How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
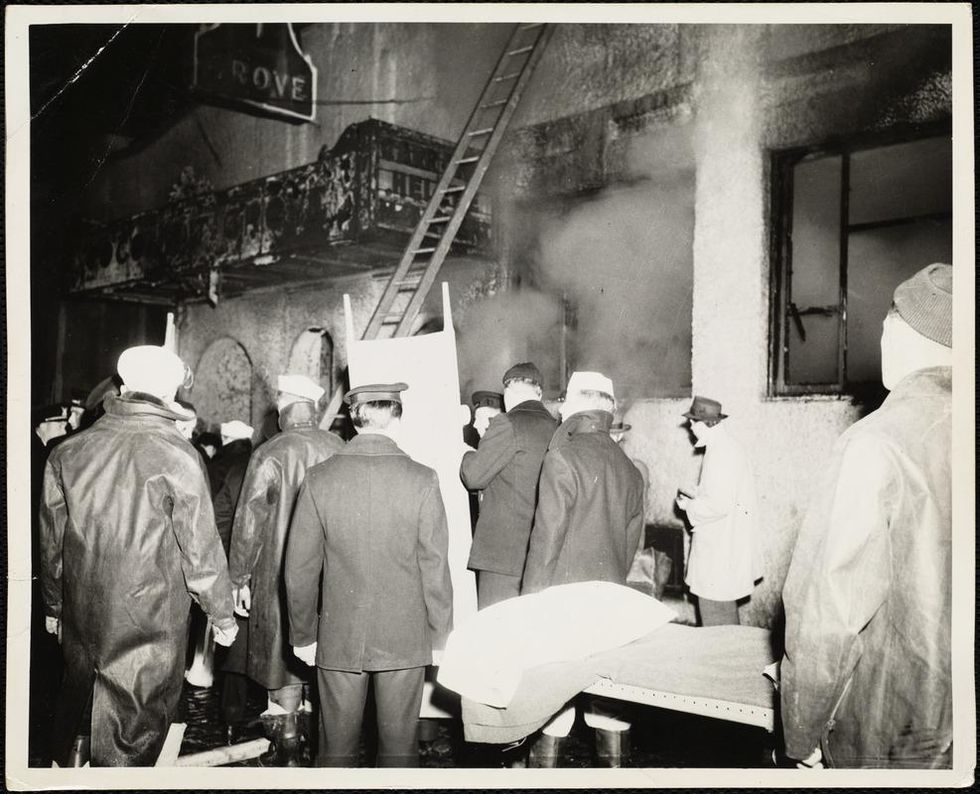
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
Enter our writing contest for a chance to win a cash prize and publication on leapsmag.
Last year, we sponsored a short story contest, asking writers to share a fictional vision of how emerging technology might shape the future. This year, the competition has a new spin.
The Prompt:
Write a personal essay of up to 2000 words describing how a new advance in medicine or science has profoundly affected your life.
The Rules:
Submissions must be received by midnight EST on September 20th, 2019. Send your original, previously unpublished essay as a double-spaced attachment in size 12 Times New Roman font to kira@leapsmag.com. Include your name and a short bio. It is free to enter, and authors retain all ownership of their work. Upon submitting an entry, the author agrees to grant leapsmag one-time nonexclusive publication rights.
All submissions will be judged by the Editor-in-Chief on the basis of insightfulness, quality of writing, and relevance to the prompt. The Contest is open to anyone around the world of any age, except for the friends and family of leapsmag staff and associates.
The winners will be announced by October 31st, 2019.
The Prizes:
Grand Prize: $500, publication of your story on leapsmag, and promotion on our social media channels.
First Runner-Up: $100 and a shout-out on our social media channels.
Good luck!
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Men and Women Experience Pain Differently. Learning Why Could Lead to Better Drugs.
According to the CDC, one fifth of American adults live with chronic pain, and women are affected more than men.
It's been more than a decade since Jeannette Rotondi has been pain-free. A licensed social worker, she lives with five chronic pain diagnoses, including migraines. After years of exploring treatment options, doctors found one that lessened the pain enough to allow her to "at least get up."
"With all that we know now about genetics and the immune system, I think the future of pain medicine is more precision-based."
Before she says, "It was completely debilitating. I was spending time in dark rooms. I got laid off from my job." Doctors advised against pregnancy; she and her husband put off starting a family for almost a decade.
"Chronic pain is very unpredictable," she says. "You cannot schedule when you'll be in debilitative pain or cannot function. You don't know when you'll be hit with a flare. It's constantly in your mind. You have to plan for every possibly scenario. You need to carry water, medications. But you can't plan for everything." Even odors can serve as a trigger.
According to the CDC, one fifth of American adults live with chronic pain, and women are affected more than men. Do men and women simply vary in how much pain they can handle? Or is there some deeper biological explanation? The short answer is it's a little of both. But understanding the biological differences can enable researchers to develop more effective treatments.
While studies in animals are straightforward (they either respond to pain or they don't), humans are more complex. Social and psychological factors can affect the outcome. For example, one Florida study found that gender role expectations influenced pain sensitivity.
"If you are a young male and you believe very strongly that men are tougher than women, you will have a much higher threshold and will be less sensitive to pain," says Robert Sorge, an associate professor at the University of Alabama at Birmingham whose lab researches the immune system's involvement in pain and addiction.
He also notes, "We looked at transgender women and their pain sensitivity in comparison to cis men and women. They show very similar pain sensitivity to cis women, so that may reduce the impact of genetic sex in terms of what underlies that sensitivity."
But the difference goes deeper than gender expectations. There are biological differences as well. In 2015, Sorge and his team discovered that pain stimuli activated different immune cells in male and female rodents and that the presence of testosterone seemed to be a factor in the response.
More recently, Ted Price, professor of neuroscience at University of Texas, Dallas, examined pain at a genetic level, specifically looking at the patterns of RNA, which are single-stranded molecules that act as a messenger for DNA. Price noted that there were differences in these patterns that coincided with whether an individual experienced pain.
Price explains, "Every cell in your body has DNA, but the RNA that is in the cells is different for every cell type. The RNA in any particular cell type, like a neuron, can change as a result of some environmental influence like an injury. We found a number of genes that are potentially causative factors for neuropathic pain. Those, interestingly, seemed to be different between men and women."
Differences in treatment also affect pain response. Sorge says, "Women are experiencing more pain dismissal and more hostility when they report chronic pain. Women are more likely to have their pain associated with psychological issues." He adds that this dismissal may require women to exaggerate symptoms in order to be believed.
This can impact pain management. "Women are more likely to be prescribed and to use opioids," says Dr. Roger B. Fillingim, Director of Pain Research and Intervention Center of Excellence at the University of Florida. Yet, when self-administering pain meds, "women used significantly less opioids after surgery than did men." He also points out that "men are at greater risk for dose escalation and for opioid-related death than are women. So even though more women are using opioids, men are more likely to die from opioid-related causes."
Price acknowledges that other drugs treat pain, but "unfortunately, for chronic pain, none of these drugs work very well. We haven't yet made classes of drugs that really target the underlying mechanism that causes people to have chronic pain."
New drugs are now being developed that "might be particularly efficacious in women's chronic pain."
Sorge points out that there are many variables in pain conditions, so drugs that work for one may be ineffective for another. "With all that we know now about genetics and the immune system, I think the future of pain medicine is more precision-based, where based on your genetics, your immune status, your history, we may eventually get to the point where we can say [certain] drugs have a much bigger chance of working for you."
It will take some time for these new discoveries to translate into effective treatments, but Price says, "I'm excited about the opportunities. DNA and RNA sequencing totally changes our ability to make these therapeutics. I'm very hopeful." New drugs are now being developed that "might be particularly efficacious in women's chronic pain," he says, because they target specific receptors that seem to be involved when only women experience pain.
Earlier this year, three such drugs were approved to treat migraines; Rotondi recently began taking one. For Rotondi, improved treatments would allow her to "show up for life. For me," she says, "it would mean freedom."