Her Incredible Sense of Smell Helped Scientists Develop the First Parkinson's Test

Joy Milne's unusual sense of smell led Dr. Tilo Kunath, a neurobiologist at the Centre for Regenerative Medicine at the University of Edinburgh, and a host of other scientists, to develop a new diagnostic test for Parkinson's.
Forty years ago, Joy Milne, a nurse from Perth, Scotland, noticed a musky odor coming from her husband, Les. At first, Milne thought the smell was a result of bad hygiene and badgered her husband to take longer showers. But when the smell persisted, Milne learned to live with it, not wanting to hurt her husband's feelings.
Twelve years after she first noticed the "woodsy" smell, Les was diagnosed at the age of 44 with Parkinson's Disease, a neurodegenerative condition characterized by lack of dopamine production and loss of movement. Parkinson's Disease currently affects more than 10 million people worldwide.
Milne spent the next several years believing the strange smell was exclusive to her husband. But to her surprise, at a local support group meeting in 2012, she caught the familiar scent once again, hanging over the group like a cloud. Stunned, Milne started to wonder if the smell was the result of Parkinson's Disease itself.
Milne's discovery led her to Dr. Tilo Kunath, a neurobiologist at the Centre for Regenerative Medicine at the University of Edinburgh. Together, Milne, Kunath, and a host of other scientists would use Milne's unusual sense of smell to develop a new diagnostic test, now in development and poised to revolutionize the treatment of Parkinson's Disease.
"Joy was in the audience during a talk I was giving on my work, which has to do with Parkinson's and stem cell biology," Kunath says. "During the patient engagement portion of the talk, she asked me if Parkinson's had a smell to it." Confused, Kunath said he had never heard of this – but for months after his talk he continued to turn the question over in his mind.
Kunath knew from his research that the skin's microbiome changes during different disease processes, releasing metabolites that can give off odors. In the medical literature, diseases like melanoma and Type 2 diabetes have been known to carry a specific scent – but no such connection had been made with Parkinson's. If people could smell Parkinson's, he thought, then it stood to reason that those metabolites could be isolated, identified, and used to potentially diagnose Parkinson's by their presence alone.
First, Kunath and his colleagues decided to test Milne's sense of smell. "I got in touch with Joy again and we designed a protocol to test her sense of smell without her having to be around patients," says Kunath, which could have affected the validity of the test. In his spare time, Kunath collected t-shirt samples from people diagnosed with Parkinson's and from others without the diagnosis and gave them to Milne to smell. In 100 percent of the samples, Milne was able to detect whether a person had Parkinson's based on smell alone. Amazingly, Milne was even able to detect the "Parkinson's scent" in a shirt from the control group – someone who did not have a Parkinson's diagnosis, but would go on to be diagnosed nine months later.
From the initial study, the team discovered that Parkinson's did have a smell, that Milne – inexplicably – could detect it, and that she could detect it long before diagnosis like she had with her husband, Les. But the experiments revealed other things that the team hadn't been expecting.
"One surprising thing we learned from that experiment was that the odor was always located in the back of the shirt – never in the armpit, where we expected the smell to be," Kunath says. "I had a chance meeting with a dermatologist and he said the smell was due to the patient's sebum, which are greasy secretions that are really dense on your upper back. We have sweat glands, instead of sebum, in our armpits." Patients with Parkinson's are also known to have increased sebum production.
With the knowledge that a patient's sebum was the source of the unusual smell, researchers could go on to investigate exactly what metabolites were in the sebum and in what amounts. Kunath, along with his associate, Dr. Perdita Barran, collected and analyzed sebum samples from 64 participants across the United Kingdom. Once the samples were collected, Barran and others analyzed it using a method called gas chromatography mass spectrometry, or GS-MC, which separated, weighed and helped identify the individual compounds present in each sebum sample.
Barran's team can now correctly identify Parkinson's in nine out of 10 patients – a much quicker and more accurate way to diagnose than what clinicians do now.
"The compounds we've identified in the sebum are not unique to people with Parkinson's, but they are differently expressed," says Barran, a professor of mass spectrometry at the University of Manchester. "So this test we're developing now is not a black-and-white, do-you-have-something kind of test, but rather how much of these compounds do you have compared to other people and other compounds." The team identified over a dozen compounds that were present in the sebum of Parkinson's patients in much larger amounts than the control group.
Using only the GC-MS and a sebum swab test, Barran's team can now correctly identify Parkinson's in nine out of 10 patients – a much quicker and more accurate way to diagnose than what clinicians do now.
"At the moment, a clinical diagnosis is based on the patient's physical symptoms," Barran says, and determining whether a patient has Parkinson's is often a long and drawn-out process of elimination. "Doctors might say that a group of symptoms looks like Parkinson's, but there are other reasons people might have those symptoms, and it might take another year before they're certain," Barran says. "Some of those symptoms are just signs of aging, and other symptoms like tremor are present in recovering alcoholics or people with other kinds of dementia." People under the age of 40 with Parkinson's symptoms, who present with stiff arms, are often misdiagnosed with carpal tunnel syndrome, she adds.
Additionally, by the time physical symptoms are present, Parkinson's patients have already lost a substantial amount of dopamine receptors – about sixty percent -- in the brain's basal ganglia. Getting a diagnosis before physical symptoms appear would mean earlier interventions that could prevent dopamine loss and preserve regular movement, Barran says.
"Early diagnosis is good if it means there's a chance of early intervention," says Barran. "It stops the process of dopamine loss, which means that motor symptoms potentially will not happen, or the onset of symptoms will be substantially delayed." Barran's team is in the processing of streamlining the sebum test so that definitive results will be ready in just two minutes.
"What we're doing right now will be a very inexpensive test, a rapid-screen test, and that will encourage people to self-sample and test at home," says Barran. In addition to diagnosing Parkinson's, she says, this test could also be potentially useful to determine if medications were at a therapeutic dose in people who have the disease, since the odor is strongest in people whose symptoms are least controlled by medication.
"When symptoms are under control, the odor is lower," Barran says. "Potentially this would allow patients and clinicians to see whether their symptoms are being managed properly with medication, or perhaps if they're being overmedicated." Hypothetically, patients could also use the test to determine if interventions like diet and exercise are effective at keeping Parkinson's controlled.
"We hope within the next two to five years we will have a test available."
Barran is now running another clinical trial – one that determines whether they can diagnose at an earlier stage and whether they can identify a difference in sebum samples between different forms of Parkinson's or diseases that have Parkinson's-like symptoms, such as Lewy Body Dementia.
"Within the next one to two years, we hope to be running a trial in the Manchester area for those people who do not have motor symptoms but are at risk for developing dementia due to symptoms like loss of smell and sleep difficulty," Barran had said in 2019. "If we can establish that, we can roll out a test that determines if you have Parkinson's or not with those first pre-motor symptoms, and then at what stage. We hope within the next two to five years we will have a test available."
In a 2022 study, published in the American Chemical Society, researchers used mass spectrometry to analyze sebum from skin swabs for the presence of the specific molecules. They found that some specific molecules are present only in people who have Parkinson’s. Now they hope that the same method can be used in regular diagnostic labs. The test, many years in the making, is inching its way to the clinic.
"We would likely first give this test to people who are at risk due to a genetic predisposition, or who are at risk based on prodomal symptoms, like people who suffer from a REM sleep disorder who have a 50 to 70 percent chance of developing Parkinson's within a ten year period," Barran says. "Those would be people who would benefit from early therapeutic intervention. For the normal population, it isn't beneficial at the moment to know until we have therapeutic interventions that can be useful."
Milne's husband, Les, passed away from complications of Parkinson's Disease in 2015. But thanks to him and the dedication of his wife, Joy, science may have found a way to someday prolong the lives of others with this devastating disease. Sometimes she can smell people who have Parkinson’s while in the supermarket or walking down the street but has been told by medical ethicists she cannot tell them, Milne said in an interview with the Guardian. But once the test becomes available in the clinics, it will do the job for her.
[Ed. Note: A older version of this hit article originally ran on September 3, 2019.]
The Nation’s Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored?
Morale at federal science agencies -- and public trust in their guidance -- is at a concerning low right now.
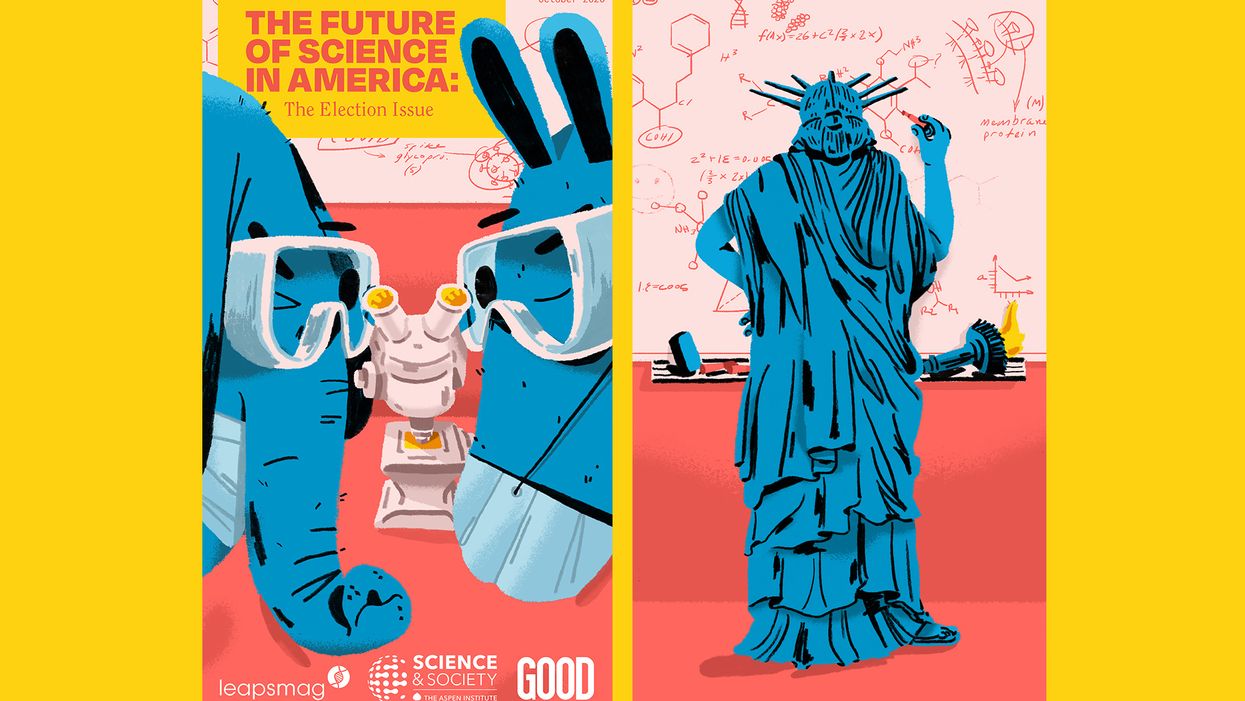
This article is part of the magazine, "The Future of Science In America: The Election Issue," co-published by LeapsMag, the Aspen Institute Science & Society Program, and GOOD.
It didn't have to be this way. More than 200,000 Americans dead, seven million infected, with numbers continuing to climb, an economy in shambles with millions out of work, hundreds of thousands of small businesses crushed with most of the country still under lockdown. And all with no end in sight. This catastrophic result is due in large part to the willful disregard of scientific evidence and of muzzling policy experts by the Trump White House, which has spent its entire time in office attacking science.
One of the few weapons we had to combat the spread of Covid-19—wearing face masks—has been politicized by the President, who transformed this simple public health precaution into a first amendment issue to rally his base. Dedicated public health officials like Dr. Anthony Fauci, the highly respected director of the National Institute of Allergies and Infectious Diseases, have received death threats, which have prompted many of them around the country to resign.
Over the summer, the Trump White House pressured the Centers for Disease Control, which is normally in charge of fighting epidemics, to downplay COVID risks among young people and encourage schools to reopen. And in late September, the CDC was forced to pull federal teams who were going door-to-door doing testing surveys in Minnesota because of multiple incidents of threats and abuse. This list goes on and on.
Still, while the Trump administration's COVID failures are the most visible—and deadly—the nation's entire federal science infrastructure has been undermined in ways large and small.
The White House has steadily slashed monies for science—the 2021 budget cuts funding by 10–30% or more for crucial agencies like National Oceanic and Atmospheric Administration (NOAA) and the Environmental Protection Agency (EPA)—and has gutted health and science agencies across the board, including key agencies of the Department of Energy and the Interior, especially in divisions that deal with issues they oppose ideologically like climate change.
Even farmers can't get reliable information about how climate change affects planting seasons because the White House moved the entire staff at the U.S. Department of Agriculture agency who does this research, relocating them from Maryland to Kansas City, Missouri. Many of these scientists couldn't uproot their families and sell their homes, so the division has had to pretty much start over from scratch with a skeleton crew.
More than 1,600 federal scientists left government in the first two years of the Trump Administration, according to data compiled by the Washington Post, and one-fifth of top positions in science are vacant, depriving agencies of the expertise they need to fulfill their vital functions. Industry executives and lobbyists have been installed as gatekeepers—HHS Secretary Alex Azar was previously president of Eli Lilly, and three climate change deniers were appointed to key posts at the National Oceanic and Atmospheric Administration, to cite just a couple of examples. Trump-appointed officials have sidelined, bullied, or even vilified those who dare to speak out, which chills the rigorous debate that is the essential to sound, independent science.
"The CDC needs to be able to speak regularly to the American people to explain what it knows and how it knows it."
Linda Birnbaum knows firsthand what it's like to become a target. The microbiologist recently retired after more than a decade as the director of the National Institute of Environmental Health Sciences, which is the world's largest environmental health organization and the greatest funder of environmental health and toxicology research, a position that often put her agency at odds with the chemical and fossil fuel industry. There was an attempt to get her fired, she says, "because I had the nerve to write that science should be used in making policy. The chemical industry really went after me, and my last two years were not so much fun under this administration. I'd like to believe it was because I was making a difference—if I wasn't, they wouldn't care."
Little wonder that morale at federal agencies is low. "We're very frustrated," says Dr. William Schaffner, a veteran infectious disease specialist and a professor of medicine at the Vanderbilt University School of Medicine in Nashville. "My colleagues within these agencies, the CDC rank and file, are keeping their heads down doing the best they can, and they hope to weather this storm."
The cruel irony is that the United States was once a beacon of scientific innovation. In the heady post World War II years, while Europe lay in ruins, the successful development of penicillin and the atomic bomb—which Americans believed helped vanquish the Axis powers—unleashed a gusher of public money into research, launching an unprecedented era of achievement in American science. Scientists conquered polio, deciphered the genetic code, harnessed the power of the atom, invented lasers, transistors, microchips and computers, sent missions beyond Mars, and landed men on the moon. A once-inconsequential hygiene laboratory was transformed into the colossus the National Institutes of Health has become, which remains today the world's flagship medical research center, unrivaled in size and scope.
At the same time, a tiny public health agency headquartered in Atlanta, which had been in charge of eradicating the malaria outbreaks that plagued impoverished rural areas in the Deep South until the late 1940s, evolved into the Centers for Disease Control and Prevention. The CDC became the world's leader in fighting disease outbreaks, and the agency's crack team of epidemiologists—members of the vaunted Epidemic Intelligence Service—were routinely dispatched to battle global outbreaks of contagions such as Ebola and malaria and help lead the vaccination campaigns to eradicate killers like polio and small pox that have saved millions of lives.
What will it take to rebuild our federal science infrastructure and restore not only the public's confidence but the respect of the world's scientific community? There are some hopeful signs that there is pushback against the current national leadership, and non-profit watchdog groups like the Union of Concerned Scientists have mapped out comprehensive game plans to restore public trust and the integrity of science.
These include methods of protecting science from political manipulation; restoring the oversight role of independent federal advisory committees, whose numbers were decimated by recent executive orders; strengthening scientific agencies that have been starved by budget cuts and staff attrition; and supporting whistleblower protections and allowing scientists to do their jobs without political meddling to restore integrity to the process. And this isn't just a problem at the CDC. A survey of 1,600 EPA scientists revealed that more than half had been victims of political interference and were pressured to skew their findings, according to research released in April by the Union of Concerned Scientists.
"Federal agencies are staffed by dedicated professionals," says Andrew Rosenberg, director of the Center for Science and Democracy at the Union of Concerned Scientists and a former fisheries biologist for NOAA. "Their job is not to serve the president but the public interest. Inspector generals are continuing to do what they're supposed to, but their findings are not being adhered to. But they need to hold agencies accountable. If an agency has not met its mission or engaged in misconduct, there needs to be real consequences."
On other fronts, last month nine vaccine makers, including Sanofi, Pfizer, and AstraZeneca, took the unprecedented stop of announcing that their COVID-19 vaccines would be thoroughly vetted before they were released. In their implicit refusal to bow to political pressure from the White House to have a vaccine available before the election, their goal was to restore public confidence in vaccine safety, and ensure that enough Americans would consent to have the shot when it was eventually approved so that we'd reach the long-sought holy grail of herd immunity.
"That's why it's really important that all of the decisions need to be made with complete transparency and not taking shortcuts," says Dr. Tom Frieden, president and CEO of Resolve to Save Lives and former director of the CDC during the H1N1, Ebola, and Zika emergencies. "A vaccine is our most important tool, and we can't break that tool by meddling in the science approval process."
In late September, Senate Democrats introduced a new bill to halt political meddling in public health initiatives by the White House. Called Science and Transparency Over Politics Act (STOP), the legislation would create an independent task force to investigate political interference in the federal response to the coronavirus pandemic. "The Trump administration is still pushing the president's political priorities rather than following the science to defeat this virus," Senate Minority Leader Chuck Schumer said in a press release.
To effectively bring the pandemic under control and restore public confidence, the CDC must assume the leadership role in fighting COVID-19. During previous outbreaks, the top federal infectious disease specialists like Drs. Fauci and Frieden would have daily press briefings, and these need to resume. "The CDC needs to be able to speak regularly to the American people to explain what it knows and how it knows it," says Frieden, who cautions that a vaccine won't be a magic bullet. "There is no one thing that is going to make this virus go away. We need to continue to limit indoor exposures, wear masks, and do strategic testing, isolation, and quarantine. We need a comprehensive approach, and not just a vaccine."
We must also appoint competent and trustworthy leaders, says Rosenberg of the Union of Concerned Scientists. Top posts in too many science agencies are now filled by former industry executives and lobbyists with a built-in bias, as well as people lacking relevant scientific experience, many of whom were never properly vetted because of the current administration's penchant for bypassing Congress and appointing "acting" officials. "We've got great career people who have hung in, but in so much of the federal government, they just put in 'acting' people," says Linda Birnbaum. "They need to bring in better, qualified senior leadership."
Open positions need to be filled, too. Federal science agencies have been seriously crippled by staffing attrition, and the Trump Administration instituted a hiring freeze when it first came in. Staffing levels remain at least ten percent down from previous levels, says Birnbaum and in many agencies, like the EPA, "everything has come to a screeching halt, making it difficult to get anything done."
But in the meantime, the critical first step may be at the ballot box in November. Even Scientific American, the esteemed consumer science publication, for the first time in its 175-year history felt "compelled" to endorse a presidential candidate, Joe Biden, because of the enormity of the damage they say Donald Trump has inflicted on scientists, their legal protections, and on the federal science agencies.
"If the current administration continues, the national political leadership will be emboldened and will be even more assertive of their executive prerogatives and less concerned about traditional niceties, leading to further erosion of the activities of many federal agencies," says Vanderbilt's William Schaffner. "But the reality is, if the team is losing, you change the coach. Then agencies really have to buckle down because it will take some time to restore their hard-earned reputations."
[Editor's Note: To read other articles in this special magazine issue, visit the beautifully designed e-reader version.]
Announcing "The Future of Science in America: The Election Issue"
This special magazine explores what's at stake for science & policy over the next four years.
As reviewed in The Washington Post, "Tomorrow's challenges in science and politics: Magazine offers in-depth takes on these U.S. issues":
"Is it time for a new way to help make adults more science-literate? What should the next president know about science? Could science help strengthen American democracy? "The Future of Science in America: The Election Issue" has answers. The free, online magazine is packed with interesting takes on how science can serve the common good. And just in time. This year has challenged leaders, researchers and the public with thorny scientific questions, from the coronavirus pandemic to widespread misinformation on scientific issues. The magazine is a collaboration of the Aspen Institute, a think tank that brings together a variety of public figures and private individuals to tackle thorny social issues, the digital science magazine Leapsmag and GOOD, a social impact company. It's packed with 15 in-depth articles about science with a view toward our campaign year."
The Future of Science in America: The Election Issue offers wide-ranging perspectives on challenges and opportunities for science as we elect our next national and local leaders. The fast-striking COVID-19 pandemic and the more slowly moving pandemic of climate change have brought into sharp focus how reliant we will be on science and public policy to work together to rescue us from crisis. Doing so will require cooperation between both political parties, as well as significant public trust in science as a beacon to light the path forward.
In spite of its unfortunate emergence as a flash point between two warring parties, we believe that science is the driving force for universal progress. No endeavor is more noble than the quest to rigorously understand our world and apply that knowledge to further human flourishing. This magazine aspires to promote roadmaps for science as a tool for health, a vehicle for progress, and a unifier of our nation.
This special issue is a collaboration among LeapsMag, the Aspen Institute Science & Society Program, and GOOD, with support from the Gordon and Betty Moore Foundation and the Rita Allen Foundation.
It is available as a free, beautifully designed digital magazine for both desktop and mobile.
TABLE OF CONTENTS:
- SCIENTISTS:
Award-Winning Scientists Offer Advice to the Next President of the United States - PUBLIC OPINION:
National Survey Reveals Americans' Most Important Scientific Priorities - GOVERNMENT:
The Nation's Science and Health Agencies Face a Credibility Crisis: Can Their Reputations Be Restored? - TELEVISION:
To Make Science Engaging, We Need a Sesame Street for Adults - IMMIGRATION:
Immigrant Scientists—and America's Edge—Face a Moment of Truth This Election - RACIAL JUSTICE:
Democratize the White Coat by Honoring Black, Indigenous, and People of Color in Science - EDUCATION:
I'm a Black, Genderqueer Medical Student: Here's My Hard-Won Wisdom for Students and Educational Institutions - TECHNOLOGY:
"Deep Fake" Video Technology Is Advancing Faster Than Our Policies Can Keep Up - VOTERS:
Mind the (Vote) Gap: Can We Get More STEM Students to the Polls? - EXPERTS:
Who Qualifies as an "Expert" and How Can We Decide Who Is Trustworthy? - SOCIAL MEDIA:
Why Your Brain Falls for Misinformation—And How to Avoid It - YOUTH:
Youth Climate Activists Expand Their Focus and Collaborate to Get Out the Vote - SUPREME COURT:
Abortions Before Fetal Viability Are Legal: Might Science and a Change on the Supreme Court Undermine That? - NAVAJO NATION:
An Environmental Scientist and an Educator Highlight Navajo Efforts to Balance Tradition with Scientific Priorities - CIVIC SCIENCE:
Want to Strengthen American Democracy? The Science of Collaboration Can Help
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.