Fungus is the ‘New Black’ in Eco-Friendly Fashion

On the left, a Hermès bag made using fine mycelium as a leather alternative, made in partnership with the biotech company MycoWorks; on right, a sheet of mycelium "leather."
A natural material that looks and feels like real leather is taking the fashion world by storm. Scientists view mycelium—the vegetative part of a mushroom-producing fungus—as a planet-friendly alternative to animal hides and plastics.
Products crafted from this vegan leather are emerging, with others poised to hit the market soon. Among them are the Hermès Victoria bag, Lululemon's yoga accessories, Adidas' Stan Smith Mylo sneaker, and a Stella McCartney apparel collection.

The Adidas' Stan Smith Mylo concept sneaker, made in partnership with Bolt Threads, uses an alternative leather grown from mycelium; a commercial version is expected in the near future.
Adidas
Hermès has held presales on the new bag, says Philip Ross, co-founder and chief technology officer of MycoWorks, a San Francisco Bay area firm whose materials constituted the design. By year-end, Ross expects several more clients to debut mycelium-based merchandise. With "comparable qualities to luxury leather," mycelium can be molded to engineer "all the different verticals within fashion," he says, particularly footwear and accessories.
More than a half-dozen trailblazers are fine-tuning mycelium to create next-generation leather materials, according to the Material Innovation Initiative, a nonprofit advocating for animal-free materials in the fashion, automotive, and home-goods industries. These high-performance products can supersede items derived from leather, silk, down, fur, wool, and exotic skins, says A. Sydney Gladman, the institute's chief scientific officer.
That's only the beginning of mycelium's untapped prowess. "We expect to see an uptick in commercial leather alternative applications for mycelium-based materials as companies refine their R&D [research and development] and scale up," Gladman says, adding that "technological innovation and untapped natural materials have the potential to transform the materials industry and solve the enormous environmental challenges it faces."
In fewer than 10 days in indoor agricultural farms, "we grow large slabs of mycelium that are many feet wide and long. We are not confined to the shape or geometry of an animal."
Reducing our carbon footprint becomes possible because mycelium can flourish in indoor farms, using agricultural waste as feedstock and emitting inherently low greenhouse gas emissions. Carbon dioxide is the primary greenhouse gas. "We often think that when plant tissues like wood rot, that they go from something to nothing," says Jonathan Schilling, professor of plant and microbial biology at the University of Minnesota and a member of MycoWorks' Scientific Advisory Board.
But that assumption doesn't hold true for all carbon in plant tissues. When the fungi dominating the decomposition of plants fulfill their function, they transform a large portion of carbon into fungal biomass, Schilling says. That, in turn, ends up in the soil, with mycelium forming a network underneath that traps the carbon.
Unlike the large amounts of fossil fuels needed to produce styrofoam, leather and plastic, less fuel-intensive processing is involved in creating similar materials with a fungal organism. While some fungi consist of a single cell, others are multicellular and develop as very fine threadlike structures. A mass of them collectively forms a "mycelium" that can be either loose and low density or tightly packed and high density. "When these fungi grow at extremely high density," Schilling explains, "they can take on the feel of a solid material such as styrofoam, leather or even plastic."
Tunable and supple in the cultivation process, mycelium is also reliably sturdy in composition. "We believe that mycelium has some unique attributes that differentiate it from plastic-based and animal-derived products," says Gavin McIntyre, who co-founded Ecovative Design, an upstate New York-based biomaterials company, in 2007 with the goal of displacing some environmentally burdensome materials and making "a meaningful impact on our planet."
After inventing a type of mushroom-based packaging for all sorts of goods, in 2013 the firm ventured into manufacturing mycelium that can be adapted for textiles, he says, because mushrooms are "nature's recycling system."
The company aims for its material—which is "so tough and tenacious" that it doesn't require any plastic add-on as reinforcement—to be generally accessible from a pricing standpoint and not confined to a luxury space. The cost, McIntyre says, would approach that of bovine leather, not the more upscale varieties of lamb and goat skins.
Already, production has taken off by leaps and bounds. In fewer than 10 days in indoor agricultural farms, "we grow large slabs of mycelium that are many feet wide and long," he says. "We are not confined to the shape or geometry of an animal," so there's a much lower scrap rate.
Decreasing the scrap rate is a major selling point. "Our customers can order the pieces to the way that they want them, and there is almost no waste in the processing," explains Ross of MycoWorks. "We can make ours thinner or thicker," depending on a client's specific needs. Growing materials locally also results in a reduction in transportation, shipping, and other supply chain costs, he says.
Yet another advantage to making things out of mycelium is its biodegradability at the end of an item's lifecycle. When a pair of old sneakers lands in a compost pile or landfill, it decomposes thanks to microbial processes that, once again, involve fungi. "It is cool to think that the same organism used to create a product can also be what recycles it, perhaps building something else useful in the same act," says biologist Schilling. That amounts to "more than a nice business model—it is a window into how sustainability works in nature."
A product can be called "sustainable" if it's biodegradable, leaves a minimal carbon footprint during production, and is also profitable, says Preeti Arya, an assistant professor at the Fashion Institute of Technology in New York City and faculty adviser to a student club of the American Association of Textile Chemists and Colorists.
On the opposite end of the spectrum, products composed of petroleum-based polymers don't biodegrade—they break down into smaller pieces or even particles. These remnants pollute landfills, oceans, and rivers, contaminating edible fish and eventually contributing to the growth of benign and cancerous tumors in humans, Arya says.
Commending the steps a few designers have taken toward bringing more environmentally conscious merchandise to consumers, she says, "I'm glad that they took the initiative because others also will try to be part of this competition toward sustainability." And consumers will take notice. "The more people become aware, the more these brands will start acting on it."
A further shift toward mycelium-based products has the capability to reap tremendous environmental dividends, says Drew Endy, associate chair of bioengineering at Stanford University and president of the BioBricks Foundation, which focuses on biotechnology in the public interest.
The continued development of "leather surrogates on a scaled and sustainable basis will provide the greatest benefit to the greatest number of people, in perpetuity," Endy says. "Transitioning the production of leather goods from a process that involves the industrial-scale slaughter of vertebrate mammals to a process that instead uses renewable fungal-based manufacturing will be more just."
7 Reasons Why We Should Not Need Boosters for COVID-19
A top infectious disease physician explains why immunity derived from natural infection and the vaccines should be long-lasting.
There are at least 7 reasons why immunity after vaccination or infection with COVID-19 should likely be long-lived. If durable, I do not think boosters will be necessary in the future, despite CEOs of pharmaceutical companies (who stand to profit from boosters) messaging that they may and readying such boosters. To explain these reasons, let's orient ourselves to the main components of the immune system.
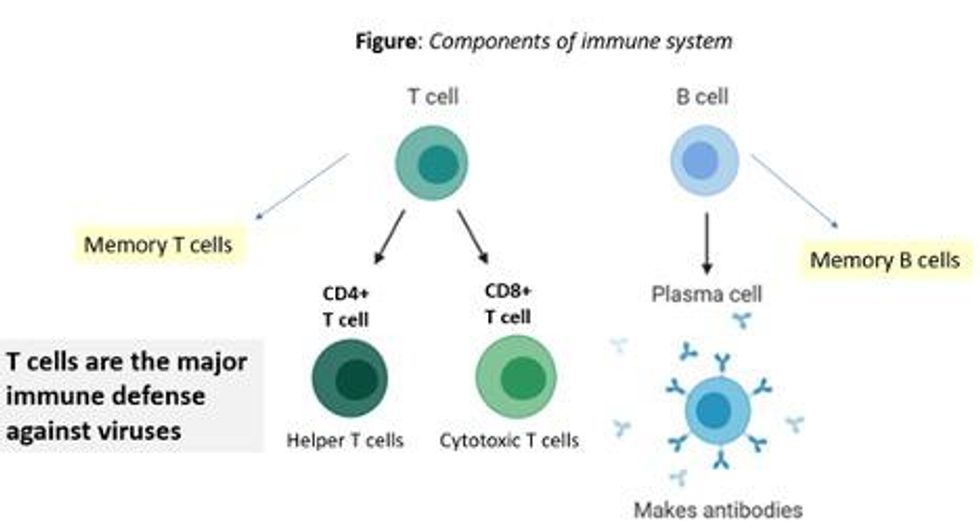
There are two major arms of the immune system: B cells (which produce antibodies) and T cells (which are formed specifically to attack and kill pathogens). T cells are divided into two types, CD4 cells ("helper" T cells) and CD8 cells ("cytotoxic" T cells).
Each arm, once stimulated by infection or vaccine, should hopefully make "memory" banks. So if the body sees the pathogen in the future, these defenses should come roaring back to attack the virus and protect you from getting sick. Plenty of research in COVID-19 indicates a likely long-lasting response to the vaccine or infection. Here are seven of the most compelling reasons:
REASON 1: Memory B Cells Are Produced By Vaccines and Natural Infection
In one study, 12 volunteers who had never had Covid-19--and were fully vaccinated with two Pfizer/BioNTech shots-- underwent biopsies of their lymph nodes. This is where memory B cells are stored in places called "germinal centers". The biopsies were performed three, four, six, and seven weeks after the first mRNA vaccine shot, and were stained to reveal that germinal center memory B cells in the lymph nodes increased in concentration over time.
Natural infection also generates memory B cells. Even after antibody levels wane over time, strong memory B cells were detected in the blood of individuals six and eight months after infection in different studies. Indeed, the half-lives of the memory B cells seen in the study examining patients 8 months after COVID-19 led the authors to conclude that "B cell memory to SARS-CoV-2 was robust and is likely long-lasting." Reason #2 tells us that memory B cells can be active for a very long time indeed.
REASON #2: Memory B Cells Can Produce Neutralizing Antibodies If They See Infection Again Decades Later
Demonstrated production of memory B cells after vaccination or natural infection with COVID-19 is so important because memory B cells, once generated, can be activated to produce high levels of neutralizing antibodies against the pathogen even if encountered many years after the initial exposure. In one amazing study (published in 2008), researchers isolated memory B cells against the 1918 flu strain from the blood of 32 individuals aged 91-101 years. These people had been born on or before 1915 and had survived that pandemic.
Their memory B cells, when exposed to the 1918 flu strain in a test tube, generated high levels of neutralizing antibodies against the virus -- antibodies that then protected mice from lethal infection with this deadly strain. The ability of memory B cells to produce complex antibody responses against an infection nine decades after exposure speaks to their durability.
REASON #3: Vaccines or Natural Infection Trigger Strong Memory T Cell Immunity
All of the trials of the major COVID-19 vaccine candidates measured strong T cell immunity following vaccination, most often assessed by measuring SARS-CoV-2 specific T cells in the phase I/II safety and immunogenicity studies. There are a number of studies that demonstrate the production of strong T cell immunity to COVID-19 after natural infection as well, even when the infection was mild or asymptomatic.
The same study that showed us robust memory B cell production 8 months after natural infection also demonstrated strong and sustained memory T cell production. In fact, the half-lives of the memory T cells in this cohort were long (~125-225 days for CD8+ and ~94-153 days for CD4+ T cells), comparable to the 123-day half-life observed for memory CD8+ T cells after yellow fever immunization (a vaccine usually given once over a lifetime).
A recent study of individuals recovered from COVID-19 show that the initial T cells generated by natural infection mature and differentiate over time into memory T cells that will be "put in the bank" for sustained periods.
REASON #4: T Cell Immunity Following Vaccinations for Other Infections Is Long-Lasting
Last year, we were fortunate to be able to measure how T cell immunity is generated by COVID-19 vaccines, which was not possible in earlier eras when vaccine trials were done for other infections (such as measles, mumps, rubella, pertussis, diphtheria). Antibodies are just the "tip of the iceberg" when assessing the response to vaccination, but were the only arm of the immune response that could be measured following vaccination in the past.
Measuring pathogen-specific T cell responses takes sophisticated technology. However, T cell responses, when assessed years after vaccination for other pathogens, has been shown to be long-lasting. For example, in one study of 56 volunteers who had undergone measles vaccination when they were much younger, strong CD8 and CD4 cell responses to vaccination could be detected up to 34 years later.
REASON #5: T Cell Immunity to Related Coronaviruses That Caused Severe Disease is Long-Lasting
SARS-CoV-2 is a coronavirus that causes severe disease, unlike coronaviruses that cause the common cold. Two other coronaviruses in the recent past caused severe disease, specifically Severely Acute Respiratory Distress Syndrome (SARS) in late 2002-2003 and Middle East Respiratory Syndrome (MERS) in 2011.
A study performed in 2020 demonstrated that the blood of 23 recovered SARS patients possess long-lasting memory T cells that were still reactive to SARS 17 years after the outbreak in 2003. Many scientists expect that T cell immunity to SARS-CoV-2 will be equally durable to that of its cousin.
REASON #6: T Cell Responses from Vaccination and Natural Infection With the Ancestral Strain of COVID-19 Are Robust Against Variants
Even though antibody responses from vaccination may be slightly lower against various COVID-19 variants of concern that have emerged in recent months, T cell immunity after vaccination has been shown to be unperturbed by mutations in the spike protein (in the variants). For instance, T cell responses after mRNA vaccines maintained strong activity against different variants (including P.1 Brazil variant, B.1.1.7 UK variant, B.1.351 South Africa variant and the CA.20.C California variant) in a recent study.
Another study showed that the vaccines generated robust T cell immunity that was unfazed by different variants, including B.1.351 and B.1.1.7. The CD4 and CD8 responses generated after natural infection are equally robust, showing activity against multiple "epitopes" (little segments) of the spike protein of the virus. For instance, CD8 cells responds to 52 epitopes and CD4 cells respond to 57 epitopes across the spike protein, so that a few mutations in the variants cannot knock out such a robust and in-breadth T cell response. Indeed, a recent paper showed that mRNA vaccines were 97.4 percent effective against severe COVID-19 disease in Qatar, even when the majority of circulating virus there was from variants of concern (B.1.351 and B.1.1.7).
REASON #7: Coronaviruses Don't Mutate Quickly Like Influenza, Which Requires Annual Booster Shots
Coronaviruses are RNA viruses, like influenza and HIV (which is actually a retrovirus), but do not mutate as quickly as either one. The reason that coronaviruses don't mutate very rapidly is that their replicating mechanism (polymerase) has a strong proofreading mechanism: If the virus mutates, it usually goes back and self-corrects. Mutations can arise with high rates of replication when transmission is very frequent -- as has been seen in recent months with the emergence of SARS-CoV-2 variants during surges. However, the COVID-19 virus will not be mutating like this when we tamp down transmission with mass vaccination.
In conclusion, I and many of my infectious disease colleagues expect the immunity from natural infection or vaccination to COVID-19 to be durable. Let's put discussion of boosters aside and work hard on global vaccine equity and distribution since the pandemic is not over until it is over for us all.
Professor Tim Caulfield stops by the "Making Sense of Science" podcast this month to discuss the infodemic around COVID-19 and how to deal with it.
The "Making Sense of Science" podcast features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
Hear the 30-second trailer:
Listen to the whole episode:
.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.