More Families Are Using Nanny Cams to Watch Elderly Loved Ones, Raising Ethical Questions

Jackie Costanzo and her 93-year-old mom, Louise, are happy to have an extra way to stay connected with the camera, which is normally placed on a television stand facing her mom's bed.
After Jackie Costanzo's mother broke her right hip in a fall, she needed more hands-on care in her assisted-living apartment near Sacramento, California. A social worker from her health plan suggested installing a video camera to help ensure those services were provided.
Without the camera, Costanzo wouldn't have a way to confirm that caregivers had followed through with serving meals, changing clothes, and fulfilling other care needs.
When Costanzo placed the device in May 2018, she informed the administrator and staff, and at first, there were no objections. The facility posted a sign on the apartment's front door, alerting anyone who entered of recording in progress.
But this past spring, a new management company came across the sign and threatened to issue a 30-day eviction notice to her 93-year-old mother, Louise Munch, who has dementia, for violating a policy that prohibits cameras in residents' rooms. With encouragement from California Advocates for Nursing Home Reform, Costanzo researched the state's regulations but couldn't find anything to support or deny camera use. She refused to remove the recording device and prevailed.
"In essence, my mom was 'grandfathered in' because she moved in under a management company that did not specify that residents could not have cameras," says Costanzo, 73, a retired elementary schoolteacher who lives a three-hour drive away, in Silicon Valley, and visits one day every two weeks. Without the camera, Costanzo, who is her mother's only surviving child, wouldn't have a way to confirm that caregivers had followed through with serving meals, changing clothes, and fulfilling other care needs.
As technological innovations enable next of kin to remain apprised of the elderly's daily care in long-term care facilities, surveillance cameras bring legal and privacy issues to the forefront of a complex ethical debate. Families place them overtly or covertly—disguised in a makeshift clock radio, for instance—when they suspect or fear abuse or neglect, so they can maintain a watchful eye, perhaps deterring egregious behavior. But the cameras also capture intimate caregiving tasks, such as bathing and toileting, as well as dressing and undressing, which may undermine the dignity of residents.
So far, laws or guidelines in eight states—Illinois, Maryland, New Mexico, Oklahoma, Texas, Utah, Virginia, and Washington—have granted families the rights to install cameras in a resident's room. In addition, about 15 other states have proposed legislation. Some states, such as Pennsylvania, have put forth regulatory compliance guidance, according to a column published in the July/August 2018 issue of Annals of Long-Term Care.
The increasing prevalence of this legislation has placed it on the radar of long-term care providers. It also suggests a trend to clarify responsible camera use in monitoring services while respecting privacy, says Victor Lane Rose, the column's editor and director of aging services at ECRI Institute, a health care nonprofit near Philadelphia, Pennsylvania.
In most cases, a resident's family installs a camera or instigates a request in hopes of sparing their loved one from the harms of abuse, says James Wright, a family physician who serves as the ethics committee's vice chair of the Society for Post-Acute and Long-Term Care Medicine in Columbia, Maryland. A camera also allows the family to check in on the resident from afar and remain on alert for a potential fall or agitated state, he says.
"It's rare that a facility will have 24-hour presence in a patient's room. You won't have a nurse in there all the time," says Wright, who is also medical director of two long-term care centers and one assisted-living facility around Richmond, Virginia. Particularly "with dementia, the family often wonders" if their loved one is safe.
While offering families peace of mind, he notes that video cameras can also help exonerate caregivers accused of abuse or theft. Hearing aids, which typically cost between $2,000 and $3,000 each, often go missing. By reviewing a video together, families and administrators may find clues to a device's disappearance. Conversely, Wright empathizes with the main counterargument against camera use, which is the belief that "invasion of privacy is also invasion of human dignity."
In respecting modesty, ethical questions abound over whether a camera should be turned off when a patient is in the midst of receiving personal care, such as dressing and undressing or using bedpans. Other ethical issues revolve around who may access the recordings, says Lori Smetanka, executive director of the National Consumer Voice for Quality Long-Term Care in Washington, D.C.
Video cameras, she contends, are only one tool in shielding residents from abuse. They are "not substitutes for personal involvement," she says. "People need to be very vigilant visiting their family members, and facilities have a responsibility to ensure that residents are free of abuse."
Lack of accountability perpetuates abuse in long-term care settings and stems in large part from systemic underfunding.
Educating employees in abuse prevention becomes paramount, and families should ask about staff training before placing their loved one in a long-term care facility, Smetanka says. Prior to installing a camera, she recommends consulting an attorney who is familiar with this issue.
But thoughts of a camera often don't occur to families until an adverse event affects their loved one, says Toby Edelman, a senior policy attorney at the Center for Medicare Advocacy, a nonprofit organization with headquarters in Washington, D.C., and Connecticut.
"These cameras can show exactly what's going on," she explains, noting that prosecutors have used the recordings in litigation. "When residents have injuries of unknown origin" and they can't verbalize what happened to them, "the cameras may document that yes, the resident was actually hit by somebody."
With a resident's safety and security being "the most important consideration," the American Health Care Association in Washington, D.C., which represents long-term and post-acute care providers, supports allowing states, clinicians, and patients to decide about camera use on a local level, says David Gifford, senior vice president of quality and regulatory affairs and chief medical officer.
"We've seen some success with tools such as permissive legislation, where residents and their loved ones have the ability to determine whether a camera is right for them while working with the center openly and ensuring the confidentiality of other residents," says Gifford, who practiced as a geriatrician. "It is important to note, however, that surveillance cameras are still only one element of the quality matrix. We can never hope to truly improve quality care by catching bad actors after the fact."
Lack of accountability perpetuates abuse in long-term care settings and stems in large part from systemic underfunding. Low wages and morale are tied to high turnover, and cameras don't address this overarching problem, says Clara Berridge, an assistant professor of social work at the University of Washington in Seattle, who has co-authored articles on surveillance devices in elder care.
Employees often don't perceive a nursing assistant position as a long-term career trajectory and may not feel vested in the workplace. Training in the recognition and reporting of abuse becomes ineffective when workers quit shortly thereafter. Many must juggle multiple jobs to make ends meet. Staffing shortages are endemic, leading to inadequate oversight of residents and voicing of abuse complaints, she says.
In Berridge's assessment, cameras may do more harm than good. Respondents to a survey she conducted of nursing homes and assisted-living facilities in the United States found that recording devices tend to fuel workers' anxiety amid a culture that further demoralizes and dehumanizes the care they provide.
Consent becomes particularly thorny in shared rooms, which are more common than not in nursing homes. States that permit in-room cameras mandate that roommates or their legal representative be made aware. Even if the camera is directed away from their bed, it will still capture conversations as well as movements that enter its scope. "Surveillance isn't the best way to protect adults in need of support," Berridge says. "Public investment in quality care is."
"The camera is invaluable. But there's no law that says you can have it automatically, so that's wrong."
In the one-bedroom assisted-living apartment where Costanzo's mother lives alone, consent from another resident wasn't needed. Without a roommate, the camera is much less intrusive, although Costanzo wishes she had put one in the living room, not just the bedroom, for more security.
Her safety concerns escalated when she read about a Texas serial killer who smothered victims after gaining access to senior care facilities by "masquerading as a maintenance man." She points to such horrifying incidents, although exceedingly rare, as further justification for permitting cameras to help guard the vulnerable against abuse in long-term care settings. And she hopes to advocate for an applicable law in California.
"The camera is invaluable," says Costanzo, who pays for monthly Wi-Fi service so she can see and interact with her mother, who turns 94 in October, any time of day or night. "But there's no law that says you can have it automatically, so that's wrong."
Scientists have known about and studied heart rate variability, or HRV, for a long time and, in recent years, monitors have come to market that can measure HRV accurately.
This episode is about a health metric you may not have heard of before: heart rate variability, or HRV. This refers to the small changes in the length of time between each of your heart beats.
Scientists have known about and studied HRV for a long time. In recent years, though, new monitors have come to market that can measure HRV accurately whenever you want.
Five months ago, I got interested in HRV as a more scientific approach to finding the lifestyle changes that work best for me as an individual. It's at the convergence of some important trends in health right now, such as health tech, precision health and the holistic approach in systems biology, which recognizes how interactions among different parts of the body are key to health.
But HRV is just one of many numbers worth paying attention to. For this episode of Making Sense of Science, I spoke with psychologist Dr. Leah Lagos; Dr. Jessilyn Dunn, assistant professor in biomedical engineering at Duke; and Jason Moore, the CEO of Spren and an app called Elite HRV. We talked about what HRV is, research on its benefits, how to measure it, whether it can be used to make improvements in health, and what researchers still need to learn about HRV.
*Talk to your doctor before trying anything discussed in this episode related to HRV and lifestyle changes to raise it.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Show notes
Spren - https://www.spren.com/
Elite HRV - https://elitehrv.com/
Jason Moore's Twitter - https://twitter.com/jasonmooreme?lang=en
Dr. Jessilyn Dunn's Twitter - https://twitter.com/drjessilyn?lang=en
Dr. Dunn's study on HRV, flu and common cold - https://jamanetwork.com/journals/jamanetworkopen/f...
Dr. Leah Lagos - https://drleahlagos.com/
Dr. Lagos on Star Talk - https://www.youtube.com/watch?v=jC2Q10SonV8
Research on HRV and intermittent fasting - https://pubmed.ncbi.nlm.nih.gov/33859841/
Research on HRV and Mediterranean diet - https://medicalxpress.com/news/2010-06-twin-medite...:~:text=Using%20data%20from%20the%20Emory,eating%20a%20Western%2Dtype%20diet
Devices for HRV biofeedback - https://elitehrv.com/heart-variability-monitors-an...
Benefits of HRV biofeedback - https://pubmed.ncbi.nlm.nih.gov/32385728/
HRV and cognitive performance - https://www.frontiersin.org/articles/10.3389/fnins...
HRV and emotional regulation - https://pubmed.ncbi.nlm.nih.gov/36030986/
Fortune article on HRV - https://fortune.com/well/2022/12/26/heart-rate-var...
Peanut allergies affect about a million children in the U.S., and most never outgrow them. Luckily, some promising remedies are in the works.
Ever since he was a baby, Sharon Wong’s son Brandon suffered from rashes, prolonged respiratory issues and vomiting. In 2006, as a young child, he was diagnosed with a severe peanut allergy.
"My son had a history of reacting to traces of peanuts in the air or in food,” says Wong, a food allergy advocate who runs a blog focusing on nut free recipes, cooking techniques and food allergy awareness. “Any participation in school activities, social events, or travel with his peanut allergy required a lot of preparation.”
Peanut allergies affect around a million children in the U.S. Most never outgrow the condition. The problem occurs when the immune system mistakenly views the proteins in peanuts as a threat and releases chemicals to counteract it. This can lead to digestive problems, hives and shortness of breath. For some, like Wong’s son, even exposure to trace amounts of peanuts could be life threatening. They go into anaphylactic shock and need to take a shot of adrenaline as soon as possible.
Typically, people with peanut allergies try to completely avoid them and carry an adrenaline autoinjector like an EpiPen in case of emergencies. This constant vigilance is very stressful, particularly for parents with young children.
“The search for a peanut allergy ‘cure’ has been a vigorous one,” says Claudia Gray, a pediatrician and allergist at Vincent Pallotti Hospital in Cape Town, South Africa. The closest thing to a solution so far, she says, is the process of desensitization, which exposes the patient to gradually increasing doses of peanut allergen to build up a tolerance. The most common type of desensitization is oral immunotherapy, where patients ingest small quantities of peanut powder. It has been effective but there is a risk of anaphylaxis since it involves swallowing the allergen.
"By the end of the trial, my son tolerated approximately 1.5 peanuts," Sharon Wong says.
DBV Technologies, a company based in Montrouge, France has created a skin patch to address this problem. The Viaskin Patch contains a much lower amount of peanut allergen than oral immunotherapy and delivers it through the skin to slowly increase tolerance. This decreases the risk of anaphylaxis.
Wong heard about the peanut patch and wanted her son to take part in an early phase 2 trial for 4-to-11-year-olds.
“We felt that participating in DBV’s peanut patch trial would give him the best chance at desensitization or at least increase his tolerance from a speck of peanut to a peanut,” Wong says. “The daily routine was quite simple, remove the old patch and then apply a new one. By the end of the trial, he tolerated approximately 1.5 peanuts.”
How it works
For DBV Technologies, it all began when pediatric gastroenterologist Pierre-Henri Benhamou teamed up with fellow professor of gastroenterology Christopher Dupont and his brother, engineer Bertrand Dupont. Together they created a more effective skin patch to detect when babies have allergies to cow's milk. Then they realized that the patch could actually be used to treat allergies by promoting tolerance. They decided to focus on peanut allergies first as the more dangerous.
The Viaskin patch utilizes the fact that the skin can promote tolerance to external stimuli. The skin is the body’s first defense. Controlling the extent of the immune response is crucial for the skin. So it has defense mechanisms against external stimuli and can promote tolerance.
The patch consists of an adhesive foam ring with a plastic film on top. A small amount of peanut protein is placed in the center. The adhesive ring is attached to the back of the patient's body. The peanut protein sits above the skin but does not directly touch it. As the patient sweats, water droplets on the inside of the film dissolve the peanut protein, which is then absorbed into the skin.
The peanut protein is then captured by skin cells called Langerhans cells. They play an important role in getting the immune system to tolerate certain external stimuli. Langerhans cells take the peanut protein to lymph nodes which activate T regulatory cells. T regulatory cells suppress the allergic response.
A different patch is applied to the skin every day to increase tolerance. It’s both easy to use and convenient.
“The DBV approach uses much smaller amounts than oral immunotherapy and works through the skin significantly reducing the risk of allergic reactions,” says Edwin H. Kim, the division chief of Pediatric Allergy and Immunology at the University of North Carolina, U.S., and one of the principal investigators of Viaskin’s clinical trials. “By not going through the mouth, the patch also avoids the taste and texture issues. Finally, the ability to apply a patch and immediately go about your day may be very attractive to very busy patients and families.”
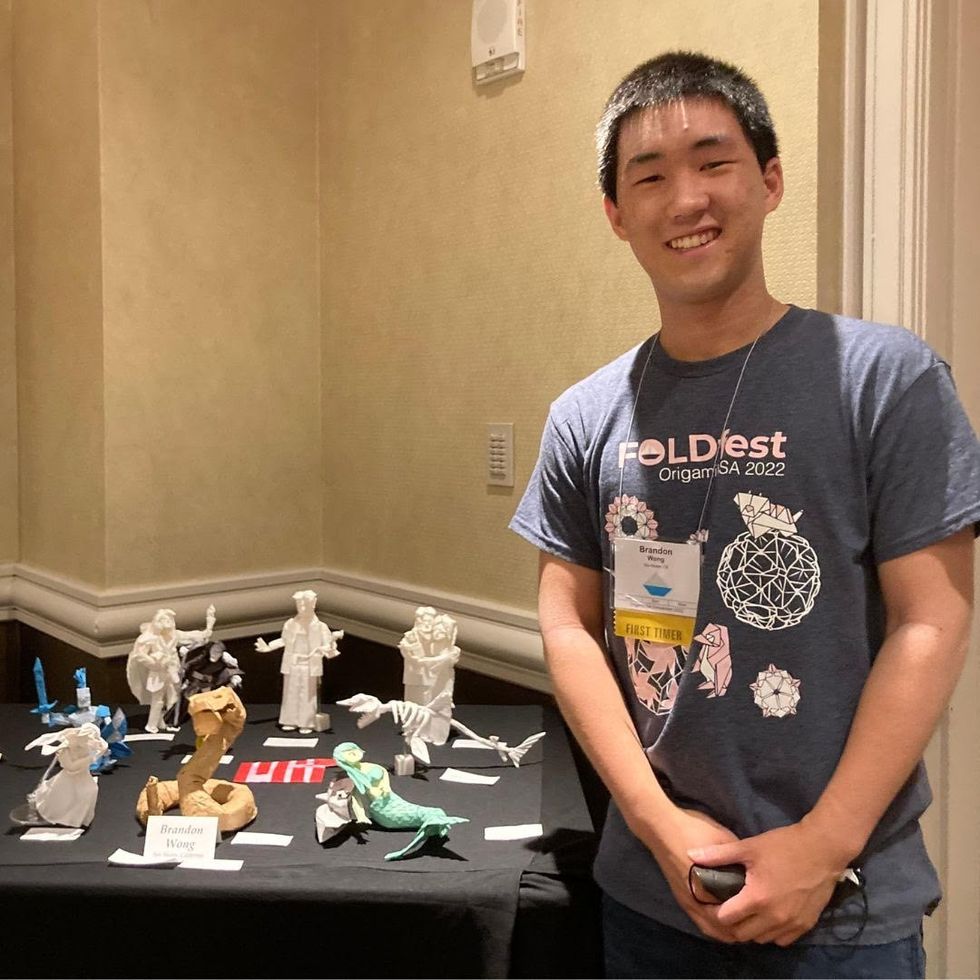
Brandon Wong displaying origami figures he folded at an Origami Convention in 2022
Sharon Wong
Clinical trials
Results from DBV's phase 3 trial in children ages 1 to 3 show its potential. For a positive result, patients who could not tolerate 10 milligrams or less of peanut protein had to be able to manage 300 mg or more after 12 months. Toddlers who could already tolerate more than 10 mg needed to be able to manage 1000 mg or more. In the end, 67 percent of subjects using the Viaskin patch met the target as compared to 33 percent of patients taking the placebo dose.
“The Viaskin peanut patch has been studied in several clinical trials to date with promising results,” says Suzanne M. Barshow, assistant professor of medicine in allergy and asthma research at Stanford University School of Medicine in the U.S. “The data shows that it is safe and well-tolerated. Compared to oral immunotherapy, treatment with the patch results in fewer side effects but appears to be less effective in achieving desensitization.”
The primary reason the patch is less potent is that oral immunotherapy uses a larger amount of the allergen. Additionally, absorption of the peanut protein into the skin could be erratic.
Gray also highlights that there is some tradeoff between risk and efficacy.
“The peanut patch is an exciting advance but not as effective as the oral route,” Gray says. “For those patients who are very sensitive to orally ingested peanut in oral immunotherapy or have an aversion to oral peanut, it has a use. So, essentially, the form of immunotherapy will have to be tailored to each patient.” Having different forms such as the Viaskin patch which is applied to the skin or pills that patients can swallow or dissolve under the tongue is helpful.
The hope is that the patch’s efficacy will increase over time. The team is currently running a follow-up trial, where the same patients continue using the patch.
“It is a very important study to show whether the benefit achieved after 12 months on the patch stays stable or hopefully continues to grow with longer duration,” says Kim, who is an investigator in this follow-up trial.
"My son now attends university in Massachusetts, lives on-campus, and eats dorm food. He has so much more freedom," Wong says.
The team is further ahead in the phase 3 follow-up trial for 4-to-11-year-olds. The initial phase 3 trial was not as successful as the trial for kids between one and three. The patch enabled patients to tolerate more peanuts but there was not a significant enough difference compared to the placebo group to be definitive. The follow-up trial showed greater potency. It suggests that the longer patients are on the patch, the stronger its effects.
They’re also testing if making the patch bigger, changing the shape and extending the minimum time it’s worn can improve its benefits in a trial for a new group of 4-to-11 year-olds.
The future
DBV Technologies is using the skin patch to treat cow’s milk allergies in children ages 1 to 17. They’re currently in phase 2 trials.
As for the peanut allergy trials in toddlers, the hope is to see more efficacy soon.
For Wong’s son who took part in the earlier phase 2 trial for 4-to-11-year-olds, the patch has transformed his life.
“My son continues to maintain his peanut tolerance and is not affected by peanut dust in the air or cross-contact,” Wong says. ”He attends university in Massachusetts, lives on-campus, and eats dorm food. He still carries an EpiPen but has so much more freedom than before his clinical trial. We will always be grateful.”

