Paralyzed By Polio, This British Tea Broker Changed the Course Of Medical History Forever
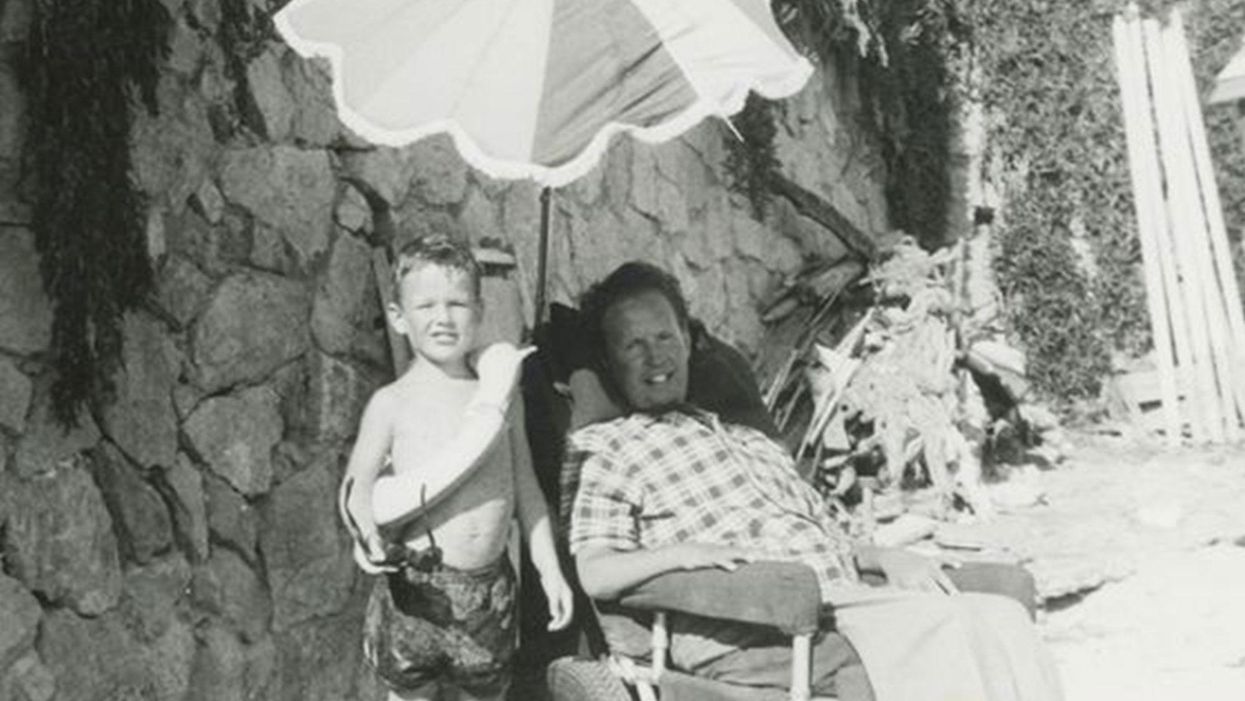
Robin Cavendish in his special wheelchair with his son Jonathan in the 1960s.
In December 1958, on a vacation with his wife in Kenya, a 28-year-old British tea broker named Robin Cavendish became suddenly ill. Neither he nor his wife Diana knew it at the time, but Robin's illness would change the course of medical history forever.
Robin was rushed to a nearby hospital in Kenya where the medical staff delivered the crushing news: Robin had contracted polio, and the paralysis creeping up his body was almost certainly permanent. The doctors placed Robin on a ventilator through a tracheotomy in his neck, as the paralysis from his polio infection had rendered him unable to breathe on his own – and going off the average life expectancy at the time, they gave him only three months to live. Robin and Diana (who was pregnant at the time with their first child, Jonathan) flew back to England so he could be admitted to a hospital. They mentally prepared to wait out Robin's final days.
But Robin did something unexpected when he returned to the UK – just one of many things that would astonish doctors over the next several years: He survived. Diana gave birth to Jonathan in February 1959 and continued to visit Robin regularly in the hospital with the baby. Despite doctors warning that he would soon succumb to his illness, Robin kept living.
After a year in the hospital, Diana suggested something radical: She wanted Robin to leave the hospital and live at home in South Oxfordshire for as long as he possibly could, with her as his nurse. At the time, this suggestion was unheard of. People like Robin who depended on machinery to keep them breathing had only ever lived inside hospital walls, as the prevailing belief was that the machinery needed to keep them alive was too complicated for laypeople to operate. But Diana and Robin were up for the challenges – and the risks. Because his ventilator ran on electricity, if the house were to unexpectedly lose power, Diana would either need to restore power quickly or hand-pump air into his lungs to keep him alive.
Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
In an interview as an adult, Jonathan Cavendish reflected on his parents' decision to live outside the hospital on a ventilator: "My father's mantra was quality of life," he explained. "He could have stayed in the hospital, but he didn't think that was as good of a life as he could manage. He would rather be two minutes away from death and living a full life."
After a few years of living at home, however, Robin became tired of being confined to his bed. He longed to sit outside, to visit friends, to travel – but had no way of doing so without his ventilator. So together with his friend Teddy Hall, a professor and engineer at Oxford University, the two collaborated in 1962 to create an entirely new invention: a battery-operated wheelchair prototype with a ventilator built in. With this, Robin could now venture outside the house – and soon the Cavendish family became famous for taking vacations. It was something that, by all accounts, had never been done before by someone who was ventilator-dependent. Robin and Hall also designed a van so that the wheelchair could be plugged in and powered during travel. Jonathan Cavendish later recalled a particular family vacation that nearly ended in disaster when the van broke down outside of Barcelona, Spain:
"My poor old uncle [plugged] my father's chair into the wrong socket," Cavendish later recalled, causing the electricity to short. "There was fire and smoke, and both the van and the chair ground to a halt." Johnathan, who was eight or nine at the time, his mother, and his uncle took turns hand-pumping Robin's ventilator by the roadside for the next thirty-six hours, waiting for Professor Hall to arrive in town and repair the van. Rather than being panicked, the Cavendishes managed to turn the vigil into a party. Townspeople came to greet them, bringing food and music, and a local priest even stopped by to give his blessing.
Robin had become a pioneer, showing the world that a person with severe disabilities could still have mobility, access, and a fuller quality of life than anyone had imagined. His mission, along with Hall's, then became gifting this independence to others like himself. Robin and Hall raised money – first from the Ernest Kleinwort Charitable Trust, and then from the British Department of Health – to fund more ventilator chairs, which were then manufactured by Hall's company, Littlemore Scientific Engineering, and given to fellow patients who wanted to live full lives at home. Robin and Hall used themselves as guinea pigs, testing out different models of the chairs and collaborating with scientists to create other devices for those with disabilities. One invention, called the Possum, allowed paraplegics to control things like the telephone and television set with just a nod of the head. Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
Robin went on to enjoy a long and happy life with his family at their house in South Oxfordshire, surrounded by friends who would later attest to his "down-to-earth" personality, his sense of humor, and his "irresistible" charm. When he died peacefully at his home in 1994 at age 64, he was considered the world's oldest-living person who used a ventilator outside the hospital – breaking yet another barrier for what medical science thought was possible.
Kids' immune systems come into contact with so many antigens every day that extra cleaning and disinfecting won't harm them, experts say.
Cleaning has taken on a whole new meaning in Frank Mosco's household during the COVID-19 pandemic. There's a protocol for everything he and his two teenage daughters do.
Experts agree that over-disinfecting is better than inadequate disinfecting, especially during a pandemic.
"We wipe down every package that comes into the house and the items inside," says Mosco, a technologist and social justice activist in Hastings-on-Hudson, N.Y. "If it's a fruit or vegetable, I use vinegar and water, or water and soap. Then we throw out the boxes, clean up the table, and wash our hands." Only then do they put items away.
As the novel coronavirus continues to pose an invisible threat, parents of infants to adolescents are pondering how vigorously and frequently to clean and disinfect surfaces at home and apply hand sanitizer in public. They also fret over whether there can be too much of a good thing: Will making everything as seemingly germ-free as possible reduce immunity down the road?
Experts agree that over-disinfecting is better than inadequate disinfecting, especially during a pandemic. Every family should assess their particular risks. Factors to consider include pre-existing medical conditions, the number of people living in the same home, and whether anyone works in a hospital or other virus-prone environment, says Kari Debbink, assistant professor of biology at Bowie State University in Bowie, Maryland.
Constantly cleaning everything in sight isn't necessary, she explains, because coronavirus tends to spread mainly via immediate contact with respiratory droplets—catching it from surfaces is a less-likely scenario. The longer the virus stays on a surface, the less contagious it becomes.
Some parents worry that their children's growing bodies may become accustomed to an environment that is "too clean." Debbink, a virologist, offers a salient reminder: "The immune system comes into contact with many, many different antigens every day, and it is 'trained' from birth onwards to respond to pathogens. Doing a little more cleansing and disinfecting during the pandemic will not weaken the immune system."
Other experts agree. "There should be no negative outcome to properly washing your hands more frequently," says Stacey Schultz-Cherry, an infectious diseases specialist at St. Jude Children's Research Hospital in Memphis, Tennessee. "Even with enhanced disinfection, kids are still getting exposed to immune-boosting microbes from playing outside, having pets, etc."
"There's no reason why hand sanitizer would weaken anyone's immune system of any age."
Applying hand sanitizer consisting of at least 60 percent alcohol helps clean hands while outdoors, says Angela Rasmussen, associate research scientist and a virologist at Columbia University's Mailman School of Public Health in New York. "There's no reason why hand sanitizer would weaken anyone's immune system of any age," she adds, and recommends moisturizer so hands don't dry out from frequent use. Meanwhile, "cleaning and disinfecting at home also don't have an impact on antiviral immunity, in kids or adults."
With the coronavirus foremost in parents' minds, Patricia Garcia, a pediatric hospitalist, has fielded many questions about how thoroughly they should wipe, rub, scrub, or mop. As medical director of Connecticut Children's Healthy Homes Program in Hartford, which takes aim at toxins and other housing hazards, she reassures them with this mantra: "You're never going to get it perfectly sterilized, and that's okay."
To quell some of these concerns, in March the U.S. Environmental Protection Agency (EPA) released a list of products for household use. None of these products have been specifically tested against SARS-CoV-2, the novel coronavirus that causes COVID-19. But the agency expects these products to be effective because they have demonstrated efficacy against a different human coronavirus similar to SARS-CoV-2 or an even harder-to-kill virus.
Many products on the list contain isopropyl alcohol or hydrogen peroxide. "When using an EPA-registered disinfectant," the agency's website instructs, "follow the label directions for safe, effective use. Make sure to follow the contact time, which is the amount of time the surface should be visibly wet."
Bear in mind that not all cleaners actually disinfect, cautions Alan Woolf, a pediatrician at Boston Children's Hospital who directs its environmental health center and is a professor at Harvard Medical School. Some cleaners remove visible dirt, grease, and grime, but they don't kill viruses. Disinfectants by their nature inactivate both bacteria and viruses. "That's an important distinction," Woolf says.
Frequently touched surfaces—for instance, doorknobs, light switches, toilet-flushing levers, and countertops—should not only be cleaned, but also disinfected at least daily during a pandemic if someone in the household is sick. The objects one touches upon coming home are the ones most likely to become contaminated with viruses, experts say.
Before bringing items inside, "it might be good to clear off a counter space where they will be placed," says Debbink, the biology professor and virologist. "This way, they come into contact with as few items and surfaces as possible."
If space permits, another option would be to set aside nonperishable items. "I've heard of some families putting things in a 'mud room' and closing the door for 48 hours, some leaving things in their garage or car trunk," says Stephanie Holm, co-director of the Western States Pediatric Environmental Health Specialty Unit at the University of California, San Francisco. "Letting new purchases sit for 48 hours undisturbed would greatly reduce the number of viable viruses present."
Cleaning surfaces is recommended before disinfecting them. Holm suggests using unscented soap and microfiber cloths instead of paper towels, which can transmit bacteria and viruses from one area to another.
Soap has the power to eradicate viruses with at least 20 seconds of contact time. It attacks the coronavirus's protective coat, explains infectious diseases specialist Schultz-Cherry. "If you destroy the coat, the virus is no longer infectious. Influenza virus is also very sensitive to soap."
"The most important thing that parents should do for children's immune systems is make sure they are up to date on all their vaccines."
For cribs, toys, and other mouth-contact surfaces, sanitizing with soap and water, not disinfectants, is advisable, says pediatrician Woolf. Fresh fruits and vegetables also can be cleaned with soap, removing dirt and pesticide residue, he adds.
"Some parents are nervous about using disinfectant on toys, which is understandable, considering many toys end up in children's mouths, so soap and water can be an alternative," says pediatrician Garcia, who recommends using hot water.
While some toys can go in the washing machine and dryer or dishwasher, others need to be cleaned by hand, with dish soap or a delicate detergent, as indicated on their labels. But toys with electrical components cannot be submerged in water, in which case consulting the EPA's list of disinfectants may be a parent's best option, she says.
Labels on the back of cleaning and disinfecting products also contain specific instructions. Not allowing a liquid to sit on a surface for the recommended time results in exposure to chemicals without even accomplishing the intended purpose of disinfection. For most household bleach-containing agents, the advisable "dwell time" is 10 minutes. "Many people don't realize this," says Holm, the environmental health specialist who also trained as a physician.
Beware of combining any type of cleaners or disinfectants that aren't already premixed. Doing so can release harmful gases into the air, she cautions.
During the pandemic, Mosco and his daughters have been very conscientious about decontaminating whatever comes through their doors. Mosco says he doesn't believe the family is overusing cleaning and disinfecting products. Although he's fastidious, he says, "a completely sterile environment is not the goal."
His mother, who was a nurse, instilled in him that exposure to some bacteria is a good thing. In turn, he "always encouraged his kids to play with animals, and to have fun in sand and dirt, with plenty of sunlight to keep their immune systems strong."
Even though a vaccine for coronavirus currently doesn't exist, parents can take some comfort in the best weapon available today to protect kids from deadly pathogens: "The most important thing that parents should do for children's immune systems," says virologist Rasmussen, "is make sure they are up to date on all their vaccines."
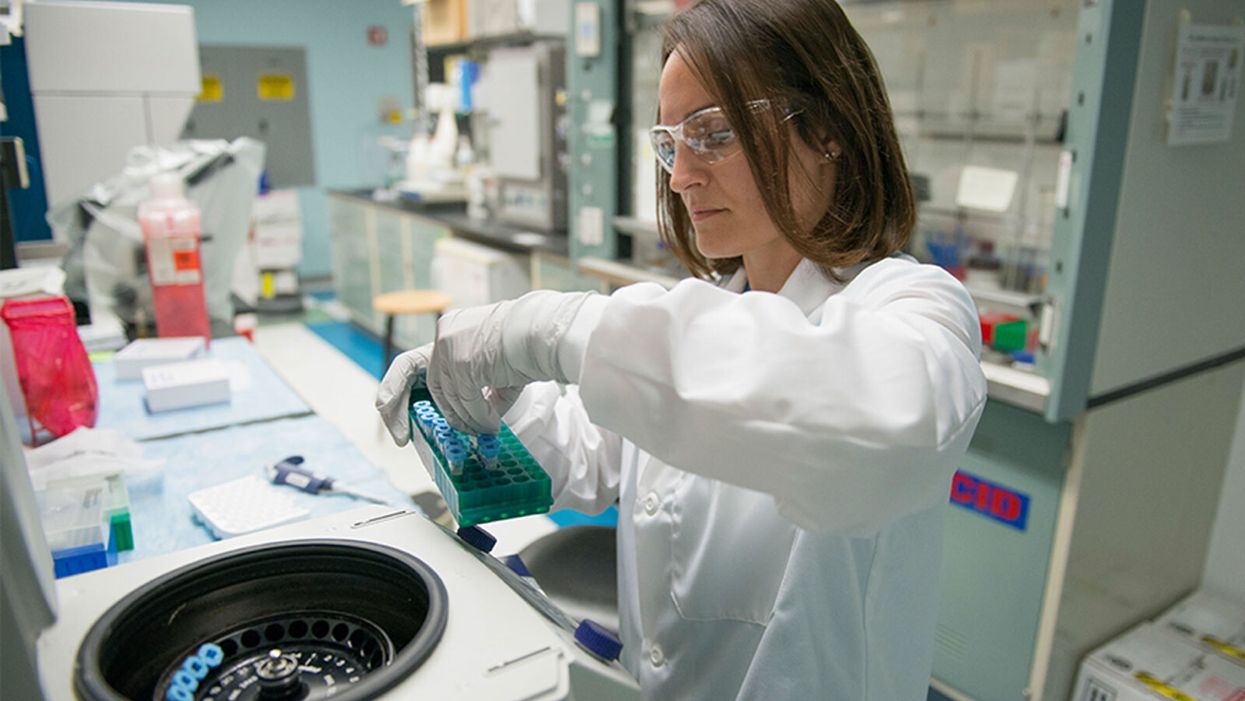
A researcher works in the lab at Alnylam Pharmaceuticals, which has pioneered the development of RNAi therapies.
In October 2006, Craig Mello received a strange phone call from Sweden at 4:30 a.m. The voice at the other end of the line told him to get dressed and that his life was about to change.
"We think this could be effective in [the early] phase, helping the body clear the virus and preventing progression to that severe hyperimmune response which occurs in some patients."
Shortly afterwards, he was informed that along with his colleague Andrew Fire, he had won the Nobel Prize in Physiology or Medicine.
Eight years earlier, biologists Fire and Mello had made a landmark discovery in the history of genetics. In a series of experiments conducted in worms, they had revealed an ancient evolutionary mechanism present in all animals that allows RNA – the structures within our cells that take genetic information from DNA and use it to make proteins – to selectively switch off genes.
At the time, scientists heralded the dawn of a new field of medical research utilizing this mechanism, known as RNA interference or RNAi, to tackle rare genetic diseases and deactivate viruses. Now, 14 years later, the pharmaceutical company Alnylam — which has pioneered the development of RNAi-based treatments over the past decade — is looking to use it to develop a groundbreaking drug for the virus that causes COVID-19.
"We can design small interfering RNAs to target regions of the viral genome and bind to them," said Akin Akinc, who manages several of Alnylam's drug development programs. "What we're learning about COVID-19 is that there's an early phase where there's lots of viral replication and a high viral load. We think this could be effective in that phase, helping the body clear the virus and preventing progression to that severe hyperimmune response which occurs in some patients."
Called ALN-COV, Alnylam's treatment hypothetically works by switching off a key gene in the virus, inhibiting its ability to replicate itself. In order to deliver it to the epithelial cells deep in the lung tissue, where the virus resides, patients will inhale a fine mist containing the RNAi molecules mixed in a saline solution, using a nebulizer.
But before human trials of the drug can begin, the company needs to convince regulators that it is both safe and effective in a series of preclinical trials. While early results appear promising - when mixed with the virus in a test tube, the drug displayed a 95 percent inhibition rate – experts are reserving judgment until it performs in clinical trials.
"If successful this could be a very important milestone in the development of RNAi therapies, but virus infections are very complicated and it can be hard to predict whether a given level of inhibition in cell culture will be sufficient to have a significant impact on the course of the infection," said Si-Ping Han, who researches RNAi therapeutics at California Institute of Technology and is not involved in the development of this drug.
So far, Alnylam has had success in using RNAi to treat rare genetic diseases. It currently has treatments licensed for Hereditary ATTR Amyloidosis and Acute Hepatic Porphyria. Another treatment, for Primary Hyperoxaluria Type 1, is currently under regulatory review. But its only previous attempt to use RNAi to tackle a respiratory infection was a failed effort to develop a drug for respiratory syncytial virus (RSV) almost a decade ago.
However, the technology has advanced considerably since then. "Back then, RNAi drugs had no chemical modifications whatsoever, so they were readily degraded by the body, and they could also result in unintended immune stimulation," said Akinc. "Since then, we've learned how to chemically modify our RNAi's to make them immunosilent and give them improved potency, stability, and duration of action."
"It would be a very important milestone in the development of RNAi therapies."
But one key challenge the company will face is the sheer speed at which viruses evolve, meaning they can become drug-resistant very quickly. Scientists predict that Alnylam will ultimately have to develop a series of RNAi drugs for the coronavirus that work together.
"There's been considerable interest in using RNAi to treat viral infections, as RNA therapies can be developed more rapidly than protein therapies like monoclonal antibodies, since one only needs to know the viral genome sequence to begin to design them," said David Schaffer, professor of bioengineering at University of California, Berkeley. "But viruses can evolve their sequences rapidly around single drugs so it is likely that a combinatorial RNAi therapy may be needed."
In the meantime, Alnylam is conducting further preclinical trials over the summer and fall, with the aim of launching testing in human volunteers by the end of this year -- an ambitious aim that would represent a breakneck pace for a drug development program.
If the approach does ultimately succeed, it would represent a major breakthrough for the field as a whole, potentially opening the door to a whole new wave of RNAi treatments for different lung infections and diseases.
"It would be a very important milestone in the development of RNAi therapies," said Han, the Caltech researcher. "It would be both the first time that an RNAi drug has been successfully used to treat a respiratory infection and as far as I know, the first time that one has been successful in treating any disease in the lungs. RNAi is a platform that can be reconfigured to hit different targets, and so once the first drug has been developed, we can expect a rapid flow of variants targeting other respiratory infections or other lung diseases."