How old fishing nets turn into chairs, car mats and Prada bags

A company called Aquafil is turning the fibers from fishing nets and old carpets into new threads for chairs, car mats, bikinis and Prada bags.
Discarded nylon fishing nets in the oceans are among the most harmful forms of plastic pollution. Every year, about 640,000 tons of fishing gear are left in our oceans and other water bodies to turn into death traps for marine life. London-based non-profit World Animal Protection estimates that entanglement in this “ghost gear” kills at least 136,000 seals, sea lions and large whales every year. Experts are challenged to estimate how many birds, turtles, fish and other species meet the same fate because the numbers are so high.
Since 2009, Giulio Bonazzi, the son of a small textile producer in northern Italy, has been working on a solution: an efficient recycling process for nylon. As CEO and chairman of a company called Aquafil, Bonazzi is turning the fibers from fishing nets – and old carpets – into new threads for car mats, Adidas bikinis, environmentally friendly carpets and Prada bags.
For Bonazzi, shifting to recycled nylon was a question of survival for the family business. His parents founded a textile company in 1959 in a garage in Verona, Italy. Fifteen years later, they started Aquafil to produce nylon for making raincoats, an enterprise that led to factories on three continents. But before the turn of the century, cheap products from Asia flooded the market and destroyed Europe’s textile production. When Bonazzi had finished his business studies and prepared to take over the family company, he wondered how he could produce nylon, which is usually produced from petrochemicals, in a way that was both successful and ecologically sustainable.
The question led him on an intellectual journey as he read influential books by activists such as world-renowned marine biologist Sylvia Earle and got to know Michael Braungart, who helped develop the Cradle-to-Cradle ethos of a circular economy. But the challenges of applying these ideologies to his family business were steep. Although fishing nets have become a mainstay of environmental fashion ads—and giants like Dupont and BASF have made breakthroughs in recycling nylon—no one had been able to scale up these efforts.
For ten years, Bonazzi tinkered with ideas for a proprietary recycling process. “It’s incredibly difficult because these products are not made to be recycled,” Bonazzi says. One complication is the variety of materials used in older carpets. “They are made to be beautiful, to last, to be useful. We vastly underestimated the difficulty when we started.”
Soon it became clear to Bonazzi that he needed to change the entire production process. He found a way to disintegrate old fibers with heat and pull new strings from the discarded fishing nets and carpets. In 2022, his company Aquafil produced more than 45,000 tons of Econyl, which is 100% recycled nylon, from discarded waste.
More than half of Aquafil’s recyclate is from used goods. According to the company, the recycling saves 90 percent of the CO2 emissions compared to the production of conventional nylon. That amounts to saving 57,100 tons of CO2 equivalents for every 10,000 tons of Econyl produced.
Bonazzi collects fishing nets from all over the world, including Norway and Chile—which have the world’s largest salmon productions—in addition to the Mediterranean, Turkey, India, Japan, Thailand, the Philippines, Pakistan, and New Zealand. He counts the government leadership of Seychelles as his most recent client; the island has prohibited ships from throwing away their fishing nets, creating the demand for a reliable recycler. With nearly 3,000 employees, Aquafil operates almost 40 collection and production sites in a dozen countries, including four collection sites for old carpets in the U.S., located in California and Arizona.
First, the dirty nets are gathered, washed and dried. Bonazzi explains that nets often have been treated with antifouling agents such as copper oxide. “We recycle the coating separately,” he says via Zoom from his home near Verona. “Copper oxide is a useful substance, why throw it away?”
Still, only a small percentage of Aquafil’s products are made from nets fished out of the ocean, so your new bikini may not have saved a strangled baby dolphin. “Generally, nylon recycling is a good idea,” says Christian Schiller, the CEO of Cirplus, the largest global marketplace for recyclates and plastic waste. “But contrary to what consumers think, people rarely go out to the ocean to collect ghost nets. Most are old, discarded nets collected on land. There’s nothing wrong with this, but I find it a tad misleading to label the final products as made from ‘ocean plastic,’ prompting consumers to think they’re helping to clean the oceans by buying these products.”
Aquafil gets most of its nets from aqua farms. Surprisingly, one of Aquafil’s biggest problems is finding enough waste. “I know, it’s hard to believe because waste is everywhere,” Bonazzi says. “But we need to find it in reliable quantity and quality.” He has invested millions in establishing reliable logistics to source the fishing nets. Then the nets get shredded into granules that can be turned into car mats for the new Hyundai Ioniq 5 or a Gucci swimsuit.
The process works similarly with carpets. In the U.S. alone, 3.5 billion pounds of carpet are discarded in landfills every year, and less than 3 percent are currently recycled. Aquafil has built a recycling plant in Phoenix to help divert 12,500 tons of carpets from the landfill every year. The carpets are shredded and deconstructed into three components: fillers such as calcium carbonate will be reused in the cement industry, synthetic fibers like polypropylene can be used for engineering plastics, and nylon. Only the pelletized nylon gets shipped back to Europe for the production of Econyl. “We ship only what’s necessary,” Bonazzi says. Nearly 50 percent of his nylon in Italy and Slovenia is produced from recyclate, and he hopes to increase the percentage to two-thirds in the next two years.
His clients include Interface, the leading world pioneer for sustainable flooring, and many other carpet producers plus more than 2500 fashion labels, including Gucci, Prada, Patagonia, Louis Vuitton, Adidas and Stella McCartney. “Stella McCartney just introduced a parka that’s made 100 percent from Econyl,” Bonazzi says. “We’re also in a lot of sportswear because Nylon is a good fabric for swimwear and for yoga clothes.” Next, he’s looking into sunglasses and chairs made with Econyl - for instance, the flexible ergonomic noho chair, designed by New Zealand company Formway.
“When I look at a landfill, I see a gold mine," Bonazzi says.
“Bonazzi decided many years ago to invest in the production of recycled nylon though industry giants halted similar plans after losing large investments,” says Anika Herrmann, vice president of the German Greentech-competitor Camm Solutions, which creates bio-based polymers from cane sugar and other ag waste. “We need role models like Bonazzi who create sustainable solutions with courage and a pioneering spirit. Like Aquafil, we count on strategic partnerships to enable fast upscaling along the entire production chain.”
Bonazzi’s recycled nylon is still five to 10 percent more expensive than conventionally produced material. However, brands are increasingly bending to the pressure of eco-conscious consumers who demand sustainable fashion. What helped Bonazzi was the recent rise of oil prices and the pressure on industries to reduce their carbon footprint. Now Bonazzi says, “When I look at a landfill, I see a gold mine.”
Ideally, the manufacturers take the products back when the client is done with it, and because the nylon can theoretically be reused nearly infinitely, the chair or bikini could be made into another chair or bikini. “But honestly,” Bonazzi half-jokes, “if someone returns a McCartney parka to me, I’ll just resell it because it’s so expensive.”
The next step: Bonazzi wants to reshape the entire nylon industry by pivoting from post-consumer nylon to plant-based nylon. In 2017, he began producing “nylon-6,” together with Genomatica in San Diego. The process uses sugar instead of petroleum. “The idea is to make the very same molecule from sugar, not from oil,” he says. The demonstration plant in Ljubljana, Slovenia, has already produced several hundred tons of nylon, and Genomatica is collaborating with Lululemon to produce plant-based yoga wear.
Bonazzi acknowledges that his company needs a few more years before the technology is ready to meet his ultimate goal, producing only recyclable products with no petrochemicals, low emissions and zero waste on an industrial scale. “Recycling is not enough,” he says. “You also need to produce the primary material in a sustainable way, with a low carbon footprint.”
A company in England has made a test that picks out the compounds from breath that reveal if people have liver disease.
Every year, around two million people worldwide die of liver disease. While some people inherit the disease, it’s most commonly caused by hepatitis, obesity and alcoholism. These underlying conditions kill liver cells, causing scar tissue to form until eventually the liver cannot function properly. Since 1979, deaths due to liver disease have increased by 400 percent.
The sooner the disease is detected, the more effective treatment can be. But once symptoms appear, the liver is already damaged. Around 50 percent of cases are diagnosed only after the disease has reached the final stages, when treatment is largely ineffective.
To address this problem, Owlstone Medical, a biotech company in England, has developed a breath test that can detect liver disease earlier than conventional approaches. Human breath contains volatile organic compounds (VOCs) that change in the first stages of liver disease. Owlstone’s breath test can reliably collect, store and detect VOCs, while picking out the specific compounds that reveal liver disease.
“There’s a need to screen more broadly for people with early-stage liver disease,” says Owlstone’s CEO Billy Boyle. “Equally important is having a test that's non-invasive, cost effective and can be deployed in a primary care setting.”
The standard tool for detection is a biopsy. It is invasive and expensive, making it impractical to use for people who aren't yet symptomatic. Meanwhile, blood tests are less invasive, but they can be inaccurate and can’t discriminate between different stages of the disease.
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
The team is testing patients in the early stages of advanced liver disease, or cirrhosis, to identify and detect these biomarkers. In an initial study, Owlstone’s breathalyzer was able to pick out patients who had early cirrhosis with 83 percent sensitivity.
Boyle’s work is personally motivated. His wife died of colorectal cancer after she was diagnosed with a progressed form of the disease. “That was a big impetus for me to see if this technology could work in early detection,” he says. “As a company, Owlstone is interested in early detection across a range of diseases because we think that's a way to save lives and a way to save costs.”
How it works
In the past, breath tests have not been widely used because of the difficulties of reliably collecting and storing breath. But Owlstone’s technology could help change that.
Study participants breathe into a mouthpiece attached to a breath sampler developed by Owlstone. It has cartridges are designed and optimized to collect gases. The sampler specifically targets VOCs, extracting them from atmospheric gases in breath, to ensure that even low levels of these compounds are captured.
The sampler can store compounds stably before they are assessed through a method called mass spectrometry, in which compounds are converted into charged atoms, before electromagnetic fields filter and identify even the tiniest amounts of charged atoms according to their weight and charge.
The top four compounds in our breath
In an initial study, Owlstone captured VOCs in breath to see which ones could help them tell the difference between people with and without liver disease. They tested the breath of 46 patients with liver disease - most of them in the earlier stages of cirrhosis - and 42 healthy people. Using this data, they were able to create a diagnostic model. Individually, compounds like 2-Pentanone and limonene performed well as markers for liver disease. Owlstone achieved even better performance by examining the levels of the top four compounds together, distinguishing between liver disease cases and controls with 95 percent accuracy.
“It was a good proof of principle since it looks like there are breath biomarkers that can discriminate between diseases,” Boyle says. “That was a bit of a stepping stone for us to say, taking those identified, let’s try and dose with specific concentrations of probes. It's part of building the evidence and steering the clinical trials to get to liver disease sensitivity.”
Sabine Szunerits, a professor of chemistry in Institute of Electronics at the University of Lille, sees the potential of Owlstone’s technology.
“Breath analysis is showing real promise as a clinical diagnostic tool,” says Szunerits, who has no ties with the company. “Owlstone Medical’s technology is extremely effective in collecting small volatile organic biomarkers in the breath. In combination with pattern recognition it can give an answer on liver disease severity. I see it as a very promising way to give patients novel chances to be cured.”
Improving the breath sampling process
Challenges remain. With more than one thousand VOCs found in the breath, it can be difficult to identify markers for liver disease that are consistent across many patients.
Julian Gardner is a professor of electrical engineering at Warwick University who researches electronic sensing devices. “Everyone’s breath has different levels of VOCs and different ones according to gender, diet, age etc,” Gardner says. “It is indeed very challenging to selectively detect the biomarkers in the breath for liver disease.”
So Owlstone is putting chemicals in the body that they know interact differently with patients with liver disease, and then using the breath sampler to measure these specific VOCs. The chemicals they administer are called Exogenous Volatile Organic Compound) probes, or EVOCs.
Most recently, they used limonene as an EVOC probe, testing 29 patients with early cirrhosis and 29 controls. They gave the limonene to subjects at specific doses to measure how its concentrations change in breath. The aim was to try and see what was happening in their livers.
“They are proposing to use drugs to enhance the signal as they are concerned about the sensitivity and selectivity of their method,” Gardner says. “The approach of EVOC probes is probably necessary as you can then eliminate the person-to-person variation that will be considerable in the soup of VOCs in our breath.”
Through these probes, Owlstone could identify patients with liver disease with 83 percent sensitivity. By targeting what they knew was a disease mechanism, they were able to amplify the signal. The company is starting a larger clinical trial, and the plan is to eventually use a panel of EVOC probes to make sure they can see diverging VOCs more clearly.
“I think the approach of using probes to amplify the VOC signal will ultimately increase the specificity of any VOC breath tests, and improve their practical usability,” says Roger Yazbek, who leads the South Australian Breath Analysis Research (SABAR) laboratory in Flinders University. “Whilst the findings are interesting, it still is only a small cohort of patients in one location.”
The future of breath diagnosis
Owlstone wants to partner with pharmaceutical companies looking to learn if their drugs have an effect on liver disease. They’ve also developed a microchip, a miniaturized version of mass spectrometry instruments, that can be used with the breathalyzer. It is less sensitive but will enable faster detection.
Boyle says the company's mission is for their tests to save 100,000 lives. "There are lots of risks and lots of challenges. I think there's an opportunity to really establish breath as a new diagnostic class.”
Doctors worry that fungal pathogens may cause the next pandemic.
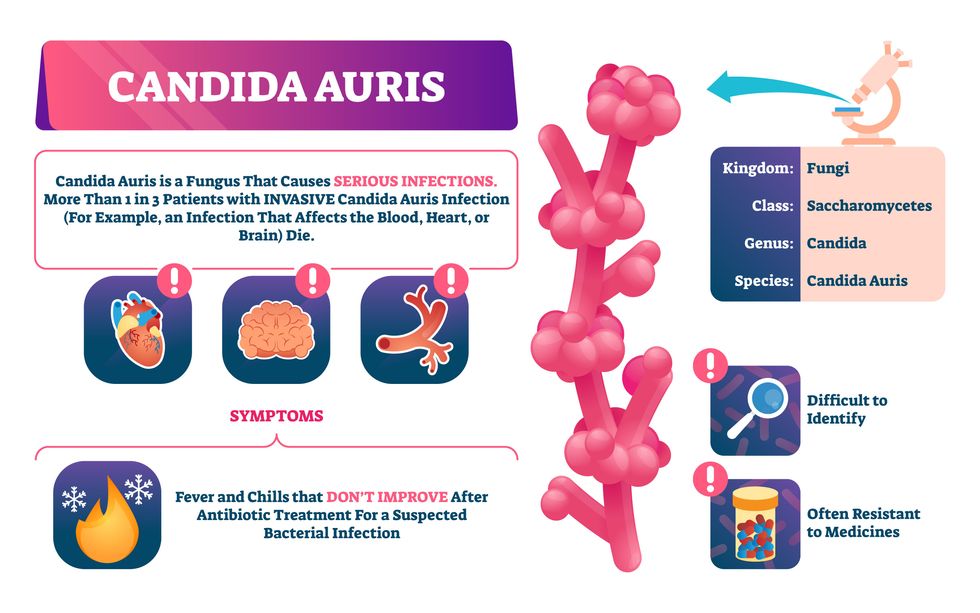
Bacterial antibiotic resistance has been a concern in the medical field for several years. Now a new, similar threat is arising: drug-resistant fungal infections. The Centers for Disease Control and Prevention considers antifungal and antimicrobial resistance to be among the world’s greatest public health challenges.
One particular type of fungal infection caused by Candida auris is escalating rapidly throughout the world. And to make matters worse, C. auris is becoming increasingly resistant to current antifungal medications, which means that if you develop a C. auris infection, the drugs your doctor prescribes may not work. “We’re effectively out of medicines,” says Thomas Walsh, founding director of the Center for Innovative Therapeutics and Diagnostics, a translational research center dedicated to solving the antimicrobial resistance problem. Walsh spoke about the challenges at a Demy-Colton Virtual Salon, one in a series of interactive discussions among life science thought leaders.
Although C. auris typically doesn’t sicken healthy people, it afflicts immunocompromised hospital patients and may cause severe infections that can lead to sepsis, a life-threatening condition in which the overwhelmed immune system begins to attack the body’s own organs. Between 30 and 60 percent of patients who contract a C. auris infection die from it, according to the CDC. People who are undergoing stem cell transplants, have catheters or have taken antifungal or antibiotic medicines are at highest risk. “We’re coming to a perfect storm of increasing resistance rates, increasing numbers of immunosuppressed patients worldwide and a bug that is adapting to higher temperatures as the climate changes,” says Prabhavathi Fernandes, chair of the National BioDefense Science Board.
Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures.
Although medical professionals aren’t concerned at this point about C. auris evolving to affect healthy people, they worry that its presence in hospitals can turn routine surgeries into life-threatening calamities. “It’s coming,” says Fernandes. “It’s just a matter of time.”
An emerging global threat
“Fungi are found in the environment,” explains Fernandes, so Candida spores can easily wind up on people’s skin. In hospitals, they can be transferred from contact with healthcare workers or contaminated surfaces. Most Candida species aren’t well-adapted to our body temperatures so they aren’t a threat. C. auris, however, thrives at human body temperatures. It can enter the body during medical treatments that break the skin—and cause an infection. Overall, fungal infections cost some $48 billion in the U.S. each year. And infection rates are increasing because, in an ironic twist, advanced medical therapies are enabling severely ill patients to live longer and, therefore, be exposed to this pathogen.
The first-ever case of a C. auris infection was reported in Japan in 2009, although an analysis of Candida samples dated the earliest strain to a 1996 sample from South Korea. Since then, five separate varieties – called clades, which are similar to strains among bacteria – developed independently in different geographies: South Asia, East Asia, South Africa, South America and, recently, Iran. So far, C. auris infections have been reported in 35 countries.
In the U.S., the first infection was reported in 2016, and the CDC started tracking it nationally two years later. During that time, 5,654 cases have been reported to the CDC, which only tracks U.S. data.
What’s more notable than the number of cases is their rate of increase. In 2016, new cases increased by 175 percent and, on average, they have approximately doubled every year. From 2016 through 2022, the number of infections jumped from 63 to 2,377, a roughly 37-fold increase.
“This reminds me of what we saw with epidemics from 2013 through 2020… with Ebola, Zika and the COVID-19 pandemic,” says Robin Robinson, CEO of Spriovas and founding director of the Biomedical Advanced Research and Development Authority (BARDA), which is part of the U.S. Department of Health and Human Services. These epidemics started with a hockey stick trajectory, Robinson says—a gradual growth leading to a sharp spike, just like the shape of a hockey stick.
Another challenge is that right now medics don’t have rapid diagnostic tests for fungal infections. Currently, patients are often misdiagnosed because C. auris resembles several other easily treated fungi. Or they are diagnosed long after the infection begins and is harder to treat.
The problem is that existing diagnostics tests can only identify C. auris once it reaches the bloodstream. Yet, because this pathogen infects bodily tissues first, it should be possible to catch it much earlier before it becomes life-threatening. “We have to diagnose it before it reaches the bloodstream,” Walsh says.
The most alarming fact is that some Candida infections no longer respond to standard therapeutics.
“We need to focus on rapid diagnostic tests that do not rely on a positive blood culture,” says John Sperzel, president and CEO of T2 Biosystems, a company specializing in diagnostics solutions. Blood cultures typically take two to three days for the concentration of Candida to become large enough to detect. The company’s novel test detects about 90 percent of Candida species within three to five hours—thanks to its ability to spot minute quantities of the pathogen in blood samples instead of waiting for them to incubate and proliferate.
Unlike other Candida species C. auris thrives at human body temperatures
Adobe Stock
Tackling the resistance challenge
The most alarming fact is that some Candida infections no longer respond to standard therapeutics. The number of cases that stopped responding to echinocandin, the first-line therapy for most Candida infections, tripled in 2020, according to a study by the CDC.
Now, each of the first four clades shows varying levels of resistance to all three commonly prescribed classes of antifungal medications, such as azoles, echinocandins, and polyenes. For example, 97 percent of infections from C. auris Clade I are resistant to fluconazole, 54 percent to voriconazole and 30 percent of amphotericin. Nearly half are resistant to multiple antifungal drugs. Even with Clade II fungi, which has the least resistance of all the clades, 11 to 14 percent have become resistant to fluconazole.
Anti-fungal therapies typically target specific chemical compounds present on fungi’s cell membranes, but not on human cells—otherwise the medicine would cause damage to our own tissues. Fluconazole and other azole antifungals target a compound called ergosterol, preventing the fungal cells from replicating. Over the years, however, C. auris evolved to resist it, so existing fungal medications don’t work as well anymore.
A newer class of drugs called echinocandins targets a different part of the fungal cell. “The echinocandins – like caspofungin – inhibit (a part of the fungi) involved in making glucan, which is an essential component of the fungal cell wall and is not found in human cells,” Fernandes says. New antifungal treatments are needed, she adds, but there are only a few magic bullets that will hit just the fungus and not the human cells.
Research to fight infections also has been challenged by a lack of government support. That is changing now that BARDA is requesting proposals to develop novel antifungals. “The scope includes C. auris, as well as antifungals following a radiological/nuclear emergency, says BARDA spokesperson Elleen Kane.
The remaining challenge is the number of patients available to participate in clinical trials. Large numbers are needed, but the available patients are quite sick and often die before trials can be completed. Consequently, few biopharmaceutical companies are developing new treatments for C. auris.
ClinicalTrials.gov reports only two drugs in development for invasive C. auris infections—those than can spread throughout the body rather than localize in one particular area, like throat or vaginal infections: ibrexafungerp by Scynexis, Inc., fosmanogepix, by Pfizer.
Scynexis’ ibrexafungerp appears active against C. auris and other emerging, drug-resistant pathogens. The FDA recently approved it as a therapy for vaginal yeast infections and it is undergoing Phase III clinical trials against invasive candidiasis in an attempt to keep the infection from spreading.
“Ibreafungerp is structurally different from other echinocandins,” Fernandes says, because it targets a different part of the fungus. “We’re lucky it has activity against C. auris.”
Pfizer’s fosmanogepix is in Phase II clinical trials for patients with invasive fungal infections caused by multiple Candida species. Results are showing significantly better survival rates for people taking fosmanogepix.
Although C. auris does pose a serious threat to healthcare worldwide, scientists try to stay optimistic—because they recognized the problem early enough, they might have solutions in place before the perfect storm hits. “There is a bit of hope,” says Robinson. “BARDA has finally been able to fund the development of new antifungal agents and, hopefully, this year we can get several new classes of antifungals into development.”

