Meet the Scientists on the Frontlines of Protecting Humanity from a Man-Made Pathogen
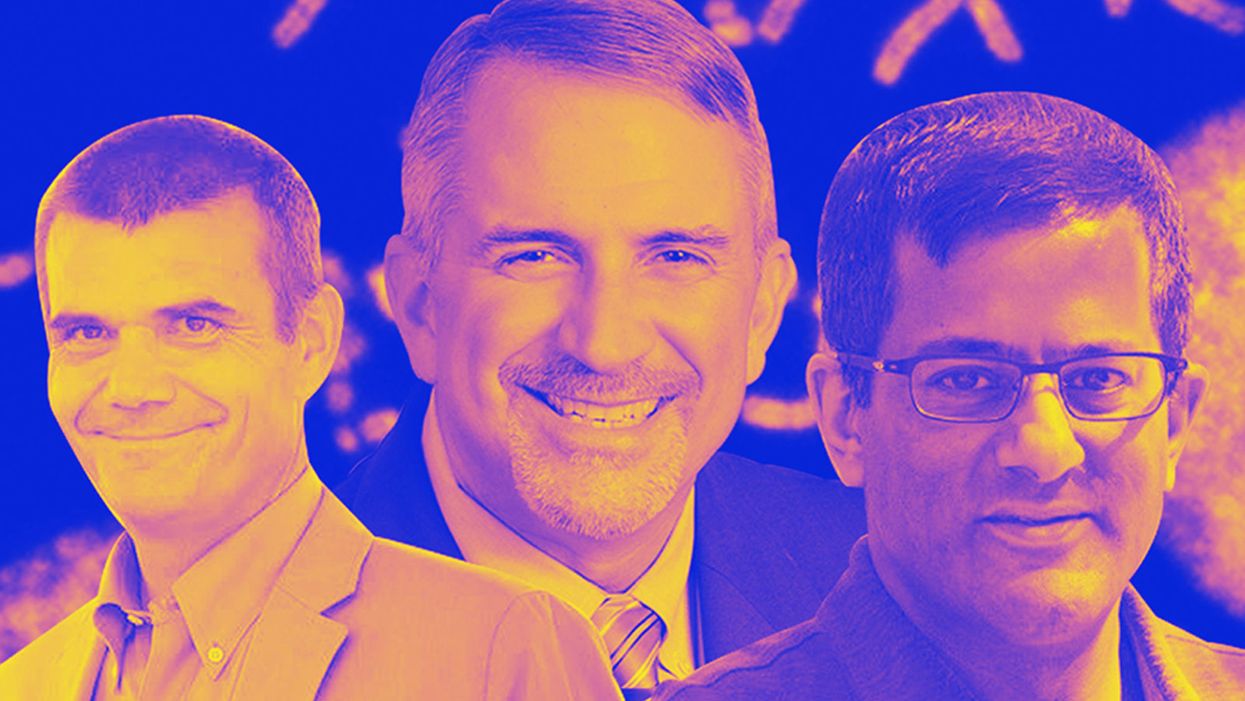
From left: Jean Peccoud, Randall Murch, and Neeraj Rao.
Jean Peccoud wasn't expecting an email from the FBI. He definitely wasn't expecting the agency to invite him to a meeting. "My reaction was, 'What did I do wrong to be on the FBI watch list?'" he recalls.
You use those blueprints for white-hat research—which is, indeed, why the open blueprints exist—or you can do the same for a black-hat attack.
He didn't know what the feds could possibly want from him. "I was mostly scared at this point," he says. "I was deeply disturbed by the whole thing."
But he decided to go anyway, and when he traveled to San Francisco for the 2008 gathering, the reason for the e-vite became clear: The FBI was reaching out to researchers like him—scientists interested in synthetic biology—in anticipation of the potential nefarious uses of this technology. "The whole purpose of the meeting was, 'Let's start talking to each other before we actually need to talk to each other,'" says Peccoud, now a professor of chemical and biological engineering at Colorado State University. "'And let's make sure next time you get an email from the FBI, you don't freak out."
Synthetic biology—which Peccoud defines as "the application of engineering methods to biological systems"—holds great power, and with that (as always) comes great responsibility. When you can synthesize genetic material in a lab, you can create new ways of diagnosing and treating people, and even new food ingredients. But you can also "print" the genetic sequence of a virus or virulent bacterium.
And while it's not easy, it's also not as hard as it could be, in part because dangerous sequences have publicly available blueprints. You use those blueprints for white-hat research—which is, indeed, why the open blueprints exist—or you can do the same for a black-hat attack. You could synthesize a dangerous pathogen's code on purpose, or you could unwittingly do so because someone tampered with your digital instructions. Ordering synthetic genes for viral sequences, says Peccoud, would likely be more difficult today than it was a decade ago.
"There is more awareness of the industry, and they are taking this more seriously," he says. "There is no specific regulation, though."
Trying to lock down the interconnected machines that enable synthetic biology, secure its lab processes, and keep dangerous pathogens out of the hands of bad actors is part of a relatively new field: cyberbiosecurity, whose name Peccoud and colleagues introduced in a 2018 paper.
Biological threats feel especially acute right now, during the ongoing pandemic. COVID-19 is a natural pathogen -- not one engineered in a lab. But future outbreaks could start from a bug nature didn't build, if the wrong people get ahold of the right genetic sequences, and put them in the right sequence. Securing the equipment and processes that make synthetic biology possible -- so that doesn't happen -- is part of why the field of cyberbiosecurity was born.
The Origin Story
It is perhaps no coincidence that the FBI pinged Peccoud when it did: soon after a journalist ordered a sequence of smallpox DNA and wrote, for The Guardian, about how easy it was. "That was not good press for anybody," says Peccoud. Previously, in 2002, the Pentagon had funded SUNY Stonybrook researchers to try something similar: They ordered bits of polio DNA piecemeal and, over the course of three years, strung them together.
Although many years have passed since those early gotchas, the current patchwork of regulations still wouldn't necessarily prevent someone from pulling similar tricks now, and the technological systems that synthetic biology runs on are more intertwined — and so perhaps more hackable — than ever. Researchers like Peccoud are working to bring awareness to those potential problems, to promote accountability, and to provide early-detection tools that would catch the whiff of a rotten act before it became one.
Peccoud notes that if someone wants to get access to a specific pathogen, it is probably easier to collect it from the environment or take it from a biodefense lab than to whip it up synthetically. "However, people could use genetic databases to design a system that combines different genes in a way that would make them dangerous together without each of the components being dangerous on its own," he says. "This would be much more difficult to detect."
After his meeting with the FBI, Peccoud grew more interested in these sorts of security questions. So he was paying attention when, in 2010, the Department of Health and Human Services — now helping manage the response to COVID-19 — created guidance for how to screen synthetic biology orders, to make sure suppliers didn't accidentally send bad actors the sequences that make up bad genomes.
Guidance is nice, Peccoud thought, but it's just words. He wanted to turn those words into action: into a computer program. "I didn't know if it was something you can run on a desktop or if you need a supercomputer to run it," he says. So, one summer, he tasked a team of student researchers with poring over the sentences and turning them into scripts. "I let the FBI know," he says, having both learned his lesson and wanting to get in on the game.
Peccoud later joined forces with Randall Murch, a former FBI agent and current Virginia Tech professor, and a team of colleagues from both Virginia Tech and the University of Nebraska-Lincoln, on a prototype project for the Department of Defense. They went into a lab at the University of Nebraska at Lincoln and assessed all its cyberbio-vulnerabilities. The lab develops and produces prototype vaccines, therapeutics, and prophylactic components — exactly the kind of place that you always, and especially right now, want to keep secure.
"We were creating wiki of all these nasty things."
The team found dozens of Achilles' heels, and put them in a private report. Not long after that project, the two and their colleagues wrote the paper that first used the term "cyberbiosecurity." A second paper, led by Murch, came out five months later and provided a proposed definition and more comprehensive perspective on cyberbiosecurity. But although it's now a buzzword, it's the definition, not the jargon, that matters. "Frankly, I don't really care if they call it cyberbiosecurity," says Murch. Call it what you want: Just pay attention to its tenets.
A Database of Scary Sequences
Peccoud and Murch, of course, aren't the only ones working to screen sequences and secure devices. At the nonprofit Battelle Memorial Institute in Columbus, Ohio, for instance, scientists are working on solutions that balance the openness inherent to science and the closure that can stop bad stuff. "There's a challenge there that you want to enable research but you want to make sure that what people are ordering is safe," says the organization's Neeraj Rao.
Rao can't talk about the work Battelle does for the spy agency IARPA, the Intelligence Advanced Research Projects Activity, on a project called Fun GCAT, which aims to use computational tools to deep-screen gene-sequence orders to see if they pose a threat. It can, though, talk about a twin-type internal project: ThreatSEQ (pronounced, of course, "threat seek").
The project started when "a government customer" (as usual, no one will say which) asked Battelle to curate a list of dangerous toxins and pathogens, and their genetic sequences. The researchers even started tagging sequences according to their function — like whether a particular sequence is involved in a germ's virulence or toxicity. That helps if someone is trying to use synthetic biology not to gin up a yawn-inducing old bug but to engineer a totally new one. "How do you essentially predict what the function of a novel sequence is?" says Rao. You look at what other, similar bits of code do.
"We were creating wiki of all these nasty things," says Rao. As they were working, they realized that DNA manufacturers could potentially scan in sequences that people ordered, run them against the database, and see if anything scary matched up. Kind of like that plagiarism software your college professors used.
Battelle began offering their screening capability, as ThreatSEQ. When customers -- like, currently, Twist Bioscience -- throw their sequences in, and get a report back, the manufacturers make the final decision about whether to fulfill a flagged order — whether, in the analogy, to give an F for plagiarism. After all, legitimate researchers do legitimately need to have DNA from legitimately bad organisms.
"Maybe it's the CDC," says Rao. "If things check out, oftentimes [the manufacturers] will fulfill the order." If it's your aggrieved uncle seeking the virulent pathogen, maybe not. But ultimately, no one is stopping the manufacturers from doing so.
Beyond that kind of tampering, though, cyberbiosecurity also includes keeping a lockdown on the machines that make the genetic sequences. "Somebody now doesn't need physical access to infrastructure to tamper with it," says Rao. So it needs the same cyber protections as other internet-connected devices.
Scientists are also now using DNA to store data — encoding information in its bases, rather than into a hard drive. To download the data, you sequence the DNA and read it back into a computer. But if you think like a bad guy, you'd realize that a bad guy could then, for instance, insert a computer virus into the genetic code, and when the researcher went to nab her data, her desktop would crash or infect the others on the network.
Something like that actually happened in 2017 at the USENIX security symposium, an annual programming conference: Researchers from the University of Washington encoded malware into DNA, and when the gene sequencer assembled the DNA, it corrupted the sequencer's software, then the computer that controlled it.
"This vulnerability could be just the opening an adversary needs to compromise an organization's systems," Inspirion Biosciences' J. Craig Reed and Nicolas Dunaway wrote in a paper for Frontiers in Bioengineering and Biotechnology, included in an e-book that Murch edited called Mapping the Cyberbiosecurity Enterprise.
Where We Go From Here
So what to do about all this? That's hard to say, in part because we don't know how big a current problem any of it poses. As noted in Mapping the Cyberbiosecurity Enterprise, "Information about private sector infrastructure vulnerabilities or data breaches is protected from public release by the Protected Critical Infrastructure Information (PCII) Program," if the privateers share the information with the government. "Government sector vulnerabilities or data breaches," meanwhile, "are rarely shared with the public."
"What I think is encouraging right now is the fact that we're even having this discussion."
The regulations that could rein in problems aren't as robust as many would like them to be, and much good behavior is technically voluntary — although guidelines and best practices do exist from organizations like the International Gene Synthesis Consortium and the National Institute of Standards and Technology.
Rao thinks it would be smart if grant-giving agencies like the National Institutes of Health and the National Science Foundation required any scientists who took their money to work with manufacturing companies that screen sequences. But he also still thinks we're on our way to being ahead of the curve, in terms of preventing print-your-own bioproblems: "What I think is encouraging right now is the fact that we're even having this discussion," says Rao.
Peccoud, for his part, has worked to keep such conversations going, including by doing training for the FBI and planning a workshop for students in which they imagine and work to guard against the malicious use of their research. But actually, Peccoud believes that human error, flawed lab processes, and mislabeled samples might be bigger threats than the outside ones. "Way too often, I think that people think of security as, 'Oh, there is a bad guy going after me,' and the main thing you should be worried about is yourself and errors," he says.
Murch thinks we're only at the beginning of understanding where our weak points are, and how many times they've been bruised. Decreasing those contusions, though, won't just take more secure systems. "The answer won't be technical only," he says. It'll be social, political, policy-related, and economic — a cultural revolution all its own.
A Doctor Who Treated His Own Rare Disease Is Tracking COVID-19 Treatments Hiding In Plain Sight
Dr. David Fajgenbaum looking through a microscope at his lab.
In late March, just as the COVID-19 pandemic was ramping up in the United States, David Fajgenbaum, a physician-scientist at the University of Pennsylvania, devised a 10-day challenge for his lab: they would sift through 1,000 recently published scientific papers documenting cases of the deadly virus from around the world, pluck out the names of any drugs used in an attempt to cure patients, and track the treatments and their outcomes in a database.
Before late 2019, no one had ever had to treat this exact disease before, which meant all treatments would be trial and error. Fajgenbaum, a pioneering researcher in the field of drug repurposing—which prioritizes finding novel uses for existing drugs, rather than arduously and expensively developing new ones for each new disease—knew that physicians around the world would be embarking on an experimental journey, the scale of which would be unprecedented. His intention was to briefly document the early days of this potentially illuminating free-for-all, as a sidebar to his primary field of research on a group of lymph node disorders called Castleman disease. But now, 11 months and 29,000 scientific papers later, he and his team of 22 are still going strong.
They're running a publicly accessible database called the CORONA Project (COvid19 Registry of Off-label & New Agents) that to date tracks 400 different COVID-19 treatments that have been tried somewhere in the world, along with the frequency of their use, and the outcomes.
"There's so many drugs being used all over the place, in different ways, with different outcomes," says Fajgenbaum. "We're trying to add some order to the madness."
20,000 people have accessed the registry—other physicians and researchers, those in the pharmaceutical industry, and even curious lay people—and the data are now being shared with the U.S. Food and Drug Administration in the hopes of launching large-scale trials that would lead to approving a constellation of treatment options for COVID-19 faster than any new drugs could come online.
"What David's group has done with the CORONA Project is on a scale that I don't think has ever been seen before," says Heather Stone, a health science policy analyst at the FDA who specializes in drug repurposing. She was not involved in establishing the project, but is now working with its data. "To collect and collate that information and make it openly accessible is a massive feat, and a huge benefit to the medical community," she says.
On a Personal Mission
In the science and medical world, Fajgenbaum lives a dual existence: he is both researcher and subject, physician and patient. In July 2010, when he was a healthy and physically fit 25-year-old finishing medical school, he began living through what would become a recurring, unprovoked, and overzealous immune response that repeatedly almost killed him.
His lymph nodes were inflamed; his liver, kidneys, and bone marrow were faltering; and he was dead tired all the time. At first his doctors mistook his mysterious illness for lymphoma, but his inflamed lymph nodes were merely a red herring. A month after his initial hospitalization, pathologists at Mayo Clinic finally diagnosed him with idiopathic multicentric Castleman disease—a particularly ruthless form of a class of lymph node disorders that doesn't just attack one part of the body, but many, and has no known cause. It's a rare diagnosis within an already rare set of disorders. Only about 1,500 Americans a year receive the same diagnosis.
Without many options for treatment, Fajgenbaum underwent recurring rounds of chemotherapy. Each time, the treatment would offer temporary respite from Castleman symptoms, but bring the full spate of chemotherapy side effects. And it wasn't a sustainable treatment for the long haul. Regularly dousing a person's cells in unmitigated toxicity was about as elegant a solution to Fajgenbaum's disease as bulldozing a house in response to a toaster fire. The fire might go out (though not necessarily), but the house would be destroyed.
A swirl of exasperation and doggedness finally propelled Fajgenbaum to take on a crucial question himself: Among all of the already FDA-approved drugs on the market, was there something out there, labeled for another use, that could beat back Castleman disease and that he could tolerate long-term? After months of research, he discovered the answer: sirolimus, a drug normally prescribed to patients receiving a kidney transplant, could be used to suppress his overactive immune system with few known side effects to boot.
Fajgenbaum became hellbent on devoting his practice and research to making similar breakthroughs for others. He founded the Castleman Disease Collaborative Network, to coordinate the research of others studying this bewildering disease, and directs a laboratory consumed with studying cytokine storms—out-of-control immune responses characterized by the body's release of cytokines, proteins that the immune system secretes and uses to communicate with and direct other cells.
In the spring of 2020, when cytokine storms emerged as a hallmark of the most severe and deadly cases of COVID-19, Fajgenbaum's ears perked up. Although SARS-CoV-2 itself was novel, Fajgenbaum already had almost a decade of experience battling the most severe biological forces it brought. Only this time, he thought, it might actually be easier to pinpoint a treatment—unlike Castleman disease, which has no known cause, at least here a virus was clearly the instigator.
"Because [a drug] looks promising, we need to do a well-designed, large randomized controlled trial to really investigate whether this drug works or not ... We don't use that to say, 'You should take it.'"
Thinking Beyond COVID
The week of March 13, when the World Health Organization declared COVID-19 a pandemic, Fajgenbaum found himself hoping that someone would make the same connection and apply the research to COVID. "Then like a minute later I was like, 'Why am I hoping that someone, somewhere, either follows our footsteps, or has a similar background to us? Maybe we just need to do it," he says. And the CORONA Project was born—first as a 10-day exercise, and later as the robust, interactive tool it now is.
All of the 400 treatments in the CORONA database are examples of repurposed drugs, or off-label uses: physicians are prescribing drugs to treat COVID that have been approved for a different disease. There are no bonafide COVID treatments, only inferences. The goal for people like Fajgenbaum and Stone is to identify potential treatments for further study and eventual official approval, so that physicians can treat the disease with a playbook in hand. When it works, drug repurposing opens up a way to move quickly: A range of treatments could be available to patients within just a few years of a totally new virus entering our reality compared with the 12 - 19 years new drug development takes.
"Companies for many decades have explored the use of their products for not just a single indication but often for many indications," says Stone. "'Supplemental approvals' are all essentially examples of drug repurposing, we just didn't call it that. The challenge, I think, is to explore those opportunities more comprehensively and systematically to really try to understand the full breadth of potential activity of any drug or molecule."

The left column shows the path of a repurposed drug, and on the right is the path of a newly discovered and developed drug.
Cures Within Reach
In Fajgenbaum's primary work, promising drugs stand out easily. For a disease like Castleman, where improvement almost never occurs on its own, any improvement that follows a treatment can pretty clearly be attributed to that treatment. But Fajgenbaum says tracking COVID outcomes is less straightforward since "the vast majority of people will get better, whether they take steroids or they take Skittles." That's why the intent of the database is to identify promising treatments only to generate hypotheses and fruitful clinical trials, not to offer full-throated treatment recommendations. Within the registry, Fajgenbaum considers a drug promising if it's being used in humans, not just in lab animals, and a significant proportion of cases report patient improvement.
"It's that sort of combination of rock-solid randomized controlled trial data, plus anecdotal retrospective data, that we combine to say, 'Wow, this drug looks more promising than another,'" says Fajgenbaum. "Because it looks promising, we need to do a well-designed, large randomized controlled trial to really investigate whether this drug works or not ... We don't use that to say, 'You should take it.'"
Experts say that the search for repurposed drugs to treat COVID could have implications for rare diseases in general. Rare diseases, of which Castleman is one, affect 400 million people around the world. 95% of them don't have a tailor-made, FDA-approved drug treatment. Developing one is a lengthy and often prohibitively expensive process. If only a dozen people will benefit from and buy a drug, it's not often worth it to pharmaceutical companies to spend millions of dollars making them. On occasion when they do, however, that overhead shows up in the price tag: the top 10 most expensive drugs in the world are all for rare diseases, often making them inaccessible to patients. Identifying new clinical uses for drugs that already exist is critical for opening a trap door out of a cycle that prioritizes profits over health outcomes.
"COVID is an interesting case where it's demonstrated that when the scientific and medical community really focuses all of its efforts and talents on a single problem, a solution can be identified and in a much faster time period than has ever historically been the case," says Stone. "I certainly wish it hadn't taken a pandemic to do that, but I think it does have lessons for the future in terms of our ability to accomplish things that we might have previously not thought were possible"—for example, mainstreaming the idea of drug repurposing as a treatment tool, even long after the pandemic subsides.
A Confounding Virus
The FDA declined to comment on what drugs it was fast-tracking for trials, but Fajgenbaum says that based on the CORONA Project's data, which includes data from smaller trials that have already taken place, he feels there are three drugs that seem the most clearly and broadly promising for large-scale studies. Among them are dexamethasone, which is a steroid with anti-inflammatory effects, and baricitinib, a rheumatoid arthritis drug, both of which have enabled the sickest COVID-19 patients to bounce back by suppressing their immune systems. The third most clearly promising drug is heparin, a blood thinner, which a recent trial showed to be most helpful when administered at a full dose, more so than at a small, preventative dose. (On the flipside, Fajgenbaum says "it's a little sad" that in the database you can see hydroxychloroquine is still the most-prescribed drug being tried as a COVID treatment around the world, despite over the summer being debunked widely as an effective treatment, and continuously since then.)
One of the confounding attributes of SARS-CoV-2 is its ability to cause such a huge spectrum of outcomes. It's unlikely a silver bullet treatment will emerge under that reality, so the database also helps surface drugs that seem most promising for a specific population. Fluvoxamine, a selective serotonin reuptake inhibitor used to treat obsessive compulsive disorder, showed promise in the recovery of outpatients—those who were sick, but not severely enough to be hospitalized. Tocilizumab, which was actually developed for Castleman disease, the disease Fajgenbaum is managing, was initially written off as a COVID treatment because it failed to benefit large portions of hospitalized patients, but now seems to be effective if used on intensive care unit patients within 24 hours of admission—these are some of the sickest patients with the highest risk of dying.
Other than fluvoxamine, most of the drugs labeled as promising do skew toward targeting hospitalized patients, more than outpatients. One reason, Fajgenbaum says, is that "if you're in a hospital it's very easy to give you a drug and to track you, and there are very objective measurements as to whether you die, you progress to a ventilator, etc." Tracking outpatients is far more difficult, especially when folks have been routinely asked to stay home, quarantine, and free up hospital resources if they're experiencing only mild symptoms.
But the other reason for the skew is because COVID is very unlike most other diseases in terms of the human immune response the virus triggers. For example, if oncology treatments show some benefit to people with the highest risk of dying, then they usually work extremely well if administered in the earlier stages of a cancer diagnosis. Across many diseases, this dialing backward is a standard approach to identifying promising treatments. With COVID, all of that reasoning has proven moot.
As we've seen over the last year, COVID cases often start as asymptomatic, and remain that way for days, indicating the body is mounting an incredibly weak immune response initially. Then, between days five and 14, as if trying to make up for lost time, the immune system overcompensates by launching a major inflammatory response, which in the sickest patient can lead to the type of cytokine storms that helped Fajgenbaum realize his years of Castleman research might be useful during this public health crisis. Because of this phased response, you can't apply the same treatment logic to all cases.
"In COVID, drugs that work late tend to not work if given early, and drugs that work early tend to not work if given late," says Fajgenbaum. "Generally this … is not a commonplace thing for a virus."
"There are drugs that are literally sitting in every single hospital pharmacy in the country that, if a study shows it's effective, can be deployed that evening to patients on a massive scale."
This see-sawing necessitates tracking a constellation of drugs that might work for different stages of the disease as a patient moves from the weak immune response stage into the overzealous immune response.
"COVID is difficult, compared to other diseases, because there are so many different levels of disease severity, and recovery at different rates," says Stone, the FDA researcher. "That makes it hard to see the patterns or signals and it makes it very important to collect very, very large numbers of cases in order to really reliably identify signals."
This particular moment in the pandemic feels like a massive tipping point, or the instant a tiny pinprick of light finally appeared at the end of the tunnel: several vaccines are already here, with more on the way imminently. In the U.S., more than 65 million doses of the vaccine have been administered, and positive COVID cases are finally falling back to levels not seen since October. On the hopeful surface, it might seem a strange moment to be preparing to launch trials that will validate treatments for a virus it seems the U.S. may finally be beating back. But at best, Americans are still months away from reaching herd immunity through vaccination, and new circulating variants may threaten to upend our fragile progress.
"In the meantime, there are drugs that are literally sitting in every single hospital pharmacy in the country that, if a study shows it's effective, can be deployed that evening to patients on a massive scale. It wouldn't have to be newly produced, it wouldn't have to be shipped, it's literally there already," says Fajgenbaum. "The idea that you can save a lot of lives by finding things that are just already there I think is really compelling, given how many people are going to die over these next few months."
Even after that, not everyone can or will be vaccinated, and, as the Wall Street Journal recently reported, "The pathogen will circulate for years, or even decades, leaving society to coexist with Covid-19 much as it does with other endemic diseases like flu, measles, and HIV." Neither vaccines, personal behavior, or treatments alone is a panacea against the virus, but together they might be.
"It's important to explore all avenues in this public health emergency, and drug repurposing can continue to play a role as the pandemic continues and evolves," says Stone. "I think COVID variants in particular are a big concern at the moment, and therefore continuing to investigate new therapeutics, even as the vaccines roll out, will continue to be a priority."
How a Nobel-Prize Winner Fought Her Family, Nazis, and Bombs to Change our Understanding of Cells Forever
Rita Levi-Montalcini survived the Nazis and eventually won a Nobel Prize for her work to understand why certain cells grow so quickly.
When Rita Levi-Montalcini decided to become a scientist, she was determined that nothing would stand in her way. And from the beginning, that determination was put to the test. Before Levi-Montalcini became a Nobel Prize-winning neurobiologist, the first to discover and isolate a crucial chemical called Neural Growth Factor (NGF), she would have to battle both the sexism within her own family as well as the racism and fascism that was slowly engulfing her country
Levi-Montalcini was born to two loving parents in Turin, Italy at the turn of the 20th century. She and her twin sister, Paola, were the youngest of the family's four children, and Levi-Montalcini described her childhood as "filled with love and reciprocal devotion." But while her parents were loving, supportive and "highly cultured," her father refused to let his three daughters engage in any schooling beyond the basics. "He loved us and had a great respect for women," she later explained, "but he believed that a professional career would interfere with the duties of a wife and mother."
At age 20, Levi-Montalcini had finally had enough. "I realized that I could not possibly adjust to a feminine role as conceived by my father," she is quoted as saying, and asked his permission to finish high school and pursue a career in medicine. When her father reluctantly agreed, Levi-Montalcini was ecstatic: In just under a year, she managed to catch up on her mathematics, graduate high school, and enroll in medical school in Turin.
By 1936, Levi-Montalcini had graduated medical school at the top of her class and decided to stay on at the University of Turin as a research assistant for histologist and human anatomy professor Guiseppe Levi. Levi-Montalcini started studying nerve cells and nerve fibers – the tiny, slender tendrils that are threaded throughout our nerves and that determine what information each nerve can transmit. But it wasn't long before another enormous obstacle to her scientific career reared its head.
Science Under a Fascist Regime
Two years into her research assistant position, Levi-Montalcini was fired, along with every other "non-Aryan Italian" who held an academic or professional career, thanks to a series of antisemitic laws passed by Italy's then-leader Benito Mussolini. Forced out of her academic position, Levi-Montalcini went to Belgium for a fellowship at a neurological institute in Brussels – but then was forced back to Turin when the German army invaded.
Levi-Montalcini decided to keep researching. She and Guiseppe Levi built a makeshift lab in Levi-Montalcini's apartment, borrowing chicken eggs from local farmers and using sewing needles to dissect them. By dissecting the chicken embryos from her bedroom laboratory, she was able to see how nerve fibers formed and died. The two continued this research until they were interrupted again – this time, by British air raids. Levi-Montalcini fled to a country cottage to continue her research, and then two years later was forced into hiding when the German army invaded Italy. Levi-Montalcini and her family assumed different identities and lived with non-Jewish friends in Florence to survive the Holocaust. Despite all of this, Levi-Montalcini continued her work, dissecting chicken embryos from her hiding place until the end of the war.
"The discovery of NGF really changed the world in which we live, because now we knew that cells talk to other cells, and that they use soluble factors. It was hugely important."
A Post-War Discovery
Several years after the war, when Levi-Montalcini was once again working at the University of Turin, a German embryologist named Viktor Hamburger invited her to Washington University in St. Louis. Hamburger was impressed by Levi-Montalcini's research with her chicken embryos, and secured an opportunity for her to continue her work in America. The invitation would "change the course of my life," Levi-Montalcini would later recall.
During her fellowship, Montalcini grew tumors in mice and then transferred them to chick embryos in order to see how it would affect the chickens. To her surprise, she noticed that introducing the tumor samples would cause nerve fibers to grow rapidly. From this, Levi-Montalcini discovered and was able to isolate a protein that she determined was able to cause this rapid growth. She later named this Nerve Growth Factor, or NGF.
From there, Levi-Montalcini and her team launched new experiments to test NGF, injecting it and repressing it to see the effect it had in a test subject's body. When the team injected NGF into embryonic mice, they observed nerve growth, as well as the mouse pups developing faster – their eyes opening earlier and their teeth coming in sooner – than the untreated group. When the team purified the NGF extract, however, it had no effect, leading the team to believe that something else in the crude extract of NGF was influencing the growth of the newborn mice. Stanley Cohen, Levi-Montalcini's colleague, identified another growth factor called EGF – epidermal growth factor – that caused the mouse pups' eyes and teeth to grow so quickly.
Levi-Montalcini continued to experiment with NGF for the next several decades at Washington University, illuminating how NGF works in our body. When Levi-Montalcini injected newborn mice with an antiserum for NGF, for example, her team found that it "almost completely deprived the animals of a sympathetic nervous system." Other experiments done by Levi-Montalcini and her colleagues helped show the role that NGF plays in other important biological processes, such as the regulation of our immune system and ovulation.
"The discovery of NGF really changed the world in which we live, because now we knew that cells talk to other cells, and that they use soluble factors. It was hugely important," said Bill Mobley, Chair of the Department of Neurosciences at the University of California, San Diego School of Medicine.
Her Lasting Legacy
After years of setbacks, Levi-Montalcini's groundbreaking work was recognized in 1986, when she was awarded the Nobel Prize in Medicine for her discovery of NGF (Cohen, her colleague who discovered EGF, shared the prize). Researchers continue to study NGF even to this day, and the continued research has been able to increase our understanding of diseases like HIV and Alzheimer's.
Levi-Montalcini never stopped researching either: In January 2012, at the age of 102, Levi-Montalcini published her last research paper in the journal PNAS, making her the oldest member of the National Academy of Science to do so. Before she died in December 2012, she encouraged other scientists who would suffer setbacks in their careers to keep pursuing their passions. "Don't fear the difficult moments," Levi-Montalcini is quoted as saying. "The best comes from them."

