How a Deadly Fire Gave Birth to Modern Medicine

The Cocoanut Grove fire in Boston in 1942 tragically claimed 490 lives, but was the catalyst for several important medical advances.
On the evening of November 28, 1942, more than 1,000 revelers from the Boston College-Holy Cross football game jammed into the Cocoanut Grove, Boston's oldest nightclub. When a spark from faulty wiring accidently ignited an artificial palm tree, the packed nightspot, which was only designed to accommodate about 500 people, was quickly engulfed in flames. In the ensuing panic, hundreds of people were trapped inside, with most exit doors locked. Bodies piled up by the only open entrance, jamming the exits, and 490 people ultimately died in the worst fire in the country in forty years.
"People couldn't get out," says Dr. Kenneth Marshall, a retired plastic surgeon in Boston and president of the Cocoanut Grove Memorial Committee. "It was a tragedy of mammoth proportions."
Within a half an hour of the start of the blaze, the Red Cross mobilized more than five hundred volunteers in what one newspaper called a "Rehearsal for Possible Blitz." The mayor of Boston imposed martial law. More than 300 victims—many of whom subsequently died--were taken to Boston City Hospital in one hour, averaging one victim every eleven seconds, while Massachusetts General Hospital admitted 114 victims in two hours. In the hospitals, 220 victims clung precariously to life, in agonizing pain from massive burns, their bodies ravaged by infection.
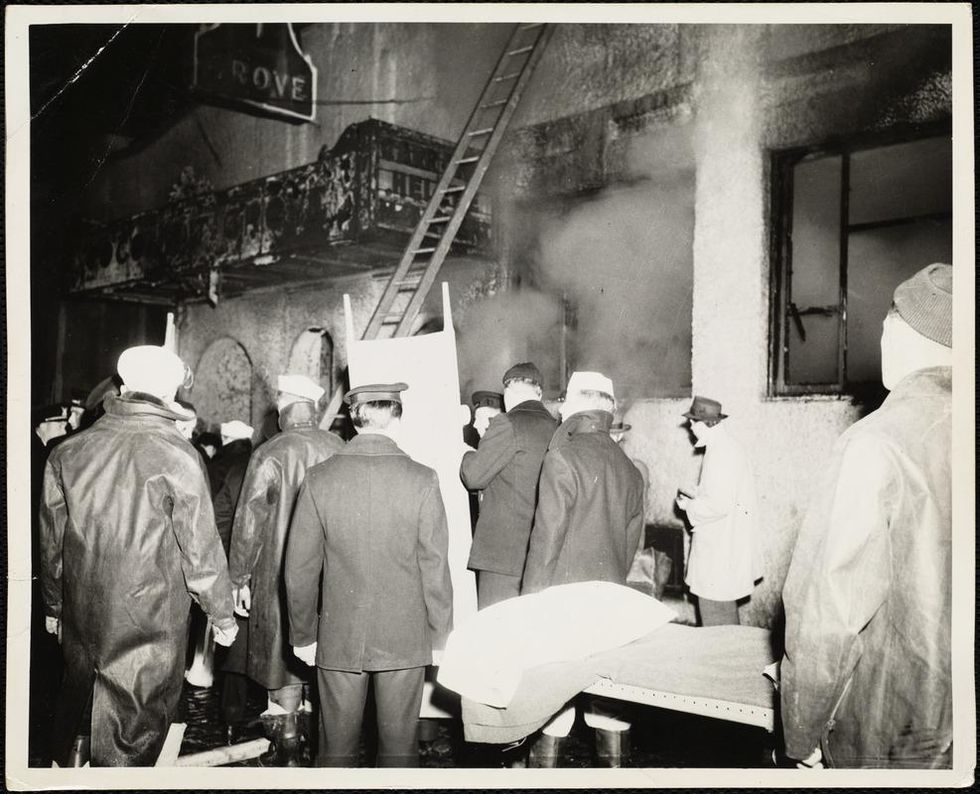
The scene of the fire.
Boston Public Library
Tragic Losses Prompted Revolutionary Leaps
But there is a silver lining: this horrific disaster prompted dramatic changes in safety regulations to prevent another catastrophe of this magnitude and led to the development of medical techniques that eventually saved millions of lives. It transformed burn care treatment and the use of plasma on burn victims, but most importantly, it introduced to the public a new wonder drug that revolutionized medicine, midwifed the birth of the modern pharmaceutical industry, and nearly doubled life expectancy, from 48 years at the turn of the 20th century to 78 years in the post-World War II years.
The devastating grief of the survivors also led to the first published study of post-traumatic stress disorder by pioneering psychiatrist Alexandra Adler, daughter of famed Viennese psychoanalyst Alfred Adler, who was a student of Freud. Dr. Adler studied the anxiety and depression that followed this catastrophe, according to the New York Times, and "later applied her findings to the treatment World War II veterans."
Dr. Ken Marshall is intimately familiar with the lingering psychological trauma of enduring such a disaster. His mother, an Irish immigrant and a nurse in the surgical wards at Boston City Hospital, was on duty that cold Thanksgiving weekend night, and didn't come home for four days. "For years afterward, she'd wake up screaming in the middle of the night," recalls Dr. Marshall, who was four years old at the time. "Seeing all those bodies lined up in neat rows across the City Hospital's parking lot, still in their evening clothes. It was always on her mind and memories of the horrors plagued her for the rest of her life."
The sheer magnitude of casualties prompted overwhelmed physicians to try experimental new procedures that were later successfully used to treat thousands of battlefield casualties. Instead of cutting off blisters and using dyes and tannic acid to treat burned tissues, which can harden the skin, they applied gauze coated with petroleum jelly. Doctors also refined the formula for using plasma--the fluid portion of blood and a medical technology that was just four years old--to replenish bodily liquids that evaporated because of the loss of the protective covering of skin.
"Every war has given us a new medical advance. And penicillin was the great scientific advance of World War II."
"The initial insult with burns is a loss of fluids and patients can die of shock," says Dr. Ken Marshall. "The scientific progress that was made by the two institutions revolutionized fluid management and topical management of burn care forever."
Still, they could not halt the staph infections that kill most burn victims—which prompted the first civilian use of a miracle elixir that was being secretly developed in government-sponsored labs and that ultimately ushered in a new age in therapeutics. Military officials quickly realized this disaster could provide an excellent natural laboratory to test the effectiveness of this drug and see if it could be used to treat the acute traumas of combat in this unfortunate civilian approximation of battlefield conditions. At the time, the very existence of this wondrous medicine—penicillin—was a closely guarded military secret.
From Forgotten Lab Experiment to Wonder Drug
In 1928, Alexander Fleming discovered the curative powers of penicillin, which promised to eradicate infectious pathogens that killed millions every year. But the road to mass producing enough of the highly unstable mold was littered with seemingly unsurmountable obstacles and it remained a forgotten laboratory curiosity for over a decade. But Fleming never gave up and penicillin's eventual rescue from obscurity was a landmark in scientific history.
In 1940, a group at Oxford University, funded in part by the Rockefeller Foundation, isolated enough penicillin to test it on twenty-five mice, which had been infected with lethal doses of streptococci. Its therapeutic effects were miraculous—the untreated mice died within hours, while the treated ones played merrily in their cages, undisturbed. Subsequent tests on a handful of patients, who were brought back from the brink of death, confirmed that penicillin was indeed a wonder drug. But Britain was then being ravaged by the German Luftwaffe during the Blitz, and there were simply no resources to devote to penicillin during the Nazi onslaught.
In June of 1941, two of the Oxford researchers, Howard Florey and Ernst Chain, embarked on a clandestine mission to enlist American aid. Samples of the temperamental mold were stored in their coats. By October, the Roosevelt Administration had recruited four companies—Merck, Squibb, Pfizer and Lederle—to team up in a massive, top-secret development program. Merck, which had more experience with fermentation procedures, swiftly pulled away from the pack and every milligram they produced was zealously hoarded.
After the nightclub fire, the government ordered Merck to dispatch to Boston whatever supplies of penicillin that they could spare and to refine any crude penicillin broth brewing in Merck's fermentation vats. After working in round-the-clock relays over the course of three days, on the evening of December 1st, 1942, a refrigerated truck containing thirty-two liters of injectable penicillin left Merck's Rahway, New Jersey plant. It was accompanied by a convoy of police escorts through four states before arriving in the pre-dawn hours at Massachusetts General Hospital. Dozens of people were rescued from near-certain death in the first public demonstration of the powers of the antibiotic, and the existence of penicillin could no longer be kept secret from inquisitive reporters and an exultant public. The next day, the Boston Globe called it "priceless" and Time magazine dubbed it a "wonder drug."
Within fourteen months, penicillin production escalated exponentially, churning out enough to save the lives of thousands of soldiers, including many from the Normandy invasion. And in October 1945, just weeks after the Japanese surrender ended World War II, Alexander Fleming, Howard Florey and Ernst Chain were awarded the Nobel Prize in medicine. But penicillin didn't just save lives—it helped build some of the most innovative medical and scientific companies in history, including Merck, Pfizer, Glaxo and Sandoz.
"Every war has given us a new medical advance," concludes Marshall. "And penicillin was the great scientific advance of World War II."
Are the gains from gain-of-function research worth the risks?
Gain-of-function research can make pathogens more infectious and deadly. It also enables scientists to prepare remedies in advance.
Scientists have long argued that gain-of-function research, which can make viruses and other infectious agents more contagious or more deadly, was necessary to develop therapies and vaccines to counter the pathogens in case they were used for biological warfare. As the SARS-CoV-2 origins are being investigated, one prominent theory suggests it had leaked from a biolab that conducted gain-of-function research, causing a global pandemic that claimed nearly 6.9 million lives. Now some question the wisdom of engaging in this type of research, stating that the risks may far outweigh the benefits.
“Gain-of-function research means genetically changing a genome in a way that might enhance the biological function of its genes, such as its transmissibility or the range of hosts it can infect,” says George Church, professor of genetics at Harvard Medical School. This can occur through direct genetic manipulation as well as by encouraging mutations while growing successive generations of micro-organism in culture. “Some of these changes may impact pathogenesis in a way that is hard to anticipate in advance,” Church says.
In the wake of the global pandemic, the pros and cons of gain-of-function research are being fiercely debated. Some scientists say this type of research is vital for preventing future pandemics or for preparing for bioweapon attacks. Others consider it another disaster waiting to happen. The Government Accounting Office issued a report charging that a framework developed by the U.S. Department of Health & Human Services (HHS) provided inadequate oversight of this potentially deadly research. There’s a movement to stop it altogether. In January, the Viral Gain-of-Function Research Moratorium Act (S. 81) was introduced into the Senate to cease awarding federal research funding to institutions doing gain-of-function studies.
While testifying before the House COVID Origins Select Committee on March 8th, Robert Redfield, former director of the U.S. Centers for Disease Control and Prevention, said that COVID-19 may have resulted from an accidental lab leak involving gain-of-function research. Redfield said his conclusion is based upon the “rapid and high infectivity for human-to-human transmission, which then predicts the rapid evolution of new variants.”
“It is a very, very, very small subset of life science research that could potentially generate a potential pandemic pathogen,” said Gerald Parker, associate dean for Global One Health at Texas A&M University.
“In my opinion,” Redfield continues, “the COVID-19 pandemic presents a case study on the potential dangers of such research. While many believe that gain-of-function research is critical to get ahead of viruses by developing vaccines, in this case, I believe that was the exact opposite.” Consequently, Redfield called for a moratorium on gain-of-function research until there is consensus about the value of such risky science.
What constitutes risky?
The Federal Select Agent Program lists 68 specific infectious agents as risky because they are either very contagious or very deadly. In order to work with these 68 agents, scientists must register with the federal government. Meanwhile, research on deadly pathogens that aren’t easily transmitted, or pathogens that are quite contagious but not deadly, can be conducted without such oversight. “If you’re not working with select agents, you’re not required to register the research with the federal government,” says Gerald Parker, associate dean for Global One Health at Texas A&M University. But the 68-item list may not have everything that could possibly become dangerous or be engineered to be dangerous, thus escaping the government’s scrutiny—an issue that new regulations aim to address.
In January 2017, the White House Office of Science and Technology Policy (OSTP) issued additional guidance. It required federal departments and agencies to follow a series of steps when reviewing proposed research that could create, transfer, or use potential pandemic pathogens resulting from the enhancement of a pathogen’s transmissibility or virulence in humans.
In defining risky pathogens, OSTP included viruses that were likely to be highly transmissible and highly virulent, and thus very deadly. The Proposed Biosecurity Oversight Framework for the Future of Science, outlined in 2023, broadened the scope to require federal review of research “that is reasonably anticipated to enhance the transmissibility and/or virulence of any pathogen” likely to pose a threat to public health, health systems or national security. Those types of experiments also include the pathogens’ ability to evade vaccines or therapeutics, or diagnostic detection.
However, Parker says that dangers of generating a pandemic-level germ are tiny. “It is a very, very, very small subset of life science research that could potentially generate a potential pandemic pathogen.” Since gain-of-function guidelines were first issued in 2017, only three such research projects have met those requirements for HHS review. They aimed to study influenza and bird flu. Only two of those projects were funded, according to the NIH Office of Science Policy. For context, NIH funded approximately 11,000 of the 54,000 grant applications it received in 2022.
Guidelines governing gain-of-function research are being strengthened, but Church points out they aren’t ideal yet. “They need to be much clearer about penalties and avoiding positive uses before they would be enforceable.”
What do we gain from gain-of-function research?
The most commonly cited reason to conduct gain-of-function research is for biodefense—the government’s ability to deal with organisms that may pose threats to public health.
In the era of mRNA vaccines, the advance preparedness argument may be even less relevant.
“The need to work with potentially dangerous viruses is central to our preparedness,” Parker says. “It’s essential that we know and understand the basic biology, microbiology, etc. of some of these dangerous pathogens.” That includes increasing our knowledge of the molecular mechanisms by which a virus could become a sustained threat to humans. “Knowing that could help us detect [risks] earlier,” Parker says—and could make it possible to have medical countermeasures, like vaccines and therapeutics, ready.
Most vaccines, however, aren’t affected by this type of research. Essentially, scientists hope they will never need to use it. Moreover, Paul Mango, HSS former deputy chief of staff for policy, and author of the 2022 book Warp Speed, says he believes that in the era of mRNA vaccines, the advance preparedness argument may be even less relevant. “That’s because these vaccines can be developed and produced in less than 12 months, unlike traditional vaccines that require years of development,” he says.
Can better oversight guarantee safety?
Another situation, which Parker calls unnecessarily dangerous, is when regulatory bodies cannot verify that the appropriate biosafety and biosecurity controls are in place.
Gain-of-function studies, Parker points out, are conducted at the basic research level, and they’re performed in high-containment labs. “As long as all the processes, procedures and protocols are followed and there’s appropriate oversight at the institutional and scientific level, it can be conducted safely.”
Globally, there are 69 Biosafety Level 4 (BSL4) labs operating, under construction or being planned, according to recent research from King’s College London and George Mason University for Global BioLabs. Eleven of these 18 high-containment facilities that are planned or under construction are in Asia. Overall, three-quarters of the BSL4 labs are in cities, increasing public health risks if leaks occur.
Researchers say they are confident in the oversight system for BSL4 labs within the U.S. They are less confident in international labs. Global BioLabs’ report concurs. It gives the highest scores for biosafety to industrialized nations, led by France, Australia, Canada, the U.S. and Japan, and the lowest scores to Saudi Arabia, India and some developing African nations. Scores for biosecurity followed similar patterns.
“There are no harmonized international biosafety and biosecurity standards,” Parker notes. That issue has been discussed for at least a decade. Now, in the wake of SARS and the COVID-19 pandemic, scientists and regulators are likely to push for unified oversight standards. “It’s time we got serious about international harmonization of biosafety and biosecurity standards and guidelines,” Parker says. New guidelines are being worked on. The National Science Advisory Board for Biosecurity (NSABB) outlined its proposed recommendations in the document titled Proposed Biosecurity Oversight Framework for the Future of Science.
The debates about whether gain-of-function research is useful or poses unnecessary risks to humanity are likely to rage on for a while. The public too has a voice in this debate and should weigh in by communicating with their representatives in government, or by partaking in educational forums or initiatives offered by universities and other institutions. In the meantime, scientists should focus on improving the research regulations, Parker notes. “We need to continue to look for lessons learned and for gaps in our oversight system,” he says. “That’s what we need to do right now.”

The rise of remote work is a win-win for people with disabilities and employers
Disability advocates see remote work as a silver lining of the pandemic, a win-win for adults with disabilities and the business world alike.
Any corporate leader would jump at the opportunity to increase their talent pool of potential employees by 15 percent, with all these new hires belonging to an underrepresented minority. That’s especially true given tight labor markets and CEO desires to increase headcount. Yet, too few leaders realize that people with disabilities are the largest minority group in this country, numbering 50 million.
Some executives may dread the extra investments in accommodating people’s disabilities. Yet, providing full-time remote work could suffice, according to a new study by the Economic Innovation Group think tank. The authors found that the employment rate for people with disabilities did not simply reach the pre-pandemic level by mid-2022, but far surpassed it, to the highest rate in over a decade. “Remote work and a strong labor market are helping [individuals with disabilities] find work,” said Adam Ozimek, who led the research and is chief economist at the Economic Innovation Group.
Disability advocates see this development as a silver lining of the pandemic, a win-win for adults with disabilities and the business world alike. For decades before the pandemic, employers had refused requests from workers with disabilities to work remotely, according to Thomas Foley, executive director of the National Disability Institute. During the pandemic, "we all realized that...many of us could work remotely,” Foley says. “[T]hat was disproportionately positive for people with disabilities."
Charles-Edouard Catherine, director of corporate and government relations for the National Organization on Disability, said that remote-work options had been advocated for many years to accommodate disabilities. “It’s a little frustrating that for decades corporate America was saying it’s too complicated, we’ll lose productivity, and now suddenly it’s like, sure, let’s do it.”
The pandemic opened doors for people with disabilities
Early in the pandemic, employment rates dropped for everyone, including people with disabilities, according to Ozimek’s research. However, these rates recovered quickly. In the second quarter of 2022, people with disabilities aged 25 to 54, the prime working age, are 3.5 percent more likely to be employed, compared to before the pandemic.
What about people without disabilites? They are still 1.1 percent less likely to be employed.
These numbers suggest that remote work has enabled a substantial number of people with disabilities to find and retain employment.
“We have a last-in, first-out labor market, and [people with disabilities] are often among the last in and the first out,” Ozimek says. However, this dynamic has changed, with adults with disabilities seeing employment rates recover much faster. Now, the question is whether the new trend will endure, Ozimek adds. “And my conclusion is that not only is it a permanent thing, but it’s going to improve.”
Gene Boes, president and chief executive of the Northwest Center, a Seattle organization that helps people with disabilities become more independent, confirms this finding. “The new world we live in has opened the door a little bit more…because there’s just more demand for labor.”
Long COVID disabilities put a premium on remote work
Remote work can help mitigate the impact of long COVID. The U.S. Centers for Disease Control and Prevention reports that about 19 percent of those who had COVID developed long COVID. Recent Census Bureau data indicates that 16 million working age Americans suffer from it, with economic costs estimated at $3.7 trillion.
Certainly, many of these so-called long-haulers experience relatively mild symptoms - such as loss of smell - which, while troublesome, are not disabling. But other symptoms are serious enough to be disabilities.
According to a recent study from the Federal Reserve Bank of Minneapolis, about a quarter of those with long COVID changed their employment status or working hours. That means long COVID was serious enough to interfere with work for 4 million people. For many, the issue was serious enough to qualify them as disabled.
Indeed, the Federal Reserve Bank of New York found in a just-released study that the number of individuals with disabilities in the U.S. grew by 1.7 million. That growth stemmed mainly from long COVID conditions such as fatigue and brain fog, meaning difficulties with concentration or memory, with 1.3 million people reporting an increase in brain fog since mid-2020.
Many had to drop out of the labor force due to long COVID. Yet, about 900,000 people who are newly disabled have managed to continue working. Without remote work, they might have lost these jobs.
For example, a software engineer at one of my client companies has struggled with brain fog related to long COVID. With remote work, this employee can work during the hours when she feels most mentally alert and focused, even if that means short bursts of productivity throughout the day. With flexible scheduling, she can take rests, meditate, or engage in activities that help her regain focus and energy. Without the need to commute to the office, she can save energy and time and reduce stress, which is crucial when dealing with brain fog.
In fact, the author of the Federal Reserve Bank of New York study notes that long COVID can be considered a disability under the Americans with Disability Act, depending on the specifics of the condition. That means the law can require private employers with fifteen or more staff, as well as government agencies, to make reasonable accommodations for those with long COVID. Richard Deitz, the author of this study, writes in the paper that “telework and flexible scheduling are two accommodations that can be particularly beneficial for workers dealing with fatigue and brain fog.”
The current drive to return to the office, led by many C-suite executives, may need to be reconsidered in light of legal and HR considerations. Arlene S. Kanter, director of the disability law and policy program at the Syracuse University College of Law, said that the question should depend on whether people with disabilities can perform their work well at home, as they did during Covid outbreaks. “[T]hen people with disabilities, as a matter of accommodation, shouldn’t be denied that right,” Kanter said.
Diversity benefits
But companies shouldn’t need to worry about legal regulations. It simply makes dollars and sense to expand their talent pool by 15% of an underrepresented minority. After all, extensive research shows that improving diversity boosts both decision-making and financial performance.
Companies that are offering more flexible work options have already gained significant benefits in terms of diverse hires. In its efforts to adapt to the post-pandemic environment, Meta, the owner of Facebook and Instagram, decided to offer permanent fully remote work options to its entire workforce. And according to Meta chief diversity officer Maxine Williams, the candidates who accepted job offers for remote positions were “substantially more likely” to come from diverse communities: people with disabilities, Black, Hispanic, Alaskan Native, Native American, veterans, and women. The numbers bear out these claims: people with disabilities increased from 4.7 to 6.2 percent of Meta’s employees.
Having consulted for 21 companies to help them transition to hybrid work arrangements, I can confirm that Meta’s numbers aren’t a fluke. The more my clients proved willing to offer remote work, the more staff with disabilities they recruited - and retained. That includes employees with mobility challenges. But it also includes employees with less visible disabilities, such as people with long COVID and immunocompromised people who feel reluctant to put themselves at risk of getting COVID by coming into the office.
Unfortunately, many leaders fail to see the benefits of remote work for underrepresented groups, such as those with disabilities. Some even say the opposite is true, with JP Morgan CEO Jamie Dimon claiming that returning to the office will aid diversity.
What explains this poor executive decision making? Part of the answer comes from a mental blindspot called the in-group bias. Our minds tend to favor and pay attention to the concerns of those in the group of people who seem to look and think like us. Dimon and other executives without disabilities don’t perceive people with disabilities to be part of their in-group. They thus are blind to the concerns of those with disabilities, which leads to misperceptions such as Dimon’s that returning to the office will aid diversity.
In-group bias is one of many dangerous judgment errors known as cognitive biases. They impact decision making in all life areas, ranging from the future of work to relationships.
Another relevant cognitive bias is the empathy gap. This term refers to our difficulty empathizing with those outside of our in-group. The lack of empathy combines with the blindness from the in-group bias, causing executives to ignore the feelings of employees with disabilities and prospective hires.
Omission bias also plays a role. This dangerous judgment error causes us to perceive failure to act as less problematic than acting. Consequently, executives perceive a failure to support the needs of those with disabilities as a minor matter.
Conclusion
The failure to empower people with disabilities through remote work options will prove costly to the bottom lines of companies. Not only are limiting their talent pool by 15 percent, they’re harming their ability to recruit and retain diverse candidates. And as their lawyers and HR departments will tell them, by violating the ADA, they are putting themselves in legal jeopardy.
By contrast, companies like Meta - and my clients - that offer remote work opportunities are seizing a competitive advantage by recruiting these underrepresented candidates. They’re lowering costs of labor while increasing diversity. The future belongs to the savvy companies that offer the flexibility that people with disabilities need.