How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
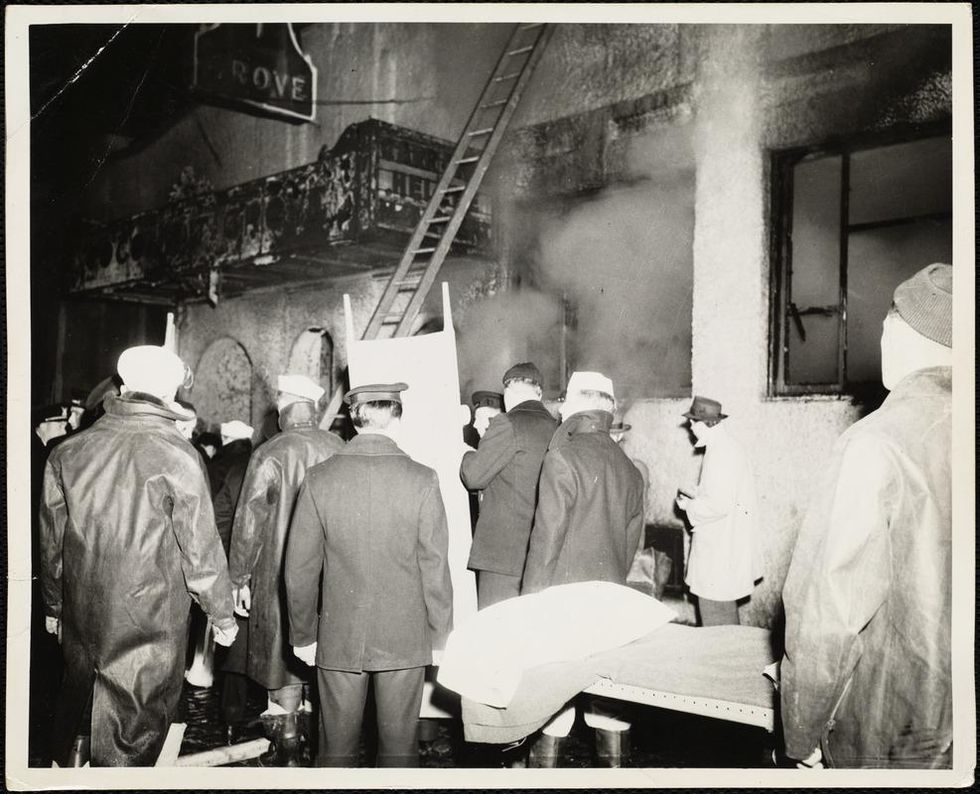
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
World’s First “Augmented Reality” Contact Lens Aims to Revolutionize Much More Than Medicine
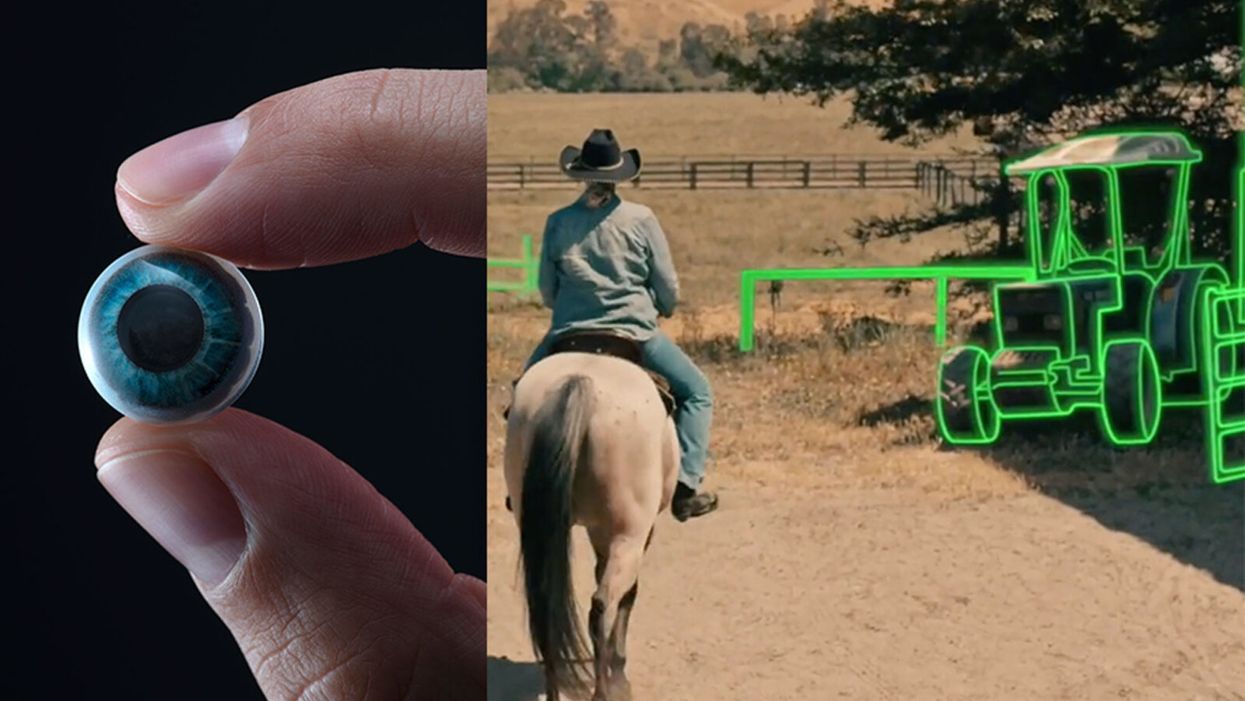
On the left, a picture of the Mojo lens smart contact; and a simulated image of a woman with low vision who is wearing the contact to highlight objects in her field of vision.
Imagine a world without screens. Instead of endlessly staring at your computer or craning your neck down to scroll through social media feeds and emails, information simply appears in front of your eyes when you need it and disappears when you don't.
"The vision is super clear...I was reading the poem with my eyes closed."
No more rude interruptions during dinner, no more bumping into people on the street while trying to follow GPS directions — just the information you want, when you need it, projected directly onto your visual field.
While this screenless future sounds like science fiction, it may soon be a reality thanks to the new Silicon Valley startup Mojo Vision, creator of the world's first smart contact lens. With a 14,000 pixel-per-inch display with eye-tracking, image stabilization, and a custom wireless radio, the Mojo smart lens bills itself the "smallest and densest dynamic display ever made." Unlike current augmented reality wearables such as Google Glass or ThirdEye, which project images onto a glass screen, the Mojo smart lens can project images directly onto the retina.
A current prototype displayed at the Consumer Electronics Show earlier this year in Las Vegas includes a tiny screen positioned right above the most sensitive area of the pupil. "[The Mojo lens] is a contact lens that essentially has wireless power and data transmission for a small micro LED projector that is placed over the center of the eye," explains David Hobbs, Director of Product Management at Mojo Vision. "[It] displays critical heads-up information when you need it and fades into the background when you're ready to continue on with your day."
Eventually, Mojo Visions' technology could replace our beloved smart devices but the first generation of the Mojo smart lens will be used to help the 2.2 billion people globally who suffer from vision impairment.
"If you think of the eye as a camera [for the visually impaired], the sensors are not working properly," explains Dr. Ashley Tuan, Vice President of Medical Devices at Mojo Vision and fellow of the American Academy of Optometry. "For this population, our lens can process the image so the contrast can be enhanced, we can make the image larger, magnify it so that low-vision people can see it or we can make it smaller so they can check their environment." In January of this year, the FDA granted Breakthrough Device Designation to Mojo, allowing them to have early and frequent discussions with the FDA about technical, safety and efficacy topics before clinical trials can be done and certification granted.
For now, Dr. Tuan is one of the few people who has actually worn the Mojo lens. "I put the contact lens on my eye. It was very comfortable like any contact lenses I've worn before," she describes. "The vision is super clear and then when I put on the accessories, suddenly I see Yoda in front of me and I see my vital signs. And then I have my colleague that prepared a beautiful poem that I loved when I was young [and] I was reading the poem with my eyes closed."
At the moment, there are several electronic glasses on the market like Acesight and Nueyes Pro that provide similar solutions for those suffering from visual impairment, but they are large, cumbersome, and highly visible. Mojo lens would be a discreet, more comfortable alternative that offers users more freedom of movement and independence.
"In the case of augmented-reality contact lenses, there could be an opportunity to improve the lives of people with low vision," says Dr. Thomas Steinemann, spokesperson for the American Academy of Ophthalmology and professor of ophthalmology at MetroHealth Medical Center in Cleveland. "There are existing tools for people currently living with low vision—such as digital apps, magnifiers, etc.— but something wearable could provide more flexibility and significantly more aid in day-to-day tasks."
As one of the first examples of "invisible computing," the potential applications of Mojo lens in the medical field are endless.
According to Dr. Tuan, the visually impaired often suffer from depression due to their lack of mobility and 70 percent of them are underemployed. "We hope that they can use this device to gain their mobility so they can get that social aspect back in their lives and then, eventually, employment," she explains. "That is our first and most important goal."
But helping those with low visual capabilities is only Mojo lens' first possible medical application; augmented reality is already being used in medicine and is poised to revolutionize the field in the coming decades. For example, Accuvein, a device that uses lasers to provide real-time images of veins, is widely used by nurses and doctors to help with the insertion of needles for IVs and blood tests.
According to the National Center for Biotechnology Information, augmentation of reality has been used in surgery for many years with surgeons using devices such as Google Glass to overlay critical information about their patients into their visual field. Using software like the Holographic Navigation Platform by Scopsis, surgeons can see a mixed-reality overlay that can "show you complicated tumor boundaries, assist with implant placements and guide you along anatomical pathways," its developers say.
However, according to Dr. Tuan, augmented reality headsets have drawbacks in the surgical setting. "The advantage of [Mojo lens] is you don't need to worry about sweating or that the headset or glasses will slide down to your nose," she explains "Also, our lens is designed so that it will understand your intent, so when you don't want the image overlay it will disappear, it will not block your visual field, and when you need it, it will come back at the right time."
As one of the first examples of "invisible computing," the potential applications of Mojo lens in the medical field are endless. Possibilities include live translation of sign language for deaf people; helping those with autism to read emotions; and improving doctors' bedside manner by allowing them to fully engage with patients without relying on a computer.
"[By] monitoring those blood vessels we can [track] chronic disease progression: high blood pressure, diabetes, and Alzheimer's."
Furthermore, the lens could be used to monitor health issues. "We have image sensors in the lens right now that point to the world but we can have a camera pointing inside of your eye to your retina," says Dr. Tuan, "[By] monitoring those blood vessels we can [track] chronic disease progression: high blood pressure, diabetes, and Alzheimer's."
For the moment, the future medical applications of the Mojo lens are still theoretical, but the team is confident they can eventually become a reality after going through the proper regulatory review. The company is still in the process of design, prototype and testing of the lens, so they don't know exactly when it will be available for use, but they anticipate shipping the first available products in the next couple of years. Once it does go to market, it will be available by prescription only for those with visual impairments, but the team's goal is to bring it to broader consumer markets pending regulatory clearance.
"We see that right now there's a unique opportunity here for Mojo lens and invisible computing to help to shape what the next decade of technology development looks like," explains David Hobbs. "We can use [the Mojo lens] to better serve us as opposed to us serving technology better."
Schmidt Ocean Institute co-founder Wendy Schmidt is backed by 32 screens in research vessel Falkor's control room where most of the science takes place on the ship, from mapping to live streaming of underwater robotic dives.
WENDY SCHMIDT is a philanthropist and investor who has spent more than a dozen years creating innovative non-profit organizations to solve pressing global environmental and human rights issues. Recognizing the human dependence on sustaining and protecting our planet and its people, Wendy has built organizations that work to educate and advance an understanding of the critical interconnectivity between the land and the sea. Through a combination of grants and investments, Wendy's philanthropic work supports research and science, community organizations, promising leaders, and the development of innovative technologies. Wendy is president of The Schmidt Family Foundation, which she co-founded with her husband Eric in 2006. They also co-founded Schmidt Ocean Institute and Schmidt Futures.
Editors: The pandemic has altered the course of human history and the nature of our daily lives in equal measure. How has it affected the focus of your philanthropy across your organizations? Have any aspects of the crisis in particular been especially galvanizing as you considered where to concentrate your efforts?
Wendy: The COVID-19 pandemic has made the work of our philanthropy more relevant than ever. If anything, the circumstances of this time have validated the focus we have had for nearly 15 years. We support the need for universal access to clean, renewable energy, healthy food systems, and the dignity of human labor and self-determination in a world of interconnected living systems on land and in the Ocean we are only beginning to understand.
When you consider the disproportionate impact of the COVID-19 virus on people who are poorly paid, poorly housed, with poor nutrition and health care, and exposed to unsafe conditions in the workplace—you see clearly how the systems that have been defining how we live, what we eat, who gets healthcare and what impacts the environment around us—need to change.
"This moment has propelled broad movements toward open publication and open sharing of data and samples—something that has always been a core belief in how we support and advance science."
If the pandemic teaches us anything, we learn what resilience looks like, and the essential role for local small businesses including restaurants, farms and ranches, dairies and fish markets in the long term vitality of communities. There is resonance, local economic benefit, and also accountability in these smaller systems, with shorter supply chains and less vertical integration.
The consolidation of vertically integrated business operations for the sake of global efficiency reveals its essential weakness when supply chains break down and the failure to encourage local economic centers leads to intense systemic disruption and the possibility of collapse.
Editors: For scientists, one significant challenge has been figuring out how to continue research, if at all, during this time of isolation and distancing. Yet, your research vessel Falkor, of the Schmidt Ocean Institute, is still on its expedition exploring the Coral Sea Marine Park in Australia—except now there are no scientists onboard. What was the vessel up to before the pandemic hit? Can you tell us more about how they are continuing to conduct research from afar now and how that's going?
Wendy: We have been extremely fortunate at Schmidt Ocean Institute. When the pandemic hit in March, our research vessel, Falkor, was already months into a year-long program to research unexplored deep sea canyons around Australia and at the Great Barrier Reef. We were at sea, with an Australian science group aboard, carrying on with our mission of exploration, discovery and communication, when we happened upon what we believe to be the world's longest animal—a siphonophore about 150 feet long, spiraling out at a depth of about 2100 feet at the end of a deeper dive in the Ningaloo Canyon off Western Australia. It was the kind of wondrous creature we find so often when we conduct ROV dives in the world's Ocean.
For more than two months this year, Falkor was reportedly the only research vessel in the world carrying on active research at sea. Once we were able to dock and return the science party to shore, we resumed our program at sea offering a scheduled set of now land-based scientists in lockdown in Australia the opportunity to conduct research remotely, taking advantage of the vessel's ship to shore communications, high resolution cameras and live streaming video. It's a whole new world, and quite wonderful in its own way.
Editors: Normally, 10–15 scientists would be aboard such a vessel. Is "remote research" via advanced video technology here to stay? Are there any upsides to this "new normal"?
Wendy: Like all things pandemic, remote research is an adaptation for what would normally occur. Since we are putting safety of the crew and guest scientists at the forefront, we're working to build strong remote connections between our crew, land based scientists and the many robotic tools on board Falkor. There's no substitute for in person work, but what we've developed during the current cruise is a pretty good and productive alternative in a crisis. And what's important is that this critical scientific research into the deep sea is able to continue, despite the pandemic on land.
Editors: Speaking of marine expeditions, you've sponsored two XPRIZE competitions focused on ocean health. Do you think challenge prizes could fill gaps of the global COVID-19 response, for example, to manufacture more testing kits, accelerate the delivery of PPE, or incentivize other areas of need?
Wendy: One challenge we are currently facing is that innovations don't have the funding pathway to scale, so promising ideas by entrepreneurs, researchers, and even major companies are being developed too slowly. Challenge prizes help raise awareness for problems we are trying to solve and attract new people to help solve those problems by giving them a pathway to contribute.
One idea might be for philanthropy to pair prizes and challenges with an "advanced market commitment" where the government commits to a purchase order for the innovation if it meets a certain test. That could be deeply impactful for areas like PPE and the production of testing kits.
Editors: COVID-19 testing, especially, has been sorely needed, here in the U.S. and in developing countries as well as low-income communities. That's why we're so intrigued by your Schmidt Science Fellows grantee Hal Holmes and his work to repurpose a new DNA technology to create a portable, mobile test for COVID-19. Can you tell us about that work and how you are supporting it?
Wendy: Our work with Conservation X Labs began years ago when our foundation was the first to support their efforts to develop a handheld DNA barcode sensor to help detect illegally imported and mislabeled seafood and timber products. The device was developed by Hal Holmes, who became one of our Schmidt Science Fellows and is the technical lead on the project, working closely with Conservation X Labs co-founders Alex Deghan and Paul Bunje. Now, with COVID-19, Hal and team have worked with another Schmidt Science Fellow, Fahim Farzardfard, to repurpose the technology—which requires no continuous power source, special training, or a lab—to serve as a mobile testing device for the virus.
The work is going very well, manufacturing is being organized, and distribution agreements with hospitals and government agencies are underway. You could see this device in use within a few months and have testing results within hours instead of days. It could be especially useful in low-income communities and developing countries where access to testing is challenging.
Editors: How is Schmidt Futures involved in the development of information platforms that will offer productive solutions?
Wendy: In addition to the work I've mentioned, we've also funded the development of tech-enabled tools that can help the medical community be better prepared for the ongoing spike of COVID cases. For example, we funded EdX and Learning Agency to develop an online training to help increase the number of medical professionals who can operate ventilators. The first course is being offered by Harvard University, and so far, over 220,000 medical professionals have enrolled. We have also invested in informational platforms that make it easier to contain the spread of the disease, such as our work with Recidiviz to model the impact of COVID-19 in prisons and outline policy steps states could take to limit the spread.
Information platforms can also play a big part pushing forward scientific research into the virus. For example, we've funded the UC Santa Cruz Virus Browser, which allows researchers to examine each piece of the virus and see the proteins it creates, the interactions in the host cell, and — most importantly — almost everything the recent scientific literature has to say about that stretch of the molecule.
Editors: The scale of research collaboration and the speed of innovation today seem unprecedented. The whole science world has turned its attention to combating the pandemic. What positive big-picture trends do you think or hope will persist once the crisis eventually abates?
Wendy: As in many areas, the COVID crisis has accelerated trends in the scientific world that were already well underway. For instance, this moment has propelled broad movements toward open publication and open sharing of data and samples—something that has always been a core belief in how we support and advance science.
We believe collaboration is an essential ingredient for progress in all areas. Early in this pandemic, Schmidt Futures held a virtual gathering of 160 people across 70 organizations in philanthropy, government, and business interested in accelerating research and response to the virus, and thought at the time, it's pretty amazing this kind of thing doesn't go all the time. We are obviously going to go farther together than on our own...
My husband, Eric, has observed that in the past two months, we've all catapulted 10 years forward in our use of technology, so there are trends already underway that are likely accelerated and will become part of the fabric of the post-COVID world—like working remotely; online learning; increased online shopping, even for groceries; telemedicine; increasing use of AI to create smarter delivery systems for healthcare and many other applications in a world that has grown more virtual overnight.
"Our deepest hope is that out of these alarming and uncertain times will come a renewed appreciation for the tools of science, as they help humans to navigate a world of interconnected living systems, of which viruses are a large part."
We fully expect these trends to continue and expand across the sciences, sped up by the pressures of the health crisis. Schmidt Ocean Institute and Schmidt Futures have been pressing in these directions for years, so we are pleased to see the expansions that should help more scientists work productively, together.
Editors: Trying to find the good amid a horrible crisis, are there any other new horizons in science, philanthropy, and/or your own work that could transform our world for the better that you'd like to share?
Wendy: Our deepest hope is that out of these alarming and uncertain times will come a renewed appreciation for the tools of science, as they help humans to navigate a world of interconnected living systems, of which viruses are a large part. The more we investigate the Ocean, the more we look deeply into what lies in our soils and beneath them, the more we realize we do not know, and moreover, how vulnerable humanity is to the forces of the natural world.
Philanthropy has an important role to play in influencing how people perceive our place in the world and understand the impact of human activity on the rest of the planet. I believe it's philanthropy's role to take risks, to invest early in innovative technologies, to lead where governments and industry aren't ready to go yet. We're fortunate at this time to be able to help those working on tools to better diagnose and treat the virus, and to invest in those working to improve information systems, so citizens and policy makers can make better decisions that can reduce impacts on families and institutions.
From all we know, this isn't likely to be the last pandemic the world will see. It's been said that a crisis comes before change, and we would hope that we can play a role in furthering the work to build systems that are resilient—in information, energy, agriculture and in all the ways we work, recreate, and use the precious resources of our planet.
[This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.