers—unleashed a gusher of public money into research, launching an unprecedented era of achievement in American science. Scientists conquered polio, deciphered the genetic code, harnessed the power of the atom, invented lasers, transistors, microchips and computers, sent missions beyond Mars, and landed men on the moon. A once-inconsequential hygiene laboratory was transformed into the colossus the National Institutes of Health has become, which remains today the world's flagship medical research center, unrivaled in size and scope.
At the same time, a tiny public health agency headquartered in Atlanta, which had been in charge of eradicating the malaria outbreaks that plagued impoverished rural areas in the Deep South until the late 1940s, evolved into the Centers for Disease Control and Prevention. The CDC became the world's leader in fighting disease outbreaks, and the agency's crack team of epidemiologists—members of the vaunted Epidemic Intelligence Service—were routinely dispatched to battle global outbreaks of contagions such as Ebola and malaria and help lead the vaccination campaigns to eradicate killers like polio and small pox that have saved millions of lives.
What will it take to rebuild our federal science infrastructure and restore not only the public's confidence but the respect of the world's scientific community? There are some hopeful signs that there is pushback against the current national leadership, and non-profit watchdog groups like the Union of Concerned Scientists have mapped out comprehensive game plans to restore public trust and the integrity of science.
These include methods of protecting science from political manipulation; restoring the oversight role of independent federal advisory committees, whose numbers were decimated by recent executive orders; strengthening scientific agencies that have been starved by budget cuts and staff attrition; and supporting whistleblower protections and allowing scientists to do their jobs without political meddling to restore integrity to the process. And this isn't just a problem at the CDC. A survey of 1,600 EPA scientists revealed that more than half had been victims of political interference and were pressured to skew their findings, according to research released in April by the Union of Concerned Scientists.
"Federal agencies are staffed by dedicated professionals," says Andrew Rosenberg, director of the Center for Science and Democracy at the Union of Concerned Scientists and a former fisheries biologist for NOAA. "Their job is not to serve the president but the public interest. Inspector generals are continuing to do what they're supposed to, but their findings are not being adhered to. But they need to hold agencies accountable. If an agency has not met its mission or engaged in misconduct, there needs to be real consequences."
On other fronts, last month nine vaccine makers, including Sanofi, Pfizer, and AstraZeneca, took the unprecedented stop of announcing that their COVID-19 vaccines would be thoroughly vetted before they were released. In their implicit refusal to bow to political pressure from the White House to have a vaccine available before the election, their goal was to restore public confidence in vaccine safety, and ensure that enough Americans would consent to have the shot when it was eventually approved so that we'd reach the long-sought holy grail of herd immunity.
"That's why it's really important that all of the decisions need to be made with complete transparency and not taking shortcuts," says Dr. Tom Frieden, president and CEO of Resolve to Save Lives and former director of the CDC during the H1N1, Ebola, and Zika emergencies. "A vaccine is our most important tool, and we can't break that tool by meddling in the science approval process."
In late September, Senate Democrats introduced a new bill to halt political meddling in public health initiatives by the White House. Called Science and Transparency Over Politics Act (STOP), the legislation would create an independent task force to investigate political interference in the federal response to the coronavirus pandemic. "The Trump administration is still pushing the president's political priorities rather than following the science to defeat this virus," Senate Minority Leader Chuck Schumer said in a press release.
To effectively bring the pandemic under control and restore public confidence, the CDC must assume the leadership role in fighting COVID-19. During previous outbreaks, the top federal infectious disease specialists like Drs. Fauci and Frieden would have daily press briefings, and these need to resume. "The CDC needs to be able to speak regularly to the American people to explain what it knows and how it knows it," says Frieden, who cautions that a vaccine won't be a magic bullet. "There is no one thing that is going to make this virus go away. We need to continue to limit indoor exposures, wear masks, and do strategic testing, isolation, and quarantine. We need a comprehensive approach, and not just a vaccine."
We must also appoint competent and trustworthy leaders, says Rosenberg of the Union of Concerned Scientists. Top posts in too many science agencies are now filled by former industry executives and lobbyists with a built-in bias, as well as people lacking relevant scientific experience, many of whom were never properly vetted because of the current administration's penchant for bypassing Congress and appointing "acting" officials. "We've got great career people who have hung in, but in so much of the federal government, they just put in 'acting' people," says Linda Birnbaum. "They need to bring in better, qualified senior leadership."
Open positions need to be filled, too. Federal science agencies have been seriously crippled by staffing attrition, and the Trump Administration instituted a hiring freeze when it first came in. Staffing levels remain at least ten percent down from previous levels, says Birnbaum and in many agencies, like the EPA, "everything has come to a screeching halt, making it difficult to get anything done."
But in the meantime, the critical first step may be at the ballot box in November. Even Scientific American, the esteemed consumer science publication, for the first time in its 175-year history felt "compelled" to endorse a presidential candidate, Joe Biden, because of the enormity of the damage they say Donald Trump has inflicted on scientists, their legal protections, and on the federal science agencies.
"If the current administration continues, the national political leadership will be emboldened and will be even more assertive of their executive prerogatives and less concerned about traditional niceties, leading to further erosion of the activities of many federal agencies," says Vanderbilt's William Schaffner. "But the reality is, if the team is losing, you change the coach. Then agencies really have to buckle down because it will take some time to restore their hard-earned reputations."
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]


