Ring vaccination strategy can rein in monkeypox virus, scientists say
Monkeypox produces more telltale signs than COVID-19. Scientists think that a “ring” vaccination strategy can be used when these signs appear to help with squelching the current outbreak of this disease.
A new virus has emerged and stoked fears of another pandemic: monkeypox. Since May 2022, it has been detected in 29 U.S. states, the District of Columbia, and Puerto Rico among international travelers and their close contacts. On a worldwide scale, as of June 30, there have been 5,323 cases in 52 countries.
The good news: An existing vaccine can go a long way toward preventing a catastrophic outbreak. Because monkeypox is a close relative of smallpox, the same vaccine can be used—and it is about 85 percent effective against the virus, according to the World Health Organization (WHO).
Also on the plus side, monkeypox is less contagious with milder illness than smallpox and, compared to COVID-19, produces more telltale signs. Scientists think that a “ring” vaccination strategy can be used when these signs appear to help with squelching this alarming outbreak.
How it’s transmitted
Monkeypox spreads between people primarily through direct contact with infectious sores, scabs, or bodily fluids. People also can catch it through respiratory secretions during prolonged, face-to-face contact, according to the Centers for Disease Control and Prevention (CDC).
As of June 30, there have been 396 documented monkeypox cases in the U.S., and the CDC has activated its Emergency Operations Center to mobilize additional personnel and resources. The U.S. Department of Health and Human Services is aiming to boost testing capacity and accessibility. No Americans have died from monkeypox during this outbreak but, during the COVID-19 pandemic (February 2020 to date), Africa has documented 12,141 cases and 363 deaths from monkeypox.
Ring vaccination proved effective in curbing the smallpox and Ebola outbreaks. As the monkeypox threat continues to loom, scientists view this as the best vaccine approach.
A person infected with monkeypox typically has symptoms—for instance, fever and chills—in a contagious state, so knowing when to avoid close contact with others makes it easier to curtail than COVID-19.
Advantages of ring vaccination
For this reason, it’s feasible to vaccinate a “ring” of people around the infected individual rather than inoculating large swaths of the population. Ring vaccination proved effective in curbing the smallpox and Ebola outbreaks. As the monkeypox threat continues to loom, scientists view this as the best vaccine approach.
With many infections, “it normally would make sense to everyone to vaccinate more widely,” says Wesley C. Van Voorhis, a professor and director of the Center for Emerging and Re-emerging Infectious Diseases at the University of Washington School of Medicine in Seattle. However, “in this case, ring vaccination may be sufficient to contain the outbreak and also minimize the rare, but potentially serious side effects of the smallpox/monkeypox vaccine.”
There are two licensed smallpox vaccines in the United States: ACAM2000 (live Vaccina virus) and JYNNEOS (live virus non-replicating). The ACAM 2000, Van Voorhis says, is the old smallpox vaccine that, in rare instances, could spread diffusely within the body and cause heart problems, as well as severe rash in people with eczema or serious infection in immunocompromised patients.
To prevent organ damage, the current recommendation would be to use the JYNNEOS vaccine, says Phyllis Kanki, a professor of health sciences in the division of immunology and infectious diseases at the Harvard T.H. Chan School of Public Health. However, according to a report on the CDC’s website, people with immunocompromising conditions could have a higher risk of getting a severe case of monkeypox, despite being vaccinated, and “might be less likely to mount an effective response after any vaccination, including after JYNNEOS.”
In the late 1960s, the ring vaccination strategy became part of the WHO’s mission to globally eradicate smallpox, with the last known natural case described in Somalia in 1977. Ring vaccination can also refer to how a clinical trial is designed, as was the case in 2015, when this approach was used for researching the benefits of an investigational Ebola vaccine in Guinea, Kanki says.
“Since Monkeypox spreads by close contact and we have an effective vaccine, vaccinating high-risk individuals and their contacts may be a good strategy to limit transmission,” she says, adding that privacy is an important ethical principle that comes into play, as people with monkeypox would need to disclose their close contacts so that they could benefit from ring vaccination.
Rapid identification of cases and contacts—along with their cooperation—is essential for ring vaccination to be effective. Although mass vaccination also may work, the risk of infection to most of the population remains low while supply of the JYNNEOS vaccine is limited, says Stanley Deresinski, a clinical professor of medicine in the Infectious Disease Clinic at Stanford University School of Medicine.
Other strategies for preventing transmission
Ideally, the vaccine should be administered within four days of an exposure, but it’s recommended for up to 14 days. The WHO also advocates more widespread vaccination campaigns in the population segment with the most cases so far: men who engage in sex with other men.
The virus appears to be spreading in sexual networks, which differs from what was seen in previously reported outbreaks of monkeypox (outside of Africa), where risk was associated with travel to central or west Africa or various types of contact with individuals or animals from those locales. There is no evidence of transmission by food, but contaminated articles in the environment such as bedding are potential sources of the virus, Deresinski says.
Severe cases of monkeypox can occur, but “transmission of the virus requires close contact,” he says. “There is no evidence of aerosol transmission, as occurs with SARS-CoV-2, although it must be remembered that the smallpox virus, a close relative of monkeypox, was transmitted by aerosol.”
Deresinski points to the fact that in 2003, monkeypox was introduced into the U.S. through imports from Ghana of infected small mammals, such as Gambian giant rats, as pets. They infected prairie dogs, which also were sold as pets and, ultimately, this resulted in 37 confirmed transmissions to humans and 10 probable cases. A CDC investigation identified no cases of human-to-human transmission. Then, in 2021, a traveler flew from Nigeria to Dallas through Atlanta, developing skin lesions several days after arrival. Another CDC investigation yielded 223 contacts, although 85 percent were deemed to be at only minimal risk and the remainder at intermediate risk. No new cases were identified.
How much should we be worried
But how serious of a threat is monkeypox this time around? “Right now, the risk to the general public is very low,” says Scott Roberts, an assistant professor and associate medical director of infection prevention at Yale School of Medicine. “Monkeypox is spread through direct contact with infected skin lesions or through close contact for a prolonged period of time with an infected person. It is much less transmissible than COVID-19.”
The monkeypox incubation period—the time from infection until the onset of symptoms—is typically seven to 14 days but can range from five to 21 days, compared with only three days for the Omicron variant of COVID-19. With such a long incubation, there is a larger window to conduct contact tracing and vaccinate people before symptoms appear, which can prevent infection or lessen the severity.
But symptoms may present atypically or recognition may be delayed. “Ring vaccination works best with 100 percent adherence, and in the absence of a mandate, this is not achievable,” Roberts says.
At the outset of infection, symptoms include fever, chills, and fatigue. Several days later, a rash becomes noticeable, usually beginning on the face and spreading to other parts of the body, he says. The rash starts as flat lesions that raise and develop fluid, similar to manifestations of chickenpox. Once the rash scabs and falls off, a person is no longer contagious.
“It's an uncomfortable infection,” says Van Voorhis, the University of Washington School of Medicine professor. There may be swollen lymph nodes. Sores and rash are often limited to the genitals and areas around the mouth or rectum, suggesting intimate contact as the source of spread.
Symptoms of monkeypox usually last from two to four weeks. The WHO estimated that fatalities range from 3 to 6 percent. Although it’s believed to infect various animal species, including rodents and monkeys in west and central Africa, “the animal reservoir for the virus is unknown,” says Kanki, the Harvard T.H. Chan School of Public Health professor.
Too often, viruses originate in parts of the world that are too poor to grapple with them and may lack the resources to invest in vaccines and treatments. “This disease is endemic in central and west Africa, and it has basically been ignored until it jumped to the north and infected Europeans, Americans, and Canadians,” Van Voorhis says. “We have to do a better job in health care and prevention all over the world. This is the kind of thing that comes back to bite us.”
In this week's Friday Five, new research that could help prevent Alzheimer's. Plus, why you should care about smart senior towns, how to reverse being drunk, money can make you happier if you're this type of person, and personalized anxiety medicine.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Here are the promising studies covered in this week's Friday Five, featuring interviews with Dr. Christopher Martens, director of the Delaware Center for Cogntiive Aging Research and professor of kinesiology and applied physiology at the University of Delaware, and Dr. Ilona Matysiak, visiting scholar at Iowa State University and associate professor of sociology at Maria Grzegorzewska University.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
- Could this supplement help prevent Alzheimer's?
- Why you should care about smart senior towns
- Here's how to reverse being drunk
- Money can make you happy - if you're this type of person
- Personalized anxiety medicine
As gene therapies and small molecule drugs are being studied in clinical trials, companies increasingly see the value in hiring patients to help explain the potential benefits.
As a child, Wendy Borsari participated in a health study at Boston Children’s Hospital. She was involved because heart disease and sudden cardiac arrest ran in her family as far back as seven generations. When she was 18, however, the study’s doctors told her that she had a perfectly healthy heart and didn’t have to worry.
A couple of years after graduating from college, though, the Boston native began to experience episodes of near fainting. During any sort of strenuous exercise, my blood pressure would drop instead of increasing, she recalls.
She was diagnosed at 24 with hypertrophic cardiomyopathy. Although HCM is a commonly inherited heart disease, Borsari’s case resulted from a rare gene mutation, the MYH7 gene. Her mother had been diagnosed at 27, and Borsari had already lost her grandmother and two maternal uncles to the condition. After her own diagnosis, Borsari spent most of her free time researching the disease and “figuring out how to have this condition and still be the person I wanted to be,” she says.
Then, her son was found to have the genetic mutation at birth and diagnosed with HCM at 15. Her daughter, also diagnosed at birth, later suffered five cardiac arrests.
That changed Borsari’s perspective. She decided to become a patient advocate. “I didn’t want to just be a patient with the condition,” she says. “I wanted to be more involved with the science and the biopharmaceutical industry so I could be active in helping to make it better for other patients.”
She consulted on patient advocacy for a pharmaceutical and two foundations before coming to a company called Tenaya in 2021.
“One of our core values as a company is putting patients first,” says Tenaya's CEO, Faraz Ali. “We thought of no better way to put our money where our mouth is than by bringing in somebody who is affected and whose family is affected by a genetic form of cardiomyopathy to have them make sure we’re incorporating the voice of the patient.”
Biomedical corporations and government research agencies are now incorporating patient advocacy more than ever, says Alice Lara, president and CEO of the Sudden Arrhythmia Death Syndromes Foundation in Salt Lake City, Utah. These organizations have seen the effectiveness of including patient voices to communicate and exemplify the benefits that key academic research institutions have shown in their medical studies.
“From our side of the aisle,” Lara says, “what we know as patient advocacy organizations is that educated patients do a lot better. They have a better course in their therapy and their condition, and understanding the genetics is important because all of our conditions are genetic.”
Founded in 2016, Tenaya is advancing gene therapies and small molecule drugs in clinical trials for both prevalent and rare forms of heart disease, says Ali, the CEO.
The firm's first small molecule, now in a Phase 1 clinical trial, is intended to treat heart failure with preserved ejection fraction, where the amount of blood pumped by the heart is reduced due to the heart chambers becoming weak or stiff. The condition accounts for half or more of all heart failure in the U.S., according to Ali, and is growing quickly because it's closely associated with diabetes. It’s also linked with metabolic syndrome, or a cluster of conditions including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
“We have a novel molecule that is first in class and, to our knowledge, best in class to tackle that, so we’re very excited about the clinical trial,” Ali says.
The first phase of the trial is being performed with healthy participants, rather than people with the disease, to establish safety and tolerability. The researchers can also look for the drug in blood samples, which could tell them whether it's reaching its target. Ali estimates that, if the company can establish safety and that it engages the right parts of the body, it will likely begin dosing patients with the disease in 2024.
Tenaya’s therapy delivers a healthy copy of the gene so that it makes a copy of the protein missing from the patients' hearts because of their mutation. The study will start with adult patients, then pivot potentially to children and even newborns, Ali says, “where there is an even greater unmet need because the disease progresses so fast that they have no options.”
Although this work still has a long way to go, Ali is excited about the potential because the gene therapy achieved positive results in the preclinical mouse trial. This animal trial demonstrated that the treatment reduced enlarged hearts, reversed electrophysiological abnormalities, and improved the functioning of the heart by increasing the ejection fraction after the single-dose of gene therapy. That measurement remained stable to the end of the animals’ lives, roughly 18 months, Ali says.
He’s also energized by the fact that heart disease has “taken a page out of the oncology playbook” by leveraging genetic research to develop more precise and targeted drugs and gene therapies.
“Now we are talking about a potential cure of a disease for which there was no cure and using a very novel concept,” says Melind Desai of the Cleveland Clinic.
Tenaya’s second program focuses on developing a gene therapy to mitigate the leading cause of hypertrophic cardiomyopathy through a specific gene called MYPBC3. The disease affects approximately 600,000 patients in the U.S. This particular genetic form, Ali explains, affects about 115,000 in the U.S. alone, so it is considered a rare disease.
“There are infants who are dying within the first weeks to months of life as a result of this mutation,” he says. “There are also adults who start having symptoms in their 20s, 30s and 40s with early morbidity and mortality.” Tenaya plans to apply before the end of this year to get the FDA’s approval to administer an investigational drug for this disease humans. If approved, the company will begin to dose patients in 2023.
“We now understand the genetics of the heart much better,” he says. “We now understand the leading genetic causes of hypertrophic myopathy, dilated cardiomyopathy and others, so that gives us the ability to take these large populations and stratify them rationally into subpopulations.”
Melind Desai, MD, who directs Cleveland Clinic’s Hypertrophic Cardiomyopathy Center, says that the goal of Tenaya’s second clinical study is to help improve the basic cardiac structure in patients with hypertrophic cardiomyopathy related to the MYPBC3 mutation.
“Now we are talking about a potential cure of a disease for which there was no cure and using a very novel concept,” he says. “So this is an exciting new frontier of therapeutic investigation for MYPBC3 gene-positive patients with a chance for a cure.
Neither of Tenaya’s two therapies address the gene mutation that has affected Borsari and her family. But Ali sees opportunity down the road to develop a gene therapy for her particular gene mutation, since it is the second leading cause of cardiomyopathy. Treating the MYH7 gene is especially challenging because it requires gene editing or silencing, instead of just replacing the gene.
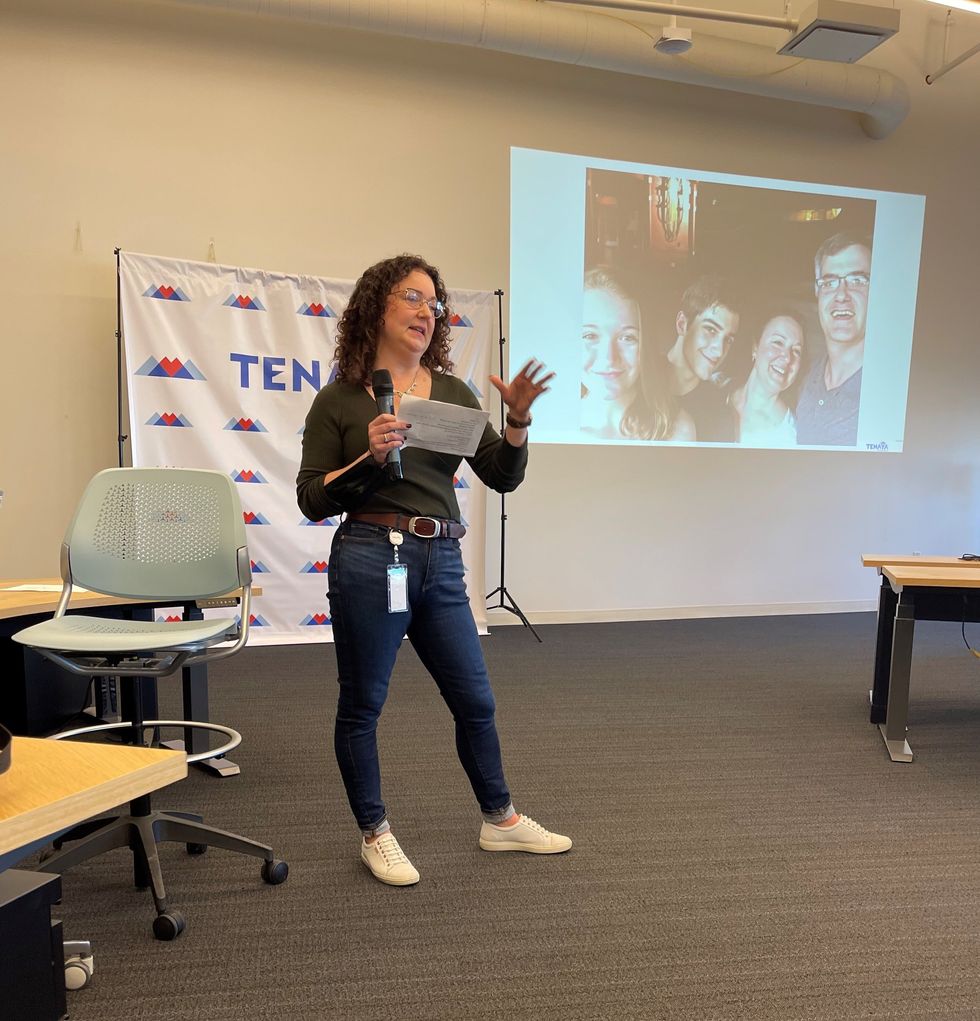
Wendy Borsari was diagnosed at age 24 with a commonly inherited heart disease. She joined Tenaya as a patient advocate in 2021.
Wendy Borsari
“If you add a healthy gene it will produce healthy copies,” Ali explains, “but it won’t stop the bad effects of the mutant protein the gene produces. You can only do that by silencing the gene or editing it out, which is a different, more complicated approach.”
Euan Ashley, professor of medicine and genetics at Stanford University and founding director of its Center for Inherited Cardiovascular Disease, is confident that we will see genetic therapies for heart disease within the next decade.
“We are at this really exciting moment in time where we have diseases that have been under-recognized and undervalued now being attacked by multiple companies with really modern tools,” says Ashley, author of The Genome Odyssey. “Gene therapies are unusual in the sense that they can reverse the cause of the disease, so we have the enticing possibility of actually reversing or maybe even curing these diseases.”
Although no one is doing extensive research into a gene therapy for her particular mutation yet, Borsari remains hopeful, knowing that companies such as Tenaya are moving in that direction.
“I know that’s now on the horizon,” she says. “It’s not just some pipe dream, but will happen hopefully in my lifetime or my kids’ lifetime to help them.”

