Roald Dahl lost a child to measles. Here's what he has to say about the new outbreaks.

Olivia Dahl, shortly before her death from measles in 1962.
In 1962, the world was a remarkably different place: Neil Armstrong had yet to take his first steps on the lunar surface, John F. Kennedy was serving as president of the United States, and the Beatles were still a few years away from superstardom, having just recorded their first single.
The word “measles” was also a household name. Measles, which still exists in parts of the world today, is a highly contagious viral infection that typically causes fever, cough, muscle pain, fatigue, and a distinctive red rash. Measles was so pervasive around the world in 1962 that most children had gotten sick with it before the age of fifteen—but even though it was common, it was far from harmless. Measles killed around 400 to 500 people per year in the United States, and approximately 2.6 million people each year worldwide. Countless others suffered severe complications from measles, such as permanent blindness.
Tragedy hits home

Author Roald Dahl at his Buckinghamshire home with Olivia, daughter Chantal, and wife Patricia Neal in 1960.
Ben Martin / Getty Images
That year, British author Roald Dahl was beginning to make a name for himself, having just published his best-selling book James and the Giant Peach. Dahl, who would go on to write some of the most well-loved children’s books of the century, lived in southern England with his wife and three children. One day, Dahl and his wife, actress Patricia Neal, received word that there was an outbreak of measles at his daughters’ school.
While some parents quarantined their children, many others also considered measles a harmless childhood disease. Neal later recalled in her autobiography that a family member had advised her to “let the girls get measles,” thinking it would strengthen their immune systems and be “good for them.” Reluctantly, Dahl and Neal let their two school-aged children, Olivia and Chantal, continue school. Olivia, then aged seven, fell sick with the measles not long after that.
Neither Dahl nor Neal were terribly concerned about Olivia’s infection. Dahl would write later that it seemed to be taking its “usual course,” and the two would read and spend time together while Olivia rested. After a few days of fever and fatigue, Dahl wrote, Olivia seemed like she was “well on the road to recovery.”
But one afternoon, as the two sat on Olivia’s bed making animals out of pipe cleaners, Dahl noticed that Olivia’s “fingers and her mind were not working together.” When Dahl asked how she was feeling, Olivia replied, “I feel all sleepy.”
Within an hour, Dahl wrote, Olivia was unconscious. Within 12 hours, she was dead.
Olivia died of measles encephalitis, an inflammation of the brain caused by an infection. Approximately 1 in 1,000 people infected with measles develop encephalitis, and of those who develop it, between 10 and 20 percent will die.
Dahl was overcome with grief and wracked with guilt for being unable to prevent his daughter’s death. Mourning, Dahl threw himself into his writing and, in his spare time, spent hours lovingly constructing a rock garden on Olivia’s grave in a local churchyard.
After Olivia’s death, Dahl wrote sixteen novels and several collections of short stories, including Matilda, Fantastic Mr. Fox, and Willy Wonka and the Chocolate Factory, which garnered him worldwide acclaim. His most influential piece of writing, however, wasn’t written until 1986.
A father's plea
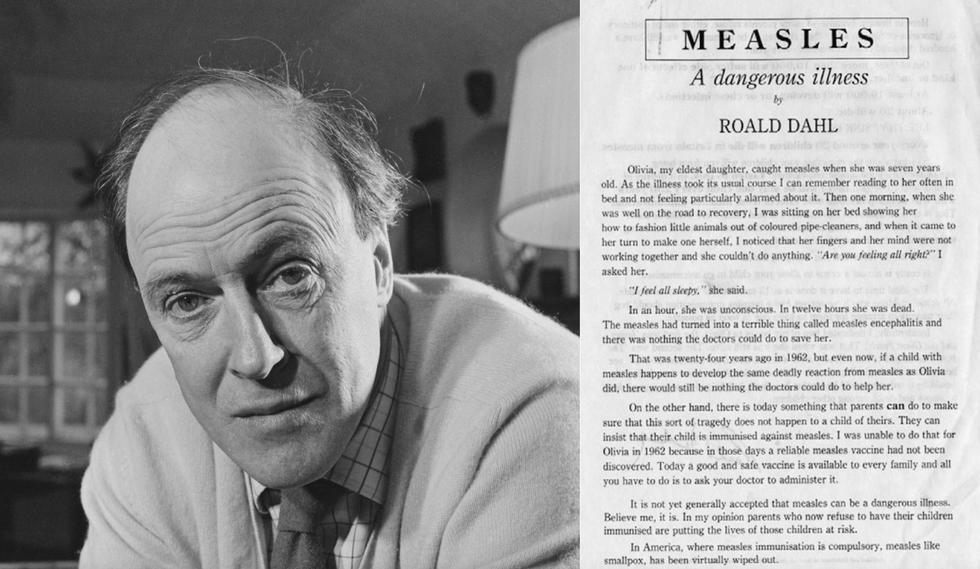
Roald Dahl and the open letter he wrote in 1986, encouraging parents to vaccinate their children against measles.
By 1986, measles was no longer the global health threat that it had been in the 1960s, thanks to a measles vaccine that became available just one year after Olivia had died. Still, in the United Kingdom alone, approximately 80,000 people every year were infected with measles. This bothered Dahl, especially since measles rates in the United States had dropped by 98 percent compared to pre-vaccine years. “Why do we have so much measles in Britain when the Americans have virtually gotten rid of it?,” Dahl was reported to have said.
So Dahl set out to prevent a tragedy like Olivia’s from happening again. With encouragement from several prominent public health activists, Dahl wrote an open letter addressed to parents in the UK. The letter recounted his daughter’s death from encephalitis and begged parents to protect their own children from measles:
“...there is today something that parents can do to make sure that this sort of tragedy does not happen to a child of theirs. They can insist that their child is immunised [sic] against measles. I was unable to do that for Olivia in 1962 because in those days a reliable measles vaccine had not been discovered. Today a good and safe vaccine is available to every family and all you have to do is to ask your doctor to administer it.”
Dahl went on to say that although many parents still viewed measles as a harmless illness, he knew from experience that it was not. Measles was capable of causing disability and death, Dahl wrote, whereas a child had a better chance of “choking on a chocolate bar” than developing any serious complication from the vaccine. Dahl ended his letter by saying how happy he knew Olivia would be “if only she could know that her death had helped to save a good deal of illness and death among other children.”
Dahl’s letter was published in early 1986 and distributed to local healthcare workers, schools, and to parents of children who were particularly at risk. As the letter circulated, vaccination rates continued to climb year after year.
Thirty-one years after Dahl’s letter was published, and 55 years after Olivia’s death, the World Health Organization declared in 2017 that measles had officially been eradicated for the first time in the UK thanks to high rates of vaccination.
A small step back

As vaccination rates decline, measles is now making a strong comeback in the United States and elsewhere.
Getty Images
Today, vaccination rates for the measles are in decline, and countries like the UK and the US, who had once eradicated measles completely, are now seeing a comeback. The Centers for Disease Control and Prevention (CDC) recently reported that between December 1, 2023 and January 23, 2024, 23 cases of measles had been confirmed across multiple states. The majority of these cases, they reported, were among children and adolescents who had traveled internationally and had not yet been vaccinated even though they were eligible to do so.
Roald Dahl passed away in 1990, but fortunately, his writing continues to live on. While readers can explore fantastical worlds through his novels and short stories, they can also look back to a reality when tragic deaths like Olivia’s happened far too often. The difference is that today, thanks to modern science, we now have the tools to stop them.
A new type of cancer therapy is shrinking deadly brain tumors with just one treatment
MRI scans after a new kind of immunotherapy for brain cancer show remarkable progress in one patient just days after the first treatment.
Few cancers are deadlier than glioblastomas—aggressive and lethal tumors that originate in the brain or spinal cord. Five years after diagnosis, less than five percent of glioblastoma patients are still alive—and more often, glioblastoma patients live just 14 months on average after receiving a diagnosis.
But an ongoing clinical trial at Mass General Cancer Center is giving new hope to glioblastoma patients and their families. The trial, called INCIPIENT, is meant to evaluate the effects of a special type of immune cell, called CAR-T cells, on patients with recurrent glioblastoma.
How CAR-T cell therapy works
CAR-T cell therapy is a type of cancer treatment called immunotherapy, where doctors modify a patient’s own immune system specifically to find and destroy cancer cells. In CAR-T cell therapy, doctors extract the patient’s T-cells, which are immune system cells that help fight off disease—particularly cancer. These T-cells are harvested from the patient and then genetically modified in a lab to produce proteins on their surface called chimeric antigen receptors (thus becoming CAR-T cells), which makes them able to bind to a specific protein on the patient’s cancer cells. Once modified, these CAR-T cells are grown in the lab for several weeks so that they can multiply into an army of millions. When enough cells have been grown, these super-charged T-cells are infused back into the patient where they can then seek out cancer cells, bind to them, and destroy them. CAR-T cell therapies have been approved by the US Food and Drug Administration (FDA) to treat certain types of lymphomas and leukemias, as well as multiple myeloma, but haven’t been approved to treat glioblastomas—yet.
CAR-T cell therapies don’t always work against solid tumors, such as glioblastomas. Because solid tumors contain different kinds of cancer cells, some cells can evade the immune system’s detection even after CAR-T cell therapy, according to a press release from Massachusetts General Hospital. For the INCIPIENT trial, researchers modified the CAR-T cells even further in hopes of making them more effective against solid tumors. These second-generation CAR-T cells (called CARv3-TEAM-E T cells) contain special antibodies that attack EFGR, a protein expressed in the majority of glioblastoma tumors. Unlike other CAR-T cell therapies, these particular CAR-T cells were designed to be directly injected into the patient’s brain.
The INCIPIENT trial results
The INCIPIENT trial involved three patients who were enrolled in the study between March and July 2023. All three patients—a 72-year-old man, a 74-year-old man, and a 57-year-old woman—were treated with chemo and radiation and enrolled in the trial with CAR-T cells after their glioblastoma tumors came back.
The results, which were published earlier this year in the New England Journal of Medicine (NEJM), were called “rapid” and “dramatic” by doctors involved in the trial. After just a single infusion of the CAR-T cells, each patient experienced a significant reduction in their tumor sizes. Just two days after receiving the infusion, the glioblastoma tumor of the 72-year-old man decreased by nearly twenty percent. Just two months later the tumor had shrunk by an astonishing 60 percent, and the change was maintained for more than six months. The most dramatic result was in the 57-year-old female patient, whose tumor shrank nearly completely after just one infusion of the CAR-T cells.
The results of the INCIPIENT trial were unexpected and astonishing—but unfortunately, they were also temporary. For all three patients, the tumors eventually began to grow back regardless of the CAR-T cell infusions. According to the press release from MGH, the medical team is now considering treating each patient with multiple infusions or prefacing each treatment with chemotherapy to prolong the response.
While there is still “more to do,” says co-author of the study neuro-oncologist Dr. Elizabeth Gerstner, the results are still promising. If nothing else, these second-generation CAR-T cell infusions may someday be able to give patients more time than traditional treatments would allow.
“These results are exciting but they are also just the beginning,” says Dr. Marcela Maus, a doctor and professor of medicine at Mass General who was involved in the clinical trial. “They tell us that we are on the right track in pursuing a therapy that has the potential to change the outlook for this intractable disease.”
A recent study in The Lancet Oncology showed that AI found 20 percent more cancers on mammogram screens than radiologists alone.
Since the early 2000s, AI systems have eliminated more than 1.7 million jobs, and that number will only increase as AI improves. Some research estimates that by 2025, AI will eliminate more than 85 million jobs.
But for all the talk about job security, AI is also proving to be a powerful tool in healthcare—specifically, cancer detection. One recently published study has shown that, remarkably, artificial intelligence was able to detect 20 percent more cancers in imaging scans than radiologists alone.
Published in The Lancet Oncology, the study analyzed the scans of 80,000 Swedish women with a moderate hereditary risk of breast cancer who had undergone a mammogram between April 2021 and July 2022. Half of these scans were read by AI and then a radiologist to double-check the findings. The second group of scans was read by two researchers without the help of AI. (Currently, the standard of care across Europe is to have two radiologists analyze a scan before diagnosing a patient with breast cancer.)
The study showed that the AI group detected cancer in 6 out of every 1,000 scans, while the radiologists detected cancer in 5 per 1,000 scans. In other words, AI found 20 percent more cancers than the highly-trained radiologists.

But even though the AI was better able to pinpoint cancer on an image, it doesn’t mean radiologists will soon be out of a job. Dr. Laura Heacock, a breast radiologist at NYU, said in an interview with CNN that radiologists do much more than simply screening mammograms, and that even well-trained technology can make errors. “These tools work best when paired with highly-trained radiologists who make the final call on your mammogram. Think of it as a tool like a stethoscope for a cardiologist.”
AI is still an emerging technology, but more and more doctors are using them to detect different cancers. For example, researchers at MIT have developed a program called MIRAI, which looks at patterns in patient mammograms across a series of scans and uses an algorithm to model a patient's risk of developing breast cancer over time. The program was "trained" with more than 200,000 breast imaging scans from Massachusetts General Hospital and has been tested on over 100,000 women in different hospitals across the world. According to MIT, MIRAI "has been shown to be more accurate in predicting the risk for developing breast cancer in the short term (over a 3-year period) compared to traditional tools." It has also been able to detect breast cancer up to five years before a patient receives a diagnosis.
The challenges for cancer-detecting AI tools now is not just accuracy. AI tools are also being challenged to perform consistently well across different ages, races, and breast density profiles, particularly given the increased risks that different women face. For example, Black women are 42 percent more likely than white women to die from breast cancer, despite having nearly the same rates of breast cancer as white women. Recently, an FDA-approved AI device for screening breast cancer has come under fire for wrongly detecting cancer in Black patients significantly more often than white patients.
As AI technology improves, radiologists will be able to accurately scan a more diverse set of patients at a larger volume than ever before, potentially saving more lives than ever.

