How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
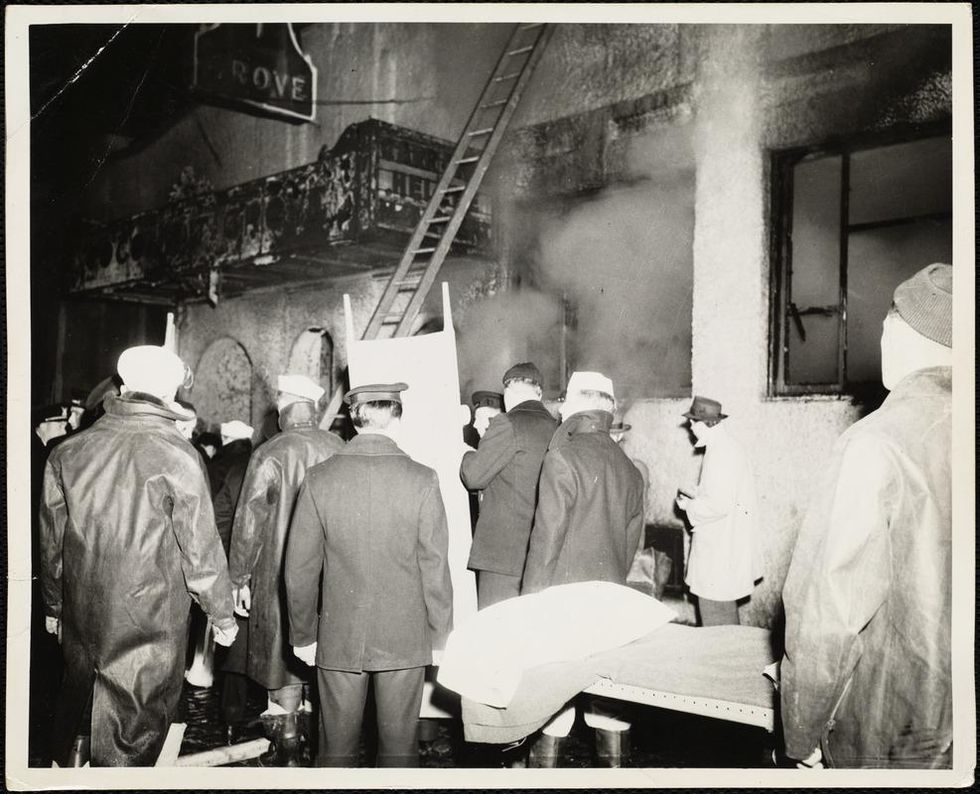
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
New Cell Therapies Give Hope to Diabetes Patients
Researchers are developing new cell therapies that could cure Type 1 diabetes and make constant management of the disease a way of the past.
For nearly four decades, George Huntley has thought constantly about his diabetes. Diagnosed in 1983 with Type 1 (insulin-dependent) diabetes, Huntley began managing his condition with daily finger sticks to check his blood glucose levels and doses of insulin that he injected into his abdomen. Even now, with an insulin pump and a device that continuously monitors his glucose, he must consider how every meal will affect his blood sugar, checking his monitor multiple times each hour.
Like many of those who depend on insulin injections, Huntley is simultaneously grateful for the technology that makes his condition easier to manage and tired of thinking about diabetes. If he could wave a magic wand, he says, he would make his diabetes disappear. So when he read about biotechs like ViaCyte and Vertex Pharmaceuticals developing new cell therapies that have the potential to cure Type 1 diabetes, Huntley was excited.
You also won’t see him signing up any time soon. The therapies under development by both companies would require a lifelong regimen of drugs for suppressing the immune system to prevent the body from rejecting the foreign cells. It’s a problem also seen in the transplant of insulin-producing cells of the pancreas – called islet cells – from deceased donors. To Howard Foyt, chief medical officer at ViaCyte, a San Diego-based biotech specializing in the development of cell therapies for diabetes, the tradeoff is worth it.
“A lot of the symptoms of diabetes are not something that you wear on your arm, so to speak. You’re not necessarily conscious of them until you’re successfully treated, and you feel better,” Foyt says.
For many with diabetes, managing these symptoms is a constant game of Whack-a-Mole. “Any form of treatment that gets someone closer to feeling good is a victory,” he says.
“Am I going to be trading diabetes for cancer? That’s not a chance I
want to take."
But not everyone is convinced. What’s more, it’s likely that the availability of these cell therapies will be limited to those with life-threatening diabetes symptoms, such as hypoglycemia unawareness. To Huntley, these therapies remain a bit of a Faustian bargain.
“Am I going to be trading diabetes for cancer? That’s not a chance I want to take,” he says.
The discovery of insulin in 1921 transformed Type 1 diabetes from a death sentence into a potentially manageable condition. Even as better versions of insulin hit the market—ones that weren’t derived from pigs and wouldn’t provoke an allergic response, longer-acting insulin, insulin pens—they didn’t change the reality that those with Type 1 diabetes remained dependent on insulin. Even the most advanced continuous glucose monitors (which tests blood sugar levels every few minutes, 24/7) and insulin pumps don’t perform as well as a healthy pancreas.
Whether by injection or pump, someone with diabetes needs to administer the insulin their body no longer makes. With advances in organ transplantation, the concept of transplanting insulin-producing pancreatic beta cells seemed obvious. After more than a decade of painstaking work, James Shapiro, who directs the Islet Transplant Program at the University of Albania, honed a process called the Edmonton Protocol for pancreas transplants. For a few patients who couldn’t control their blood sugars any other way, the Edmonton Protocol became a life saver. Some of these patients were even able to stop insulin completely, Shapiro says. But the high cost of organ transplant and a chronic shortage of donor organs, pancreas or otherwise, meant that only a small handful of patients could benefit.
Stem cells, however, can be grown in vats, meaning that supply would never be an issue. “We would be going from a very successful treatment of today to a potential cure tomorrow,” Shapiro says.
In 2014, spurred by his own children’s diagnoses with Type 1 Diabetes, stem cell biologist Doug Melton of Harvard University figured out a way to differentiate embryonic stem cells into functional pancreatic beta cells. It was a long process, explains immunoengineer Alice Tomei at the University of Miami, because “the islet is not one cell, it's like a mini-organ that has its own needs.”
Add on the risk of rejection and autoimmunity, and Tomei says that scientists soon realized that chronic and systemic immunosuppression was the only way forward. Over the next several years, Melton improved his approach to yield more cells with fewer impurities. Melton partnered with Boston-based Vertex Pharmaceuticals to create a cell therapy called VX-880.
The first patient received his dose earlier in 2021. In October, Vertex released 90-day results from the Phase 1/2 trial, which revealed the patient was able to reduce his insulin usage from an average of 34 units per day to just 2.9 units per day. The tradeoff is a lifelong need for immunosuppressive drugs to prevent the body from attacking both foreign cells and pancreatic beta cells. It’s what recipients of ViaCyte’s first-gen PEC-Direct will also need. For Foyt, it’s an easy choice.
“At this point in time, immunosuppression is the necessary evil,” he says. “For parents, would you like to worry about going into your child’s bedroom every morning and not knowing if they’re going to be alive or dead? It’s uncommon, but it does occur.”
Not everyone, however, finds the trade-off easy to swallow. Especially with COVID-19 cases reaching record highs, the prospect of reducing his immune function at a time when he needs it most doesn’t sit well with Huntley. The risks of immunosuppression also mean that diabetes cell therapies are limited to those patients with life-threatening complications.
It’s why ViaCyte has created two new iterations of cellular therapies that would eliminate this need. The ViaCyte-Encap contains the cells in a permeable container that allows oxygen, insulin, and nutrients to flow freely but prevents immune system access. Their latest model, PEC-QT, just began safety trials with Shapiro’s lab at the University of Alberta and uses gene editing to eliminate any cellular markers that would trigger an immune response.
Sanjoy Dutta, vice president of research at JDRF International, a nonprofit that funds the study of diabetes, is thrilled with the progress that’s been made around cell therapies, but he cautions it’s still early days. “We have proven that these cells can be made. What we haven’t seen is are they going to work for six months, two years, five years? It’s a challenge we still need to overcome,” he says.
Iowa social worker Jodi Lynn’s concerns echo Dutta’s. Lynn was diagnosed with diabetes in 1998 at age 14 after a bout of severe influenza, spends each day inventorying supplies, planning her food intake, and maintaining her insulin pump and glucose monitor. These newer technologies dramatically improved her blood sugar control but, like everyone with diabetes, Lynn remains at high risk for complications, such as diabetic ketoacidosis, heart disease, vision loss, and kidney failure. Lynn, already considered immunocompromised due to medications she takes for another autoimmune condition, is less concerned with immune suppression than the untested nature of these therapies.
“I want to know that they will work long-term,” she says.
How Genetic Testing and Targeted Treatments Are Helping More Cancer Patients Survive
Scientists are studying cancer genomes to more precisely diagnose their patients' diseases - offering hope for targeted drug treatments.
Late in 2018, Chris Reiner found himself “chasing a persistent cough” to figure out a cause. He talked to doctors; he endured various tests, including an X-ray. Initially, his physician suspected bronchitis. After several months, he still felt no improvement. In May 2019, his general practitioner recommended that Reiner, a business development specialist for a Seattle-based software company, schedule a CAT scan.
Reiner knew immediately that his doctor asking him to visit his office to discuss the results wasn’t a good sign. The longtime resident of Newburyport, MA, remembers dreading “that conversation that people who learn they have cancer have.”
“The doctor handed me something to look at, and the only thing I remember after that was everything went blank all around me,” Reiner, 50, reveals. “It was the magnitude of what he was telling me, that I had a malignant mass in my lung.”
Next, he recalls, he felt ushered into “the jaws of the medical system very quickly.” He spent a couple of days meeting with a team of doctors at Beth Israel Deaconess Medical Center in nearby Boston. One of them was from a medical field he hadn’t even known existed, a pulmonary interventionist, who would perform a biopsy on the mass in his lung.
“Knowing there was a medicine for my particular type of cancer was like a weight lifted off my shoulders."
A week later he and his wife Allison returned to meet with the oncologist, radiologist, pulmonary interventionist – his medical team. They confirmed his initial diagnosis: Stage 4 metastatic lung cancer that had spread to several parts of his body. “We just sat there, stunned,” he says. “I felt like I was getting hit by a wrecking ball over and over.”
An onslaught of medical terminology about what they had identified flowed over the shocked couple, but then the medical team switched gears, he recalls. They offered hope. “They told me, ‘Hey, you’re not a smoker, so that’s good,’” Reiner says. “‘There’s a good chance that what’s driving this disease for you is actually a genetic mutation, and we have ways to understand more about what that could be through some simple testing.’”
They told him about Foundation Medicine, a company launched in neighboring Cambridge, MA, in 2009 that develops, manufactures, and sells genomic profiling assays. These are tests that, according to the company’s website, “can analyze a broad panel of genes to detect the four main classes of genomic alterations known to drive cancer growth.” With these insights, certain patients can be matched with therapies targeted specifically for the genetic driver(s) of their cancer. The company maintains one of the largest cancer genomic databases in the world, with more than 500,000 patient samples profiled, and they have more than 65 biopharma partners.
According to Foundation Medicine, they are the only company that has FDA-approved tests for both tissue- and blood-based comprehensive genomic profiling tests. One other company has an FDA-approved biopsy test, and several other companies offer tissue-based genomic profiling. Additionally, several major cancer centers like Memorial Sloan Kettering in New York and Anderson Cancer Center in Texas have their own such testing platforms.
Currently, genomic profiling is more accessible for patients with advanced cancer, due to broader insurance coverage in later stages of disease.
“Right now, the vast majority of patients either have cancers for which we don’t have treatments or they have genetic alterations that are not known,” says Jorge Garcia, MD, Division Chief, Solid Tumor Oncology, UH Cleveland Medical Center, which has its own CGP testing platform. “However, a significant proportion of patients with advanced cancer have alterations that we can tap for therapeutic purposes.”
Foundation Medicine estimates that in 2017, just over 5 percent of advanced solid cancer patients in the U.S. received CGP testing. In 2021, they estimate that number is between 25 to 30 percent of advanced solid cancer patients in the U.S., which doesn’t include patients who are tested with small (less than 50 genes) panels. Their panel tests for more than 300 cancer-related genes.

“The good news is the platforms we are developing are better and more comprehensive, and they’re going to continue to be larger data sets,” Dr. Garcia adds.
In Reiner’s case, his team ordered comprehensive genetic profiling on both his tissue and blood, from Foundation Medicine.
At this point, Reiner still wasn’t sure what genetic mutations were or how they factored into cancer or what comprehensive genomic profiling entailed. That day, though, his team ushered the Reiners into the world of precision oncology that placed him on much more sure footing to learn about and fight the specific lung cancer that had been troubling him for more than a year.
What genetic alterations were driving his cancer? Foundation Medicine’s tests were about to find out.
At the core of these tests is next generation sequencing, a DNA sequencing technology. Since 2009, this has revolutionized genomic research, according to the National Center for Biotechnology Information, because it allows an entire human genome to be sequenced within one day. Cancer genomics posits that cancer is caused by mutations and is a disease of the genome. Now, cancer genomes can be systemically studied in their entirety. For cancer patients such as Reiner, NGS can provide a more precise diagnosis and classification of the disease, more accurate prognosis, and potentially the identification of targeted drug treatments. Ultimately, the technology can provide the basis of personalized cancer management.
The detailed reports supply patients and their oncologists with extensive information about the patient’s genomic profile and potential treatment options that they can discuss together. Reiner trusted his doctors that this approach was worth the two- or three-week wait to receive the Foundation Medicine report and the specifically targeted treatment, rather than immediately jump into a round of chemotherapy. He is especially grateful now, he says, because the report delivered a great deal of relief from his previously exhausting and growing anxiety about having cancer.
Reiner and his team learned his lung cancer contained the epidermal growth factor receptor (EGFR) mutation. That biomarker enabled his oncologist to prescribe Tagrisso (osimertinib), a medication developed to directly target that genetic mutation.
“Knowing there was a medicine for my particular type of cancer was like a weight lifted off my shoulders,” he says. “It only took a week or two before my cough finally started subsiding. This pill goes right after the particular piece of genetic material in the tumor that’s causing its growth.”
Dr. Jerry Mitchell, director field medical oncology, Foundation Medicine, in Columbus, Ohio, explains that genomic profiling is generating substantial impacts today. “This is a technology that is the standard of care across many advanced malignancies that takes patients from chemotherapy-only options to very targeted options or immunotherapy options,” he says. “You can also look at complex biomarkers, and these are not specific genetic changes but different genes across the tumor to get a biomarker.”
According to Dr. Mitchell, Foundation Medicine’s technology can test more than 324 different cancer-related genes in a single test. Thus, a growing number of patients are benefitting from comprehensive genetic profiling, due to the rapidly growing number of targeted therapies. While not all of the cancers are treatable yet, the company uses that information to partner with researchers to find new potential therapies for patient groups that may have rare mutations.
Since his tumor’s diagnosis, Reiner has undergone chemotherapy and a couple surgeries to treat the metastatic cancer in other parts of his body, but the drug Tagrisso has significantly reduced his lung tumor. Now, having learned so much during the past couple of years, he is grateful for precision oncology. He still reflects on the probability that, had the Tagrisso pill not been available in May 2019, he might have only survived for another six months or a year.
“Comprehensive Genomic Profiling is not some future state, but in both the U.S. and Europe, it is a very standard, accepted, and recommended first step to knowing how to treat your cancer,” says Dr. Mitchell, adding that he feels fortunate to be an oncologist in this era. “However, we know there are still people not getting this recommended testing, so we still have opportunities to find many more patients and impact them by knowing the molecular profile of their cancer.”

