How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
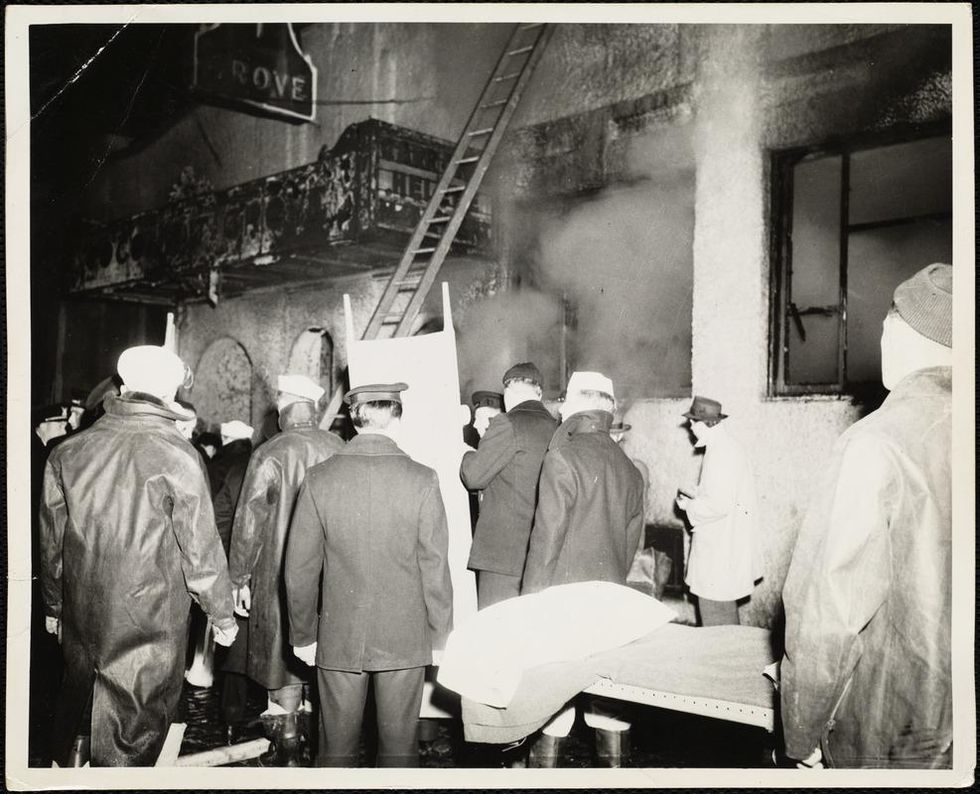
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
“Coming Back from the Dead” Is No Longer Science Fiction
A man receiving cardiopulmonary resuscitation (CPR).
Last year, there were widespread reports of a 53-year-old Frenchman who had suffered a cardiac arrest and "died," but was then resuscitated back to life 18 hours after his heart had stopped.
The once black-and-white line between life and death is now blurrier than ever.
This was thought to have been possible in part because his body had progressively cooled down naturally after his heart had stopped, through exposure to the outside cold. The medical team who revived him were reported as being "stupefied" that they had been able to bring him back to life, in particular since he had not even suffered brain damage.
Interestingly, this man represents one of a growing number of extraordinary cases in which people who would otherwise be declared dead have now been revived. It is a testament to the incredible impact of resuscitation science -- a science that is providing opportunities to literally reverse death, and in doing so, shedding light on the age-old question of what happens when we die.
Death: Past and Present
Throughout history, the boundary between life and death was marked by the moment a person's heart stopped, breathing ceased, and brain function shut down. A person became motionless, lifeless, and was deemed irreversibly dead. This is because once the heart stops beating, blood flow stops and oxygen is cut off from all the body's organs, including the brain. Consequently, within seconds, breathing stops and brain activity comes to a halt. Since the cessation of the heart literally occurs in a "moment," the philosophical notion of a specific point in time of "irreversible" death still pervades society today. The law, for example, relies on "time of death," which corresponds to when the heart stops beating.
The advent of cardiopulmonary resuscitation (CPR) in the 1960s was revolutionary, demonstrating that the heart could potentially be restarted after it had stopped, and what had been a clear black-and-white line was shown to be potentially reversible in some people. What was once called death—the ultimate end point— was now widely called cardiac arrest, and became a starting point.
From then on, it was only if somebody had requested not to be resuscitated or when CPR was deemed to have failed that people would be declared dead by "cardiopulmonary criteria." Biologically, cardiac arrest and death by cardiopulmonary criteria are the same process, albeit marked at different points in time depending on when a declaration of death is made.
The apparent irreversibility of death as we know it may not necessarily reflect true irretrievable cellular damage inside the body.
Clearly, contrary to many people's perceptions, cardiac arrest is not a heart attack; it is the final step in death irrespective of cause, whether it be a stroke, a heart attack, a car accident, an overwhelming infection or cancer. This is how roughly 95 percent of the population are declared dead.
The only exception is the small proportion of people who may have suffered catastrophic brain injuries, but whose hearts can be artificially kept beating for a period of time on life-support machines. These people can be legally declared dead based on brain death criteria before their hearts have stopped. This is because the brain can die either from oxygen starvation after cardiac arrest or from massive trauma and internal bleeding. Either way, the brain dies hours or possibly longer after these injuries have taken place and not just minutes.
A Profound Realization
What has become increasingly clear is that the apparent irreversibility of death as we know it may not necessarily reflect true irretrievable cellular damage inside the body. This is consistent with a mounting understanding: it is only after a person actually dies that the cells in the body start to undergo their own process of death. Intriguingly, this process is something that can now be manipulated through medical intervention. Being cold is one of the factors that slows down the rate of cellular decay. The 53-year-old Frenchman's case and the other recent cases of resuscitation after prolonged periods of time illustrate this new understanding.
Last week's earth-shattering announcement by neuroscientist Dr. Nenad Sestan and his team out of Yale, published in the prestigious scientific journal Nature, provides further evidence that a time gap exists between actual death and cellular death in cadavers. In this seminal study, these researchers were able to restore partial function in pig brains four hours after their heads were severed from their bodies. These results follow from the pioneering work in 2001 of geneticist Fred Gage and colleagues from the Salk Institute, also published in Nature, which demonstrated the possibility of growing human brain cells in the laboratory by taking brain biopsies from cadavers in the mortuary up to 21 hours post-mortem.
The once black-and-white line between life and death is now blurrier than ever. Some people may argue this means these humans and pigs weren't truly "dead." However, that is like saying the people who were guillotined during the French Revolution were also not dead. Clearly, that is not the case. They were all dead. The problem is not death; it's our reliance on an outdated philosophical, rather than biological, notion of death.
Death can no longer be considered an absolute moment but rather a process that can be reversed even many hours after it has taken place.
But the distinction between irreversibility from a medical perspective and biological irreversibility may not matter much from a pragmatic perspective today. If medical interventions do not exist at any given time or place, then of course death cannot be reversed.
However, it is crucial to distinguish between biologically and medically: When "irreversible" loss of function arises due to inadequate treatment, then a person could be potentially brought back in the future when an alternative therapy becomes available, or even today if he or she dies in a location where novel treatments can slow down the rate of cell death. However, when true irreversible loss of function arises from a biological perspective, then no treatment will ever be able to reverse the process, whether today, tomorrow, or in a hundred years.
Probing the "Grey Zone"
Today, thanks to modern resuscitation science, death can no longer be considered an absolute moment but rather a process that can be reversed even many hours after it has taken place. How many hours? We don't really know.
One of the wider implications of our medical advances is that we can now study what happens to the human mind and consciousness after people enter the "grey zone," which marks the time after the heart stops, but before irreversible and irretrievable cell damage occurs, and people are then brought back to life. Millions have been successfully revived and many have reported experiencing a unique, universal, and transformative mental state.
Were they "dead"? Yes, according to all the criteria we have ever used. But they were able to be brought back before their "dead" bodies had reached the point of permanent, irreversible cellular damage. This reflects the period of death for all of us. So rather than a "near-death experience," I prefer a new terminology to describe these cases -- "an actual-death experience." These survivors' unique experiences are providing eyewitness testimonies of what we will all be likely to experience when we die.
Such an experience reportedly includes seeing a warm light, the presence of a compassionate perfect individual, deceased relatives, a review of their lives, a judgment of their actions and intentions as they pertain to their humanity, and in some cases a sensation of seeing doctors and nurses working to resuscitate them.
Are these experiences compatible with hallucinations or illusions? No -- in part, because these people have described real, verifiable events, which, by definition are not hallucinations, and in part, because their experiences are not compatible with confused and delirious memories that characterize oxygen deprivation.
The challenge for us scientifically is understanding how this is possible at a time when all our science tells us the brain shuts down.
For instance, it is hard to classify a structured meaningful review of one's life and one's humanity as hallucinatory or illusory. Instead, these experiences represent a new understanding of the overall human experience of death. As an intensive care unit physician for more than 10 years, I have seen numerous cases where these reports have been corroborated by my colleagues. In short, these survivors have been known to come back with reports of full consciousness, with lucid, well-structured thought processes and memory formation.
The challenge for us scientifically is understanding how this is possible at a time when all our science tells us the brain shuts down. The fact that these experiences occur is a paradox and suggests the undiscovered entity we call the "self," "consciousness," or "psyche" – the thing that makes us who we are - may not become annihilated at the point of so-called death.
At New York University, the State University of New York, and across 20 hospitals in the U.S. and Europe, we have brought together a new multi-disciplinary team of experts across many specialties, including neurology, cardiology, and intensive care. Together, we hope to improve cardiac arrest prevention and treatment, as well as to address the impact of new scientific discoveries on our understanding of what happens at death.
One of our first studies, Awareness during Resuscitation (AWARE), published in the medical journal Resuscitation in 2014, confirmed that some cardiac arrest patients report a perception of awareness without recall; others report detailed memories and experiences; and a few report full auditory and visual awareness and consciousness of their experience, from a time when brain function would be expected to have ceased.
While you probably have some opinion or belief about this based upon your own philosophical, religious, or cultural background, you may not realize that exploring what happens when we die is now a subject that science is beginning to investigate.
There is no question more intriguing to humankind. And for the first time in our history, we may finally uncover some real answers.
A healthy middle-aged couple enjoying a hike. (Shutterstock)
[Editor's Note: This video is the fourth of a five-part series titled "The Future Is Now: The Revolutionary Power of Stem Cell Research." Produced in partnership with the Regenerative Medicine Foundation, and filmed at the annual 2019 World Stem Cell Summit, this series illustrates how stem cell research will profoundly impact human life.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

