How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
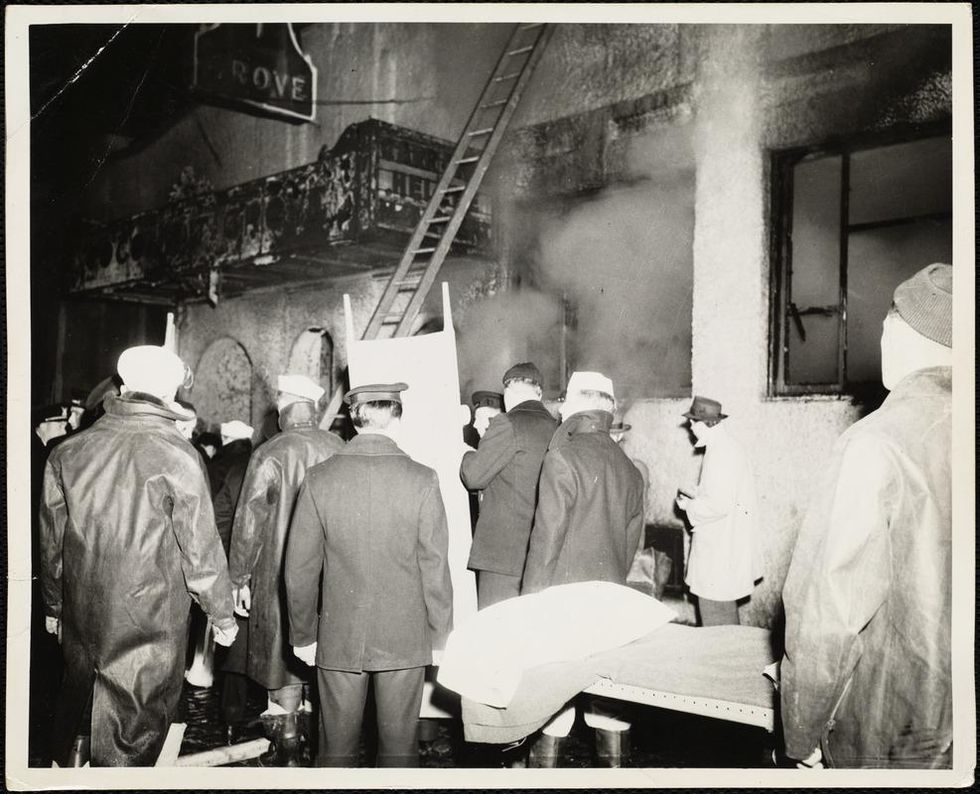
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
He Almost Died from a Deadly Superbug. A Virus Saved Him.
Tom Patterson holding an image of Acinetobacter baumannii and Steffanie Strathdee holding an image of a bacteriophage.
An attacking rogue hippo, giant jumping spiders, even a coup in Timbuktu couldn't knock out Tom Patterson, but now he was losing the fight against a microscopic bacteria.
Death seemed inevitable, perhaps hours away, despite heroic efforts to keep him alive.
It was the deadly drug-resistant superbug Acinetobacter baumannii. The infection struck during a holiday trip with his wife to the pyramids in Egypt and had sent his body into toxic shock. His health was deteriorating so rapidly that his insurance company paid to medevac him first to Germany, then home to San Diego.
Weeks passed as he lay in a coma, shedding more than a hundred pounds. Several major organs were on the precipice of collapse, and death seemed inevitable, perhaps hours away despite heroic efforts by a major research university hospital to keep Tom alive.

Tom Patterson in a deep coma on March 14, 2016, the day before phage therapy was initiated.
(Courtesy Steffanie Strathdee)
Then doctors tried something boldly experimental -- injecting him with a cocktail of bacteriophages, tiny viruses that might infect and kill the bacteria ravaging his body.
It worked. Days later Tom's eyes fluttered open for a few brief seconds, signaling that the corner had been turned. Recovery would take more weeks in the hospital and about a year of rehabilitation before life began to resemble anything near normal.
In her new book The Perfect Predator, Tom's wife, Steffanie Strathdee, recounts the personal and scientific ordeal from twin perspectives as not only his spouse but also as a research epidemiologist who has traveled the world to track down diseases.
Part of the reason why Steff wrote the book is that both she and Tom suffered severe PTSD after his illness. She says they also felt it was "part of our mission, to ensure that phage therapy wasn't going to be forgotten for another hundred years."

Tom Patterson and Steffanie Strathdee taking a first breath of fresh air during recovery outside the UCSD hospital.
(Courtesy Steffanie Strathdee)
From Prehistoric Arms Race to Medical Marvel
Bacteriophages, or phages for short, evolved as part of the natural ecosystem. They are viruses that infect bacteria, hijacking their host's cellular mechanisms to reproduce themselves, and in the process destroying the bacteria. The entire cycle plays out in about 20-60 minutes, explains Ben Chan, a phage research scientist at Yale University.
They were first used to treat bacterial infections a century ago. But the development of antibiotics soon eclipsed their use as medicine and a combination of scientific, economic, and political factors relegated them to a dusty corner of science. The emergence of multidrug-resistant bacteria has highlighted the limitations of antibiotics and prompted a search for new approaches, including a revived interest in phages.
Most phages are very picky, seeking out not just a specific type of bacteria, but often a specific strain within a family of bacteria. They also prefer to infect healthy replicating bacteria, not those that are at rest. That's what makes them so intriguing to tap as potential therapy.
Tom's case was one of the first times that phages were successfully infused into the bloodstream of a human.
Phages and bacteria evolved measures and countermeasures to each other in an "arms race" that began near the dawn of life on the planet. It is not that one consciously tries to thwart the other, says Chan, it's that countless variations of each exists in the world and when a phage gains the upper hand and kills off susceptible bacteria, it opens up a space in the ecosystem for similar bacteria that are not vulnerable to the phage to increase in numbers. Then a new phage variant comes along and the cycle repeats.
Robert "Chip" Schooley is head of infectious diseases at the University of California San Diego (UCSD) School of Medicine and a leading expert on treating HIV. He had no background with phages but when Steff, a friend and colleague, approached him in desperation about using them with Tom, he sprang into action to learn all he could, and to create a network of experts who might provide phages capable of killing Acinetobacter.
"There is very little evidence that phage[s] are dangerous," Chip concluded after first reviewing the literature and now after a few years of experience using them. He compares broad-spectrum antibiotics to using a bazooka, where every time you use them, less and less of the "good" bacteria in the body are left. "With a phage cocktail what you're really doing is more of a laser."
Collaborating labs were able to identify two sets of phage cocktails that were sensitive to Tom's particular bacterial infection. And the FDA acted with lightning speed to authorize the experimental treatment.

A bag of a four-phage "cocktail" before being infused into Tom Patterson.
(Courtesy Steffanie Strathdee)
Tom's case was scientifically important because it was one of the first times that phages were successfully infused into the bloodstream of a human. Most prior use of phages involved swallowing them or placing them directly on the area of infection.
The success has since sparked a renewed interest in phages and a reexamination of their possible role in medicine.
Over the two years since Tom awoke from his coma, several other people around the world have been successfully treated with phages as part of their regimen, after antibiotics have failed.
The Future of Phage Therapy
The experience treating Tom prompted UCSD to create the Center for Innovative Phage Applications and Therapeutics (IPATH), with Chip and Steff as co-directors. Previous labs have engaged in basic research on phages, but this is the first clinical center in North America to focus on translating that knowledge into treating patients.
In January, IPATH announced the first phase 2 clinical trial approved by the FDA that will use phages intravenously. The viruses are being developed by AmpliPhi Biosciences, a San Diego-based company that supplied one of the phages used to treat Tom. The new study takes on drug resistant Staph aureus bacteria. Experimental phage therapy treatment using the company's product candidates was recently completed in 21 patients at seven hospitals who had been suffering from serious infections that did not respond to antibiotics. The reported success rate was 84 percent.
The new era of phage research is applying cutting-edge biologic and informatics tools to better understand and reshape the viruses to better attack bacteria, evade resistance, and perhaps broaden their reach a bit within a bacterial family.
Genetic engineering tools are being used to enhance the phages' ability to infect targeted bacteria.
"As we learn more and more about which biological activities are critical and in which clinical settings, there are going to be ways to optimize these activities," says Chip. Sometimes phages may be used alone, other times in combination with antibiotics.
Genetic engineering using tools are being used to enhance the phages' ability to infect targeted bacteria and better counter evolving forms of bacterial resistance in the ongoing "arms race" between the two. It isn't just theory. A patient recently was successfully treated with a genetically modified phage as part of the regimen, and the paper is in press.
In reality, given the trillions of phages in the world and the endless encounters they have had with bacteria over the millennia, it is likely that the exact phages needed to kill off certain bacteria already exist in nature. Using CRISPR to modify a phage is simply a quick way to identify the right phage useful for a given patient and produce it in the necessary quantities, rather than go search for the proverbial phage needle in a sewage haystack, says Chan.
One non-medical reason why using modified phages could be significant is that it creates an intellectual property stake, something that is patentable with a period of exclusive use. Major pharmaceutical companies and venture capitalists have been hesitant to invest in organisms found in nature; but a patentable modification may be enough to draw their interest to phage development and provide the funding for large-scale clinical trials necessary for FDA approval and broader use.
"There are 10 million trillion trillion phages on the planet, 10 to the power of 31. And the fact is that this ongoing evolutionary arms race between bacteria and phage, they've been at it for a millennia," says Steff. "We just need to exploit it."
This Mom Is On a Mission to End Sickle Cell Disease
Adrienne Shapiro and her daughter Marissa, who is the fifth generation of children in the family to inherit sickle cell disease, pose in 2018 for a selfie after a new medicine Endari transformed their lives.
[Editor's Note: This video is the third of a five-part series titled "The Future Is Now: The Revolutionary Power of Stem Cell Research." Produced in partnership with the Regenerative Medicine Foundation, and filmed at the annual 2019 World Stem Cell Summit, this series illustrates how stem cell research will profoundly impact human life.]
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.