The New Prospective Parenthood: When Does More Info Become Too Much?

Obstetric ultrasound of a fourth-month fetus.
Peggy Clark was 12 weeks pregnant when she went in for a nuchal translucency (NT) scan to see whether her unborn son had Down syndrome. The sonographic scan measures how much fluid has accumulated at the back of the baby's neck: the more fluid, the higher the likelihood of an abnormality. The technician said the baby was in such an odd position, the test couldn't be done. Clark, whose name has been changed to protect her privacy, was told to come back in a week and a half to see if the baby had moved.
"With the growing sophistication of prenatal tests, it seems that the more questions are answered, the more new ones arise."
"It was like the baby was saying, 'I don't want you to know,'" she recently recalled.
When they went back, they found the baby had a thickened neck. It's just one factor in identifying Down's, but it's a strong indication. At that point, she was 13 weeks and four days pregnant. She went to the doctor the next day for a blood test. It took another two weeks for the results, which again came back positive, though there was still a .3% margin of error. Clark said she knew she wanted to terminate the pregnancy if the baby had Down's, but she didn't want the guilt of knowing there was a small chance the tests were wrong. At that point, she was too late to do a Chorionic villus sampling (CVS), when chorionic villi cells are removed from the placenta and sequenced. And she was too early to do an amniocentesis, which isn't done until between 14 and 20 weeks of the pregnancy. So she says she had to sit and wait, calling those few weeks "brutal."
By the time they did the amnio, she was already nearly 18 weeks pregnant and was getting really big. When that test also came back positive, she made the anguished decision to end the pregnancy.
Now, three years after Clark's painful experience, a newer form of prenatal testing routinely gives would-be parents more information much earlier on, especially for women who are over 35. As soon as nine weeks into their pregnancies, women can have a simple blood test to determine if there are abnormalities in the DNA of chromosomes 21, which indicates Down syndrome, as well as in chromosomes 13 and 18. Using next-generation sequencing technologies, the test separates out and examines circulating fetal cells in the mother's blood, which eliminates the risks of drawing fluid directly from the fetus or placenta.
"Finding out your baby has Down syndrome at 11 or 12 weeks is much easier for parents to make any decision they may want to make, as opposed to 16 or 17 weeks," said Dr. Leena Nathan, an obstetrician-gynecologist in UCLA's healthcare system. "People are much more willing or able to perhaps make a decision to terminate the pregnancy."
But with the growing sophistication of prenatal tests, it seems that the more questions are answered, the more new ones arise--questions that previous generations have never had to face. And as genomic sequencing improves in its predictive accuracy at the earliest stages of life, the challenges only stand to increase. Imagine, for example, learning your child's lifetime risk of breast cancer when you are ten weeks pregnant. Would you terminate if you knew she had a 70 percent risk? What about 40 percent? Lots of hard questions. Few easy answers. Once the cost of whole genome sequencing drops low enough, probably within the next five to ten years according to experts, such comprehensive testing may become the new standard of care. Welcome to the future of prospective parenthood.
"In one way, it's a blessing to have this information. On the other hand, it's very difficult to deal with."
How Did We Get Here?
Prenatal testing is not new. In 1979, amniocentesis was used to detect whether certain inherited diseases had been passed on to the fetus. Through the 1980s, parents could be tested to see if they carried disease like Tay-Sachs, Sickle cell anemia, Cystic fibrosis and Duchenne muscular dystrophy. By the early 1990s, doctors could test for even more genetic diseases and the CVS test was beginning to become available.
A few years later, a technique called preimplantation genetic diagnosis (PGD) emerged, in which embryos created in a lab with sperm and harvested eggs would be allowed to grow for several days and then cells would be removed and tested to see if any carried genetic diseases. Those that weren't affected could be transferred back to the mother. Once in vitro fertilization (IVF) took off, so did genetic testing. The labs test the embryonic cells and get them back to the IVF facilities within 24 hours so that embryo selection can occur. In the case of IVF, genetic tests are done so early, parents don't even have to decide whether to terminate a pregnancy. Embryos with issues often aren't even used.
"It was a very expensive endeavor but exciting to see our ability to avoid disorders, especially for families that don't want to terminate a pregnancy," said Sara Katsanis, an expert in genetic testing who teaches at Duke University. "In one way, it's a blessing to have this information (about genetic disorders). On the other hand, it's very difficult to deal with. To make that decision about whether to terminate a pregnancy is very hard."
Just Because We Can, Does It Mean We Should?
Parents in the future may not only find out whether their child has a genetic disease but will be able to potentially fix the problem through a highly controversial process called gene editing. But because we can, does it mean we should? So far, genes have been edited in other species, but to date, the procedure has not been used on an unborn child for reproductive purposes apart from research.
"There's a lot of bioethics debate and convening of groups to try to figure out where genetic manipulation is going to be useful and necessary, and where it is going to need some restrictions," said Katsanis. She notes that it's very useful in areas like cancer research, so one wouldn't want to over-regulate it.
There are already some criteria as to which genes can be manipulated and which should be left alone, said Evan Snyder, professor and director of the Center for Stem Cells and Regenerative Medicine at Sanford Children's Health Research Center in La Jolla, Calif. He noted that genes don't stand in isolation. That is, if you modify one that causes disease, will it disrupt others? There may be unintended consequences, he added.
"As the technical dilemmas get fixed, some of the ethical dilemmas get fixed. But others arise. It's kind of like ethical whack-a-mole."
But gene editing of embryos may take years to become an acceptable practice, if ever, so a more pressing issue concerns the rationale behind embryo selection during IVF. Prospective parents can end up with anywhere from zero to thirty embryos from the procedure and must choose only one (rarely two) to implant. Since embryos are routinely tested now for certain diseases, and selected or discarded based on that information, should it be ethical—and legal—to make selections based on particular traits, too? To date so far, parents can select for gender, but no other traits. Whether trait selection becomes routine is a matter of time and business opportunity, Katsanis said. So far, the old-fashioned way of making a baby combined with the luck of the draw seems to be the preferred method for the marketplace. But that could change.
"You can easily see a family deciding not to implant a lethal gene for Tay-Sachs or Duchene or Cystic fibrosis. It becomes more ethically challenging when you make a decision to implant girls and not any of the boys," said Snyder. "And then as we get better and better, we can start assigning genes to certain skills and this starts to become science fiction."
Once a pregnancy occurs, prospective parents of all stripes will face decisions about whether to keep the fetus based on the information that increasingly robust prenatal testing will provide. What influences their decision is the crux of another ethical knot, said Snyder. A clear-cut rationale would be if the baby is anencephalic, or it has no brain. A harder one might be, "It's a girl, and I wanted a boy," or "The child will only be 5' 2" tall in adulthood."
"Those are the extremes, but the ultimate question is: At what point is it a legitimate response to say, I don't want to keep this baby?'" he said. Of course, people's responses will vary, so the bigger conundrum for society is: Where should a line be drawn—if at all? Should a woman who is within the legal scope of termination (up to around 24 weeks, though it varies by state) be allowed to terminate her pregnancy for any reason whatsoever? Or must she have a so-called "legitimate" rationale?
"As the technical dilemmas get fixed, some of the ethical dilemmas get fixed. But others arise. It's kind of like ethical whack-a-mole," Snyder said.
One of the newer moles to emerge is, if one can fix a damaged gene, for how long should it be fixed? In one child? In the family's whole line, going forward? If the editing is done in the embryo right after the egg and sperm have united and before the cells begin dividing and becoming specialized, when, say, there are just two or four cells, it will likely affect that child's entire reproductive system and thus all of that child's progeny going forward.
"This notion of changing things forever is a major debate," Snyder said. "It literally gets into metaphysics. On the one hand, you could say, well, wouldn't it be great to get rid of Cystic fibrosis forever? What bad could come of getting rid of a mutant gene forever? But we're not smart enough to know what other things the gene might be doing, and how disrupting one thing could affect this network."
As with any tool, there are risks and benefits, said Michael Kalichman, Director of the Research Ethics Program at the University of California San Diego. While we can envision diverse benefits from a better understanding of human biology and medicine, it is clear that our species can also misuse those tools – from stigmatizing children with certain genetic traits as being "less than," aka dystopian sci-fi movies like Gattaca, to judging parents for making sure their child carries or doesn't carry a particular trait.
"The best chance to ensure that the benefits of this technology will outweigh the risks," Kalichman said, "is for all stakeholders to engage in thoughtful conversations, strive for understanding of diverse viewpoints, and then develop strategies and policies to protect against those uses that are considered to be problematic."
DNA- and RNA-based electronic implants may revolutionize healthcare
The test tubes contain tiny DNA/enzyme-based circuits, which comprise TRUMPET, a new type of electronic device, smaller than a cell.
Implantable electronic devices can significantly improve patients’ quality of life. A pacemaker can encourage the heart to beat more regularly. A neural implant, usually placed at the back of the skull, can help brain function and encourage higher neural activity. Current research on neural implants finds them helpful to patients with Parkinson’s disease, vision loss, hearing loss, and other nerve damage problems. Several of these implants, such as Elon Musk’s Neuralink, have already been approved by the FDA for human use.
Yet, pacemakers, neural implants, and other such electronic devices are not without problems. They require constant electricity, limited through batteries that need replacements. They also cause scarring. “The problem with doing this with electronics is that scar tissue forms,” explains Kate Adamala, an assistant professor of cell biology at the University of Minnesota Twin Cities. “Anytime you have something hard interacting with something soft [like muscle, skin, or tissue], the soft thing will scar. That's why there are no long-term neural implants right now.” To overcome these challenges, scientists are turning to biocomputing processes that use organic materials like DNA and RNA. Other promised benefits include “diagnostics and possibly therapeutic action, operating as nanorobots in living organisms,” writes Evgeny Katz, a professor of bioelectronics at Clarkson University, in his book DNA- And RNA-Based Computing Systems.
While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output.
Adamala’s research focuses on developing such biocomputing systems using DNA, RNA, proteins, and lipids. Using these molecules in the biocomputing systems allows the latter to be biocompatible with the human body, resulting in a natural healing process. In a recent Nature Communications study, Adamala and her team created a new biocomputing platform called TRUMPET (Transcriptional RNA Universal Multi-Purpose GatE PlaTform) which acts like a DNA-powered computer chip. “These biological systems can heal if you design them correctly,” adds Adamala. “So you can imagine a computer that will eventually heal itself.”
The basics of biocomputing
Biocomputing and regular computing have many similarities. Like regular computing, biocomputing works by running information through a series of gates, usually logic gates. A logic gate works as a fork in the road for an electronic circuit. The input will travel one way or another, giving two different outputs. An example logic gate is the AND gate, which has two inputs (A and B) and two different results. If both A and B are 1, the AND gate output will be 1. If only A is 1 and B is 0, the output will be 0 and vice versa. If both A and B are 0, the result will be 0. While a computer gives these inputs in binary code or "bits," such as a 0 or 1, biocomputing uses DNA strands as inputs, whether double or single-stranded, and often uses fluorescent RNA as an output. In this case, the DNA enters the logic gate as a single or double strand.
If the DNA is double-stranded, the system “digests” the DNA or destroys it, which results in non-fluorescence or “0” output. Conversely, if the DNA is single-stranded, it won’t be digested and instead will be copied by several enzymes in the biocomputing system, resulting in fluorescent RNA or a “1” output. And the output for this type of binary system can be expanded beyond fluorescence or not. For example, a “1” output might be the production of the enzyme insulin, while a “0” may be that no insulin is produced. “This kind of synergy between biology and computation is the essence of biocomputing,” says Stephanie Forrest, a professor and the director of the Biodesign Center for Biocomputing, Security and Society at Arizona State University.
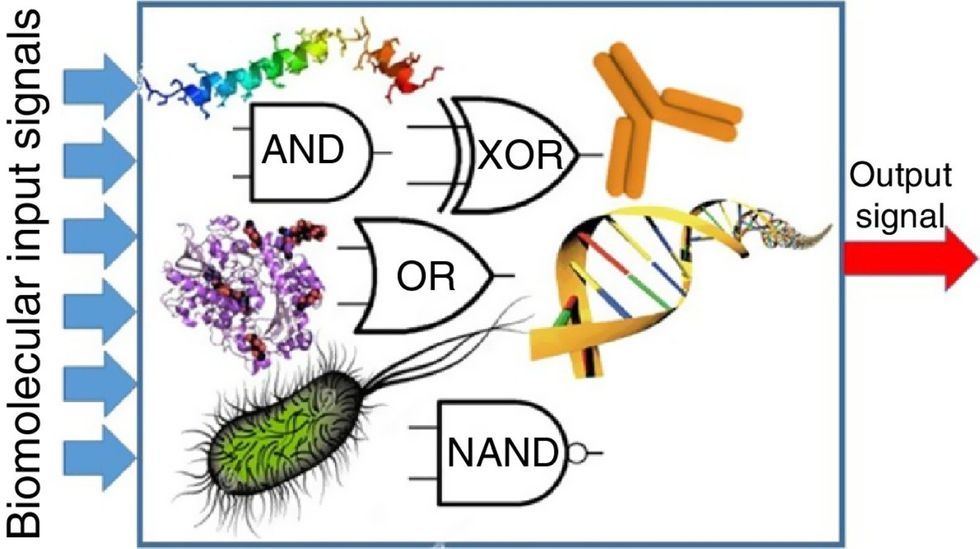
Biocomputing circles are made of DNA, RNA, proteins and even bacteria.
Evgeny Katz
The TRUMPET’s promise
Depending on whether the biocomputing system is placed directly inside a cell within the human body, or run in a test-tube, different environmental factors play a role. When an output is produced inside a cell, the cell's natural processes can amplify this output (for example, a specific protein or DNA strand), creating a solid signal. However, these cells can also be very leaky. “You want the cells to do the thing you ask them to do before they finish whatever their businesses, which is to grow, replicate, metabolize,” Adamala explains. “However, often the gate may be triggered without the right inputs, creating a false positive signal. So that's why natural logic gates are often leaky." While biocomputing outside a cell in a test tube can allow for tighter control over the logic gates, the outputs or signals cannot be amplified by a cell and are less potent.
TRUMPET, which is smaller than a cell, taps into both cellular and non-cellular biocomputing benefits. “At its core, it is a nonliving logic gate system,” Adamala states, “It's a DNA-based logic gate system. But because we use enzymes, and the readout is enzymatic [where an enzyme replicates the fluorescent RNA], we end up with signal amplification." This readout means that the output from the TRUMPET system, a fluorescent RNA strand, can be replicated by nearby enzymes in the platform, making the light signal stronger. "So it combines the best of both worlds,” Adamala adds.
These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body.
The TRUMPET biocomputing process is relatively straightforward. “If the DNA [input] shows up as single-stranded, it will not be digested [by the logic gate], and you get this nice fluorescent output as the RNA is made from the single-stranded DNA, and that's a 1,” Adamala explains. "And if the DNA input is double-stranded, it gets digested by the enzymes in the logic gate, and there is no RNA created from the DNA, so there is no fluorescence, and the output is 0." On the story's leading image above, if the tube is "lit" with a purple color, that is a binary 1 signal for computing. If it's "off" it is a 0.
While still in research, TRUMPET and other biocomputing systems promise significant benefits to personalized healthcare and medicine. These organic-based systems could detect cancer cells or low insulin levels inside a patient’s body. The study’s lead author and graduate student Judee Sharon is already beginning to research TRUMPET's ability for earlier cancer diagnoses. Because the inputs for TRUMPET are single or double-stranded DNA, any mutated or cancerous DNA could theoretically be detected from the platform through the biocomputing process. Theoretically, devices like TRUMPET could be used to detect cancer and other diseases earlier.
Adamala sees TRUMPET not only as a detection system but also as a potential cancer drug delivery system. “Ideally, you would like the drug only to turn on when it senses the presence of a cancer cell. And that's how we use the logic gates, which work in response to inputs like cancerous DNA. Then the output can be the production of a small molecule or the release of a small molecule that can then go and kill what needs killing, in this case, a cancer cell. So we would like to develop applications that use this technology to control the logic gate response of a drug’s delivery to a cell.”
Although platforms like TRUMPET are making progress, a lot more work must be done before they can be used commercially. “The process of translating mechanisms and architecture from biology to computing and vice versa is still an art rather than a science,” says Forrest. “It requires deep computer science and biology knowledge,” she adds. “Some people have compared interdisciplinary science to fusion restaurants—not all combinations are successful, but when they are, the results are remarkable.”
Crickets are low on fat, high on protein, and can be farmed sustainably. They are also crunchy.
In today’s podcast episode, Leaps.org Deputy Editor Lina Zeldovich speaks about the health and ecological benefits of farming crickets for human consumption with Bicky Nguyen, who joins Lina from Vietnam. Bicky and her business partner Nam Dang operate an insect farm named CricketOne. Motivated by the idea of sustainable and healthy protein production, they started their unconventional endeavor a few years ago, despite numerous naysayers who didn’t believe that humans would ever consider munching on bugs.
Yet, making creepy crawlers part of our diet offers many health and planetary advantages. Food production needs to match the rise in global population, estimated to reach 10 billion by 2050. One challenge is that some of our current practices are inefficient, polluting and wasteful. According to nonprofit EarthSave.org, it takes 2,500 gallons of water, 12 pounds of grain, 35 pounds of topsoil and the energy equivalent of one gallon of gasoline to produce one pound of feedlot beef, although exact statistics vary between sources.
Meanwhile, insects are easy to grow, high on protein and low on fat. When roasted with salt, they make crunchy snacks. When chopped up, they transform into delicious pâtes, says Bicky, who invents her own cricket recipes and serves them at industry and public events. Maybe that’s why some research predicts that edible insects market may grow to almost $10 billion by 2030. Tune in for a delectable chat on this alternative and sustainable protein.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Further reading:
More info on Bicky Nguyen
https://yseali.fulbright.edu.vn/en/faculty/bicky-n...
The environmental footprint of beef production
https://www.earthsave.org/environment.htm
https://www.watercalculator.org/news/articles/beef-king-big-water-footprints/
https://www.frontiersin.org/articles/10.3389/fsufs.2019.00005/full
https://ourworldindata.org/carbon-footprint-food-methane
Insect farming as a source of sustainable protein
https://www.insectgourmet.com/insect-farming-growing-bugs-for-protein/
https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/insect-farming
Cricket flour is taking the world by storm
https://www.cricketflours.com/
https://talk-commerce.com/blog/what-brands-use-cricket-flour-and-why/

Lina Zeldovich has written about science, medicine and technology for Popular Science, Smithsonian, National Geographic, Scientific American, Reader’s Digest, the New York Times and other major national and international publications. A Columbia J-School alumna, she has won several awards for her stories, including the ASJA Crisis Coverage Award for Covid reporting, and has been a contributing editor at Nautilus Magazine. In 2021, Zeldovich released her first book, The Other Dark Matter, published by the University of Chicago Press, about the science and business of turning waste into wealth and health. You can find her on http://linazeldovich.com/ and @linazeldovich.

