How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
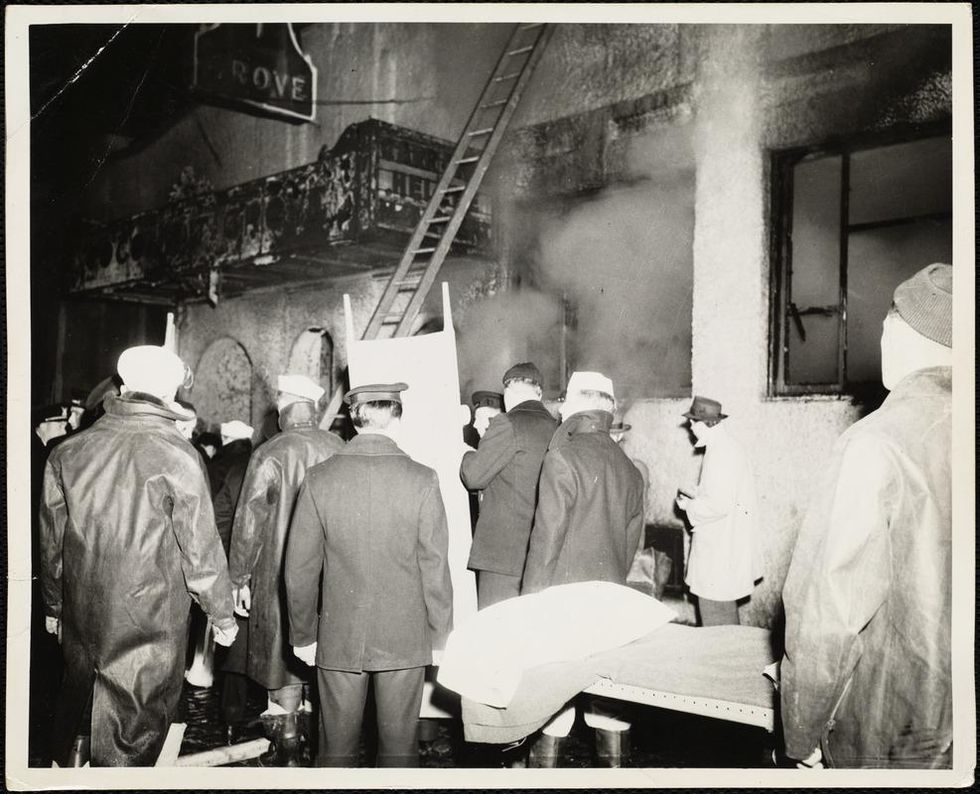
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
Vaccine passports, if required by businesses and universities, may give people a false sense of security, one expert cautions.
Vaccines are one of the greatest public health accomplishments of all time. For centuries, public health has relied on vaccinations to prevent and control disease outbreaks for a plethora of infectious scourges, with our crowning achievement being the successful eradication of smallpox.
The purpose of vaccine documentation is to provide proof of an individual's protection from either becoming infected or transmitting a vaccine-preventable disease. Vouching for these protections requires a firm knowledge about the epidemiology of the disease, as well as scientific knowledge concerning the efficacy of the vaccine. The vaccines we currently require be documented have met these tests; the vaccine for COVID-19 has not yet been proven to do so.
Let's acknowledge that the term "vaccine passport" is a poor choice of words. Passports are a legal travel document created by nations and governed by law for identification of the bearer to control entry and exit from nation states. They often serve as legal forms of identification and as a record of international travel. They are generally very sophisticated documents that have been created in a secure manner and may include a range of electronic and, in some cases, biometric measures such as fingerprints to ensure the holder is indeed who they say they are. Vaccine passports are medical documents used to document the vaccination status of an individual. They do not undergo the same level of administrative scrutiny and cannot be used to verify that the presenter is indeed the vaccinated individual. Some companies do have electronic methods to address concerns about verification; however, most people currently have paper records that can be easily falsified.
"Vaccine passports" as currently proposed risk giving people a false sense of security.
Successful disease control from vaccination programs relies on the ability to vaccinate at a level that prevents large-scale disease spread and the ability to rapidly identify the presence of disease outbreaks. It requires reliable, safe, and effective vaccines that are easily delivered in clinical and nonclinical settings. Keeping vaccination information as a part of the medical record, and even having a separate specialized vaccine record for personal use, is a time-honored tradition.
Keeping a vaccination record provides a method to keep track of the many shots one receives and serves as a visual reminder to help ensure the appropriate vaccine shot schedule is maintained for vaccines requiring multiple doses. The vaccine record, when combined with vaccine safety monitoring systems, serves as a mechanism to track adverse events to monitor and ensure the safety of vaccines as a consumer product. The record also serves as the official record of vaccination when required for administrative or legally prescribed purposes.
"Vaccine passports" as currently proposed risk giving people a false sense of security. In the case of the COVID-19 vaccines currently approved for use, many of the essential questions remain unanswered. While we do know the current three vaccines are highly protective against severe disease and death, and there is some evidence that these vaccinations do reduce infections and virus transmission of SARS-CoV-2, we do not yet know the full degree to which this occurs.
For example, we know there have been some cases of people that have been infected in close proximity to getting their full vaccination and rare cases of breakthrough reinfections. A breakthrough infection in a restaurant is a challenge for contact tracing, but an outbreak from a movie theater exposure or a baseball game could spark a major outbreak at our current level of vaccination. Current CDC guidance recommends continued mask wearing in order to address these concerns.
We also do not yet know how long the protections will last and if or when a booster or revaccination is required. In effect, it is too soon to know. Should an annual booster shot be required, then a vaccine passport would require annual updating, a process more frequent than renewal of a driver's license.
We also know that the current SARS-CoV-2 virus is mutating briskly. While the current approved vaccines have remained effective overall, there is evidence of some degree of degradation in vaccine effectiveness against some of the circulating strains. We also have sparse data on many of the other emerging strains of concern because we have not had the surveillance capacity in the U.S. to gain an adequate sense of how the virus is changing to fully align vaccine effectiveness with viral capabilities.
The risk of people misusing these "passports" is troubling. The potential for using these documents for hiring, firing or job limitation is a serious concern. Unvaccinated workers are at risk of this form of discrimination even from well-meaning employers or supervisors. Health insurers are prohibited by the Affordable Care Act from discriminating based on preexisting conditions, but they could probably charge a higher premium for unvaccinated individuals. There also is a risk of stigmatizing individuals who are not vaccinated or have left their vaccine documentation at home. Another concern: the opportunity to discriminate based on race, gender, sexual orientation, or religion, using one's vaccination status as an excuse.
These "passports" are being discussed as a "ticket verification" for entry to many activities, including dining at restaurants, flying domestically and/or internationally, going to movie theaters and sporting events, etc. These are all activities we already are doing at reduced levels and for which wearing a mask, hand hygiene and physical distancing are effective disease control practices. COVID-19 vaccines are indeed the measure that will make the ability to totally reopen our society complete, but we are not there yet. Documentation of one's COVID-19 vaccine status may be useful in selected situations in the future. That remains to be seen.
Finally, inadequate vaccine supply and disparities in vaccine delivery have created enormous challenges in providing equal access to vaccination. Also, the amount of misinformation, disinformation, and lingering vaccine hesitancy continue to limit the speed at which we will reach the level of vaccination of the population that would make this documentation meaningful. The requirement for "vaccine passports" is already alienating people who are opposed to vaccinations for a variety of reasons, paradoxically risking reduced vaccine uptake. This politicization of the vaccination effort is of concern. There are indeed people who, due to medical contraindications or legal exemptions, will not be vaccinated, and we do not yet have a national framework on how to address this.
Vaccine passports are not the solution for reopening our society — a robust vaccination program is. The requirement to document one's vaccination status for COVID-19 may one day have its place. For now, it is an idea whose time has not yet come.
Editor's Note: This op/ed is part of a "Big Question" series on the ethics of vaccine passports. Read the flip side argument here.
A digital health passport required by businesses and universities could help us get back to normal more quickly, one expert argues.
"Vaccine passports" are a system that requires proof of a COVID-19 vaccination as a condition of engaging in activities that pose a risk of transmitted SARS-CoV-2. Digital Health Passes (DHPs) are typically a smartphone application with a code that verifies whether someone has been vaccinated.
Vaccine passports could very much be in our future. Many businesses are implementing or planning to require proof of vaccination as a condition of returning to the workplace. Colleges and universities have announced vaccine requirements for students, staff, and faculty. It may not be long before the private sector requires a vaccination card or image to attend an entertainment or sporting event, to travel, or even to dine or shop indoors, at least in some venues.
But it's unlikely the federal government or the states will launch DHPs, at least not in the near-term. President Biden announced the White House has no intention of requiring proof of vaccination. While no state has mandated DHPs, New York is piloting its Excelsior Pass on a voluntary basis, partnering with IBM. Other nations are not so hesitant. Israel's "Green Pass" has gotten the nation back to normal in record time. And various countries and regions are planning DHPs, including the European Union and the United Kingdom. Foreign airlines are likely to require proof of vaccination as a condition of flying internationally.
DHPs could emerge as a way to get us back to normal more quickly, but are they ethical? Let's start with the law. The US Equal Opportunity Commission (EEOC) has specifically said that employers have the legal right to require proof of vaccination as a condition of returning to work. Colleges and universities already require several vaccines for students living in dorms. Hospitals and nursing homes often mandate influenza vaccinations. And, of course, all states require childhood vaccinations for school attendance. Vaccine passports are lawful but are they ethical? The short answer is "yes" but only if we ensure no one is left behind.
Vaccine passports "don't force anyone to be vaccinated against his or her will. They simply say to individuals that if you choose not to be vaccinated, you can't work or recreate in public spaces that risk transmission of the virus."
Why are vaccine passports ethical? Vaccines are a miracle of modern science, but they have become a political symbol, and a significant part of the population doesn't want to get a jab. The rare cases of blood clots associated with the Johnson & Johnson and AstraZeneca vaccines have only created more distrust.
Most opposition to vaccine passports hinges on the claim that they infringe personal autonomy and liberty. But this argument misses the point. Of course, every competent adult has the right to make decisions that affect his or her own health and safety. But no one has a right to infringe on the rights of others, such as by exposing them to a potentially serious or deadly infectious disease. An individual can't claim the right to attend a crowded event mask-less and unvaccinated. This was once accepted across the political spectrum. Conservative economists called it an "externality," that is a person has no right to harm others. The U.S. has lost the tradition of the common good. We have become so focused on our own individual rights that we forget about our ethical obligations to our neighbors and to our community.
In fact, DHPs actually don't force anyone to be vaccinated against his or her will. They simply say to individuals that if you choose not to be vaccinated, you can't work or recreate in public spaces that risk transmission of the virus.
DHPs also don't infringe on privacy. Again, everyone has the choice whether to show proof of vaccination. It isn't required. Moreover, DHPs may actually protect privacy because all they do is show whether or not you have been vaccinated. They don't disclose any other personal medical information. All of us actually have already had to show proof of vaccination as a condition of going to school. Thus, DHPs are well established in the United States.
But there is one ethical argument against DHPs that I find to be powerful, and that is equity. If we require proof of vaccination while doses are scarce, we will give the already privileged even more privilege. And that would be unconscionable. Thus, DHPs should not be implemented until everyone who wants a vaccine is able to get a vaccine. Equity isn't a side issue. It needs to be front and center.
As of today, all adults in the U.S. are eligible to get vaccinated, and President Biden has pledged that by the end of May there will be enough doses to vaccinate the entire U.S. population. It is a realistic promise. Once vaccines become plentiful, everyone should get their shot. All Food and Drug Administration authorized vaccines are highly safe and effective, even the Johnson & Johnson vaccine that the FDA has just put on pause.
Businesses have an economic incentive to require proof of vaccination. Very few of us would feel comfortable returning to our jobs, shops, theaters, or restaurants unless we feel safe. Businesses understand the duty to create safer places for work, recreation, and commerce.
One question has dominated national conversation since the pandemic began. "When will we get back to normal?" There is a deep human yearning to hug family and friends, see our work colleagues, recreate, and be entertained. One day we will have defeated this wily virus and get back to normal. But vaccine passports can help us get back to the things we love faster and more safely. As long as we don't leave anyone behind, using this miracle of modern science to make our lives better is both lawful and ethical.
Editor's Note: This op/ed is part of a "Big Question" series on the ethics of vaccine passports. Read the flip-side argument here.

