How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
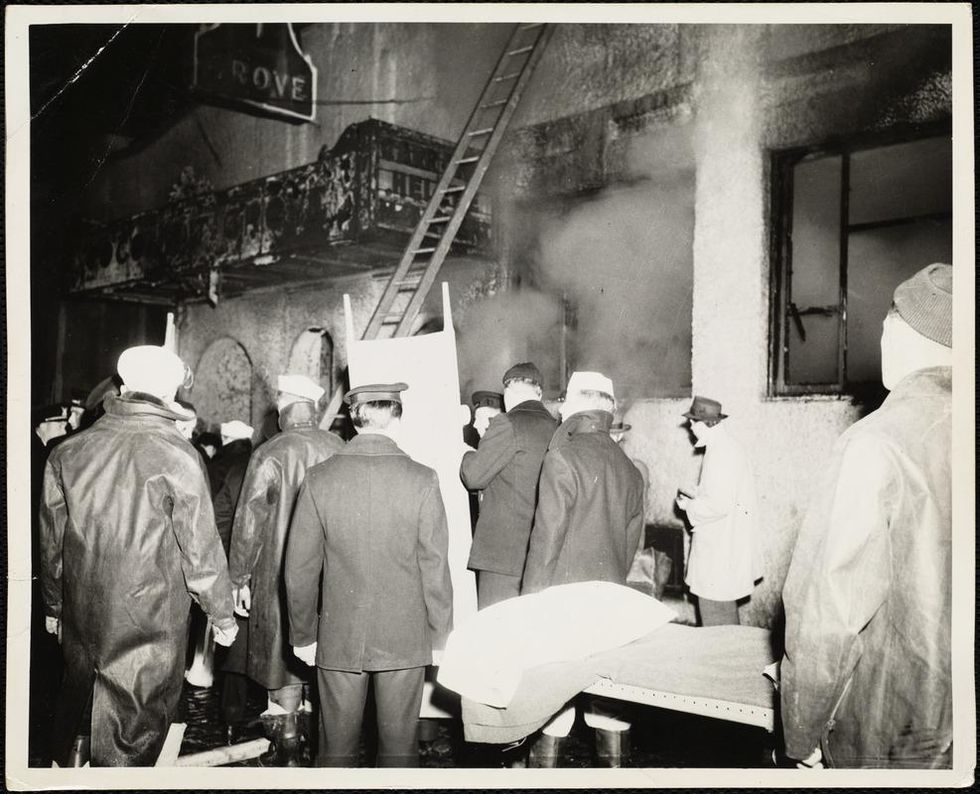
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
“Disinfection Tunnels” Are Popping Up Around the World, Fueled By Misinformation and Fear
A screenshot of a video published by The Guardian of a tunnel used in a Mexican border town to "disinfect" U.S. visitors in an attempt to prevent them from spreading the coronavirus.
In an incident that sparked widespread outrage across India in late March, officials in the north Indian state of Uttar Pradesh sprayed hundreds of migrant workers, including women and children, with a chemical solution to sanitize them, in a misguided attempt to contain the spread of the novel coronavirus.
Since COVID-19 is a respiratory disorder, disinfecting a person's body or clothes cannot protect them from contracting the novel coronavirus, or help in containing the pathogen's spread.
Health officials reportedly doused the group with a diluted mixture of sodium hypochlorite – a bleaching agent harmful to humans, which led to complaints of skin rashes and eye irritation. The opposition termed the instance 'inhuman', compelling the state government to order an investigation into the mass 'chemical bath.'
"I don't think the officials thought this through," says Thomas Abraham, a professor with The University of Hong Kong, and a former consultant for the World Health Organisation (WHO) on risk communication. "Spraying people with bleach can prove to be harmful, and there is no guideline … that recommends it. This was some sort of a kneejerk reaction."
Although spraying individuals with chemicals led to a furor in the South Asian nation owing to its potential dangers, so-called "disinfection tunnels" have sprung up in crowded public places around the world, including malls, offices, airports, railway stations and markets. Touted as mass disinfectants, these tunnels spray individuals with chemical disinfectant liquids, mists or fumes through nozzles for a few seconds, purportedly to sanitize them -- though experts strongly condemn their use. The tunnels have appeared in at least 16 countries: India, Malaysia, Scotland, Albania, Argentina, Colombia, Singapore, China, Pakistan, France, Vietnam, Bosnia and Herzegovina, Chile, Mexico, Sri Lanka and Indonesia. Russian President Vladimir Putin even reportedly has his own tunnel at his residence.
While U.S. visitors to Mexico are "disinfected" through these sanitizing tunnels, there is no evidence that the mechanism is currently in use within the United States. However, the situation could rapidly change with international innovators like RD Pack, an Israeli start-up, pushing for their deployment. Many American and multinational companies like Stretch Structures, Guilio Barbieri and Inflatable Design Works are also producing these systems. As countries gradually ease lockdown restrictions, their demand is on the rise -- despite a stringent warning from the WHO against their potential health hazards.
"Spraying individuals with disinfectants (such as in a tunnel, cabinet, or chamber) is not recommended under any circumstances," the WHO warned in a report on May 15. "This could be physically and psychologically harmful and would not reduce an infected person's ability to spread the virus through droplets or contact. Moreover, spraying individuals with chlorine and other toxic chemicals could result in eye and skin irritation, bronchospasm due to inhalation, and gastrointestinal effects such as nausea and vomiting."
Disinfection tunnels largely spray a diluted mixture of sodium hypochlorite, a chlorine compound commonly known as bleach, often used to disinfect inanimate surfaces. Known for its hazardous properties, the WHO, in a separate advisory on COVID-19, warns that spraying bleach or any other disinfectant on individuals can prove to be poisonous if ingested, and that such substances should be used only to disinfect surfaces.
Considering the effect of sodium hypochlorite on mucous membranes, the European Centre for Disease Prevention and Control, an EU agency focussed on infectious diseases, recommends limited use of the chemical compound even when disinfecting surfaces – only 0.05 percent for cleaning surfaces, and 0.1 percent for toilets and bathroom sinks. The Indian health ministry also cautioned against spraying sodium hypochlorite recently, stating that its inhalation can lead to irritation of mucous membranes of the nose, throat, and respiratory tract.
In addition to the health hazards that such sterilizing systems pose, they have little utility, argues Indian virologist T. Jacob John. Since COVID-19 is a respiratory disorder, disinfecting a person's body or clothes cannot protect them from contracting the novel coronavirus, or help in containing the pathogen's spread.
"It's a respiratory infection, which means that you have the virus in your respiratory tract, and of course, that shows in your throat, therefore saliva, etc.," says John. "The virus does not survive outside the body for a long time, unless it is in freezing temperatures. Disinfecting a person's clothes or their body makes no sense."
Disinfection tunnels have limited, if any, impact on the main modes of coronavirus transmission, adds Craig Janes, director, School of Public Health and Health Systems at Canada's University of Waterloo. He explains that the nature of COVID-19 transmission is primarily from person-to-person, either directly, or via an object that is shared between two individuals. Measures like physical distancing and handwashing take care of these transmission risks.
"My view of these kinds of actions are that they are principally symbolic, indicating to a concerned population that 'something is being done,' to martial support for government or health system efforts," says Janes. "So perhaps a psychological benefit, but I'm not sure that this benefit would outweigh the risks."
"They may make people feel that their risk of infection has been reduced, and also that they do not have to worry about infecting others."
A recent report by Health Care Without Harm (HCWH), an international not-for-profit organization focused on sustainable health care around the world, states that disinfection tunnels have little evidence to demonstrate their efficacy or safety.
"If the goal is to reduce the spread of the virus by decontaminating the exterior clothing, shoes, and skin of the general public, there is no evidence that clothes are an important vector for transmission. If the goal is to attack the virus in the airways, what is the evidence that a 20-30 second external application is efficacious and safe?" the report questions. "The World Health Organization recommends more direct and effective ways to address hand hygiene, with interventions known to be effective."
If an infected person walks through a disinfection tunnel, he would still be infectious, as the chemicals will only disinfect the surfaces, says Gerald Keusch, a professor of medicine and international health at Boston University's Schools of Medicine and Public Health.
"While we know that viruses can be "disinfected" from surfaces and hands, disinfectants can be harmful to health if ingested or inhaled. The underlying principle of medicine is to do no harm, and we always measure benefit against risk when approving interventions. I don't know if this has been followed and assessed with respect to these devices," says Keusch. "It's a really bad idea."
Experts warn that such tunnels may also create a false sense of security, discouraging people from adopting best practice methods like handwashing, social distancing, avoiding crowded places, and using masks to combat the spread of COVID-19.
"They may make people feel that their risk of infection has been reduced, and also that they do not have to worry about infecting others," says Janes. "These are false assumptions, and may lead to increasing rather than reducing transmission."
n artist rendering of a "smart toilet" that gathers biometric data to monitor a person's health in real time.
It looks like an ordinary toilet but it is anything but. The "smart toilet" is the diagnostic tool of the future, equipped with cameras that take snapshots of the users and their waste, motion sensors to analyze what's inside the urine and stool samples, and software that automatically sends data to a secure, cloud-based system that can be easily accessed by your family doctor.
"It's a way of doing community surveillance. If there is a second wave of infections in the future, we'll know right away."
Using urine "dipstick tests" similar to the home pregnancy strips, the smart toilet can detect certain proteins, immune system biomarkers and blood cells that indicate the presence of such diseases as infections, bladder cancer, and kidney failure.
The rationale behind this invention is that some of the best ways of detecting what's going on in our bodies is by analyzing the substances we excrete every day, our sweat, urine, saliva and yes, our feces. Instead of getting sporadic snapshots from doctor's visits once or twice a year, the smart toilet provides continuous monitoring of our health 24/7, so we can catch the tell-tale molecular signature of illnesses at their earliest and most treatable stages. A brainchild of Stanford University researchers, they're now working to add a COVID-19 detection component to their suite of technologies—corona virus particles can be spotted in stool samples—and hope to have the system available within the year.
"We can connect the toilet system to cell phones so we'll know the results within 30 minutes," says Seung-min Park, a lead investigator on the research team that devised this technology and a senior research scientist at the Stanford University School of Medicine. "The beauty of this technology is that it can continuously monitor even after this pandemic is over. It's a way of doing community surveillance. If there is a second wave of infections in the future, we'll know right away."
Experts believe that the COVID-19 pandemic will accelerate the widespread acceptance of in-home diagnostic tools such as this. "Shock events" like pandemics can be catalysts for sweeping changes in society, history shows us. The Black Death marked the end of feudalism and ushered in the Renaissance while the aftershocks of the Great Depression and two world wars in the 20th century led to the social safety net of the New Deal and NATO and the European Union. COVID-19 could fundamentally alter the way we deliver healthcare, abandoning the outdated 20th century brick and mortar fee-for-service model in favor of digital medicine. At-home diagnostics may be the leading edge of this seismic shift and the pandemic could accelerate the product innovations that allow for home-based medical screening.
"That's the silver lining to this devastation," says Dr. Leslie Saxon, executive director of the USC Center for Body Computing at the Keck School of Medicine in Los Angeles. As an interventional cardiologist, Saxon has spent her career devising and refining the implantable and wearable wireless devices that are used to treat and diagnose heart conditions and prevent sudden death. "This will open up innovation—research has been stymied by a lack of imagination and marriage to an antiquated model," she adds. "There are already signs this is happening—relaxing state laws about licensure, allowing physicians to deliver health care in non-traditional ways. That's a real sea change and will completely democratize medical information and diagnostic testing."
Ironically, diagnostics have long been a step-child of modern medicine, even though accurate and timely diagnostics play a crucial role in disease prevention, detection and management. "The delivery of health care has proceeded for decades with a blind spot: diagnostic errors—inaccurate or delayed diagnoses—persist throughout all settings of care and continue to harm an unacceptable number of patients," according to a 2015 National Academy of Medicine report. That same report found as many as one out of five adverse events in the hospital result from these errors and they contribute to 10 percent of all patient deaths.
The pandemic should alter the diagnostic landscape. We already have a wealth of wearable and implantable devices, like glucose sensors to monitor blood sugar levels for diabetics, Apple's smart watch, electrocardiogram devices that can detect heart arrythmias, and heart pacemakers.
The Food and Drug Administration is working closely with in-home test developers to make accurate COVID-19 diagnostic tools readily available and has so far greenlighted three at-home collection test kits. Two, LabCorp's and Everlywell's, use nasal swabs to take samples. The third one is a spit test, using saliva samples, that was devised by a Rutgers University laboratory in partnership with Spectrum Solutions and Accurate Diagnostic Labs.
The only way to safely reopen is through large scale testing, but hospitals and doctors' offices are no longer the safest places.
In fact, DIY diagnostic company Everlywell, an Austin, Texas- based digital health company, already offers more than 30 at-home kits for everything from fertility to food sensitivity tests. Typically, consumers collect a saliva or finger-prick blood sample, dispatch it in a pre-paid shipping envelope to a laboratory, and a physician will review the results and send a report to consumers' smartphones.
Thanks to advances in technology, samples taken at home can now be preserved long enough to arrive intact at diagnostic laboratories. The key is showing the agency "transport and shipping don't change or interfere with the integrity of the samples," says Dr. Frank Ong, Everlywell's chief medical and scientific officer.
Ong is keenly aware of the importance of saturation testing because of the lessons learned by colleagues fighting the SARS pandemic in his family's native Taiwan in 2003. "In the beginning, doctors didn't know what they were dealing with and didn't protect themselves adequately," he says. "But over two years, they learned the hard way that there needs to be enough testing, contact tracing of those who have been exposed, and isolation of people who test positive. The value of at-home testing is that it can be done on the kind of broad basis that needs to happen for our country to get back to work."
Because of the pandemic, new policies have removed some of the barriers that impeded the widespread adoption of home-based diagnostics and telemedicine. Physicians can now practice across state lines, get reimbursed for telemedicine visits and use FaceTime to communicate with their patients, which had long been considered taboo because of privacy issues. Doctors and patients are becoming more comfortable and realizing the convenience and benefits of being able to do these things virtually.
Added to this, the only way to safely reopen for business without triggering a second and perhaps even more deadly wave of sickness is through large-scale testing, but hospitals and doctors' offices are no longer the safest places. "We don't want people sitting in a waiting room who later find out they're positive, and potentially infected everyone, including doctors and nurses," says Dr. Kavita Patel, a physician in Washington, DC who served as a policy director in the Obama White House.
In-home testing avoids the risks of direct exposure to the virus for both patients and health care professionals, who can dispense with cumbersome protective gear to take samples, and also enables people without reliable transportation or child-care to learn their status. "At home testing can be a critical component of our country's overall testing strategy," says Dr. Shantanu Nundy, chief medical officer at Accolade Health and on the faculty of the Milken Institute School of Public Health at George Washington University. "Once we're back at work, we need to be much more targeted, and have much more access to data and controlling those outbreaks as tightly as possible. The best way to do that is by leapfrogging clinics and being able to deliver tests at home for people who are disenfranchised by the current system."
In the not-too-distant future, in-home diagnostics could be a key component of precision medicine, which is customized care tailored specifically to each patient's individual needs. Like Stanford's smart toilet prototype, these ongoing surveillance tools will gather health data, ranging from exposures to toxins and pollutions in the environment to biochemical activity, like rising blood pressure, signs of inflammation, failing kidneys or tiny cancerous tumors, and provide continuous real-time information.
"These can be deeply personalized and enabled by smart phones, sensors and artificial intelligence," says USC's Leslie Saxon. "We'll be seeing the floodgates opening to patients accessing medical services through the same devices that they access other things, and leveraging these tools for our health and to fine tune disease management in a model of care that is digitally enabled."
[Editor's Note: This article was originally published on June 8th, 2020 as part of a standalone magazine called GOOD10: The Pandemic Issue. Produced as a partnership among LeapsMag, The Aspen Institute, and GOOD, the magazine is available for free online.]

