How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
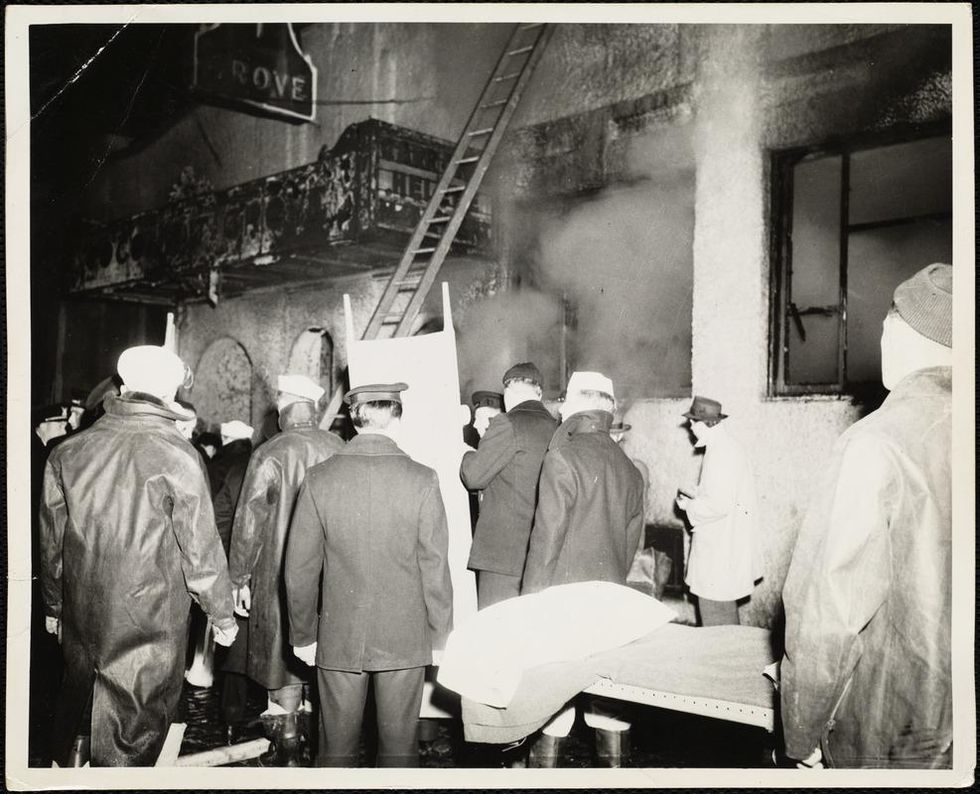
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
The Pandemic Is Ushering in a More Modern—and Ethical—Way of Studying New Drugs and Diseases
Miniature lab-grown models of human organs have major advantages over standard animal testing.
Before the onset of the coronavirus pandemic, Dutch doctoral researcher Joep Beumer had used miniature lab-grown organs to study the human intestine as part of his PhD thesis. When lockdown hit, however, he was forced to delay his plans for graduation. Overwhelmed by a sense of boredom after the closure of his lab at the Hubrecht Institute, in the Netherlands, he began reading literature related to COVID-19.
"By February [2020], there were already reports on coronavirus symptoms in the intestinal tract," Beumer says, adding that this piqued his interest. He wondered if he could use his miniature models – called organoids -- to study how the coronavirus infects the intestines.
But he wasn't the only one to follow this train of thought. In the year since the pandemic began, many researchers have been using organoids to study how the coronavirus infects human cells, and find potential treatments. Beumer's pivot represents a remarkable and fast-emerging paradigm shift in how drugs and diseases will be studied in the coming decades. With future pandemics likely to be more frequent and deadlier, such a shift is necessary to reduce the average clinical development time of 5.9 years for antiviral agents.
Part of that shift means developing models that replicate human biology in the lab. Animal models, which are the current standard in biomedical research, fail to do so—96% of drugs that pass animal testing, for example, fail to make it to market. Injecting potentially toxic drugs into living creatures, before eventually slaughtering them, also raises ethical concerns for some. Organoids, on the other hand, respond to infectious diseases, or potential treatments, in a way that is relevant to humans, in addition to being slaughter-free.

Human intestinal organoids infected with SARS-CoV-2 (white).
Credit: Joep Beumer/Clevers group/Hubrecht Institute
Urgency Sparked Momentum
Though brain organoids were previously used to study the Zika virus during the 2015-16 epidemic, it wasn't until COVID-19 that the field really started to change. "The organoid field has advanced a lot in the last year. The speed at which it happened is crazy," says Shuibing Chen, an associate professor at Weill Cornell Medicine in New York. She adds that many federal and private funding agencies have now seen the benefits of organoids, and are starting to appreciate their potential in the biomedical field.
Last summer, the Organo-Strat (OS) network—a German network that uses human organoid models to study COVID-19's effects—received 3.2 million euros in funding from the German government. "When the pandemic started, we became aware that we didn't have the right models to immediately investigate the effects of the virus," says Andreas Hocke, professor of infectious diseases at the Charité Universitätsmedizin in Berlin, Germany, and coordinator of the OS network. Hocke explained that while the World Health Organization's animal models showed an "overlap of symptoms'' with humans, there was "no clear reflection" of the same disease.
"The network functions as a way of connecting organoid experts with infectious disease experts across Germany," Hocke continues. "Having organoid models on demand means we can understand how a virus infects human cells from the first moment it's isolated." Overall, OS aims to create infrastructure that could be applied to future pandemics. There are 28 sub-projects involved in the network, covering a wide assortment of individual organoids.
Cost, however, remains an obstacle to scaling up, says Chen. She says there is also a limit to what we can learn from organoids, given that they only represent a single organ. "We can add drugs to organoids to see how the cells respond, but these tests don't tell us anything about drug metabolism, for example," she explains.
A Related "Leaps" in Progress
One way to solve this issue is to use an organ-on-a-chip system. These are miniature chips containing a variety of human cells, as well as small channels along which functions like blood or air flow can be recreated. This allows scientists to perform more complex experiments, like studying drug metabolism, while producing results that are relevant to humans.

An organ-on-a-chip system.
Credit: Fraunhofer IGB
Such systems are also able to elicit an immune response. The FDA has even entered into an agreement with Wyss Institute spinoff Emulate to use their lung-on-a-chip system to test COVID-19 vaccines. Representing multiple organs in one system is also possible. Berlin-based TissUse are aiming to make a so-called 'human on a chip' system commercially available. But TissUse senior scientist Ilka Maschmeyer warns that there is a limit to how far the technology can go. "The system will not think or feel, so it wouldn't be possible to test for illnesses affecting these abilities," she says.
Some challenges also remain in the usability of organs-on-a-chip. "Specialized training is required to use them as they are so complex," says Peter Loskill, assistant professor and head of the organ-on-a-chip group at the University of Tübingen, Germany. Hocke agrees with this. "Cell culture scientists would easily understand how to use organoids in a lab, but when using a chip, you need additional biotechnology knowledge," he says.
One major advantage of both technologies is the possibility of personalized medicine: Cells can be taken from a patient and put onto a chip, for example, to test their individual response to a treatment. Loskill also says there are other uses outside of the biomedical field, such as cosmetic and chemical testing.
"Although these technologies offer a lot of possibilities, they need time to develop," Loskill continues. He stresses, however, that it's not just the technology that needs to change. "There's a lot of conservative thinking in biomedical research that says this is how we've always done things. To really study human biology means approaching research questions in a completely new way."
Even so, he thinks that the pandemic marked a shift in people's thinking—no one cared how the results were found, as long as it was done quickly. But Loskill adds that it's important to balance promise, potential, and expectations when it comes to these new models. "Maybe in 15 years' time we will have a limited number of animal models in comparison to now, but the timescale depends on many factors," he says.
Beumer, now a post-doc, was eventually allowed to return to the lab to develop his coronavirus model, and found working on it to be an eye-opening experience. He saw first-hand how his research could have an impact on something that was affecting the entire human race, as well as the pressure that comes with studying potential treatments. Though he doesn't see a future for himself in infectious diseases, he hopes to stick with organoids. "I've now gotten really excited about the prospect of using organoids for drug discovery," he says.
The coronavirus pandemic has slowed society down in many respects, but it has flung biomedical research into the future—from mRNA vaccines to healthcare models based on human biology. It may be difficult to fully eradicate animal models, but over the coming years, organoids and organs-on-a-chip may become the standard for the sake of efficacy -- and ethics.
Jack McGovan is a freelance science writer based in Berlin. His main interests center around sustainability, food, and the multitude of ways in which the human world intersects with animal life. Find him on Twitter @jack_mcgovan."
New Podcast: Why Dr. Ashish Jha Expects a Good Summer
Dr. Jha discusses Covid vaccine passports, how supply and demand of the vaccines is about to shift, the AstraZeneca situation, what's new with kids, herd immunity, and more.
Making Sense of Science features interviews with leading medical and scientific experts about the latest developments and the big ethical and societal questions they raise. This monthly podcast is hosted by journalist Kira Peikoff, founding editor of the award-winning science outlet Leaps.org.
Hear the 30-second trailer:
Listen to the whole episode: "Why Dr. Ashish Jha Expects a Good Summer"
Dr. Ashish Jha, dean of public health at Brown University, discusses the latest developments around the Covid-19 vaccines, including supply and demand, herd immunity, kids, vaccine passports, and why he expects the summer to look very good.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.