Paralyzed By Polio, This British Tea Broker Changed the Course Of Medical History Forever
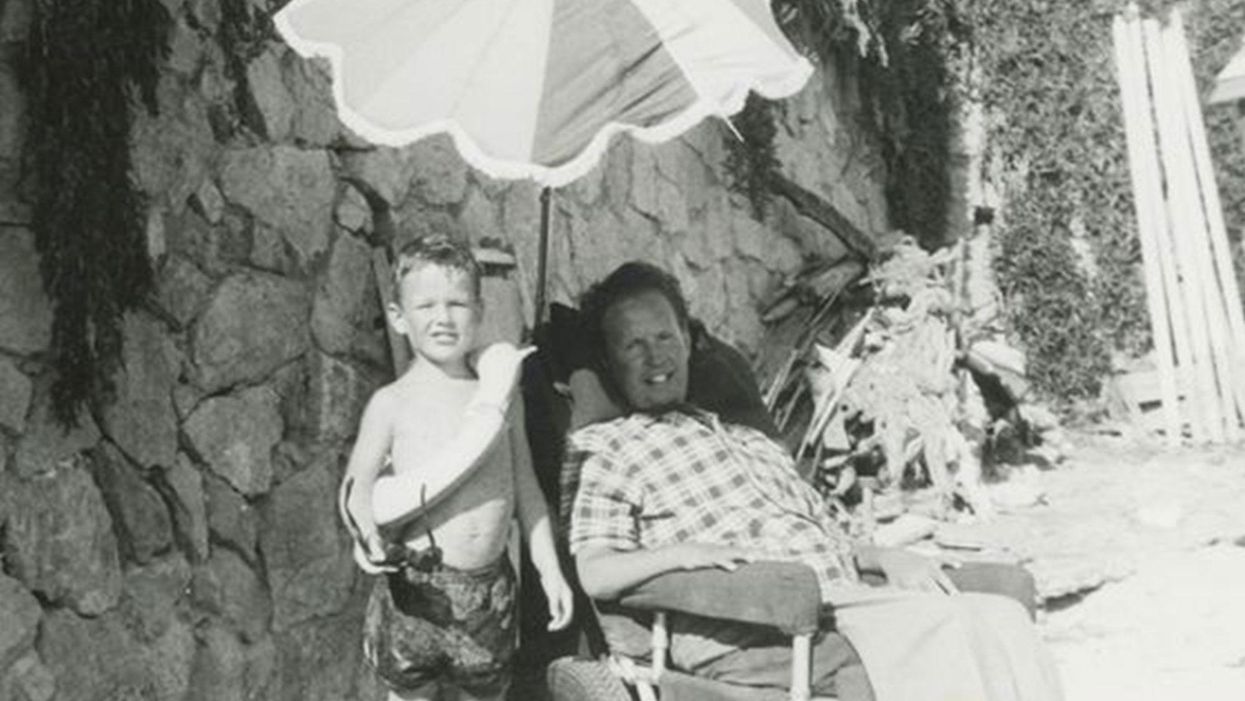
Robin Cavendish in his special wheelchair with his son Jonathan in the 1960s.
In December 1958, on a vacation with his wife in Kenya, a 28-year-old British tea broker named Robin Cavendish became suddenly ill. Neither he nor his wife Diana knew it at the time, but Robin's illness would change the course of medical history forever.
Robin was rushed to a nearby hospital in Kenya where the medical staff delivered the crushing news: Robin had contracted polio, and the paralysis creeping up his body was almost certainly permanent. The doctors placed Robin on a ventilator through a tracheotomy in his neck, as the paralysis from his polio infection had rendered him unable to breathe on his own – and going off the average life expectancy at the time, they gave him only three months to live. Robin and Diana (who was pregnant at the time with their first child, Jonathan) flew back to England so he could be admitted to a hospital. They mentally prepared to wait out Robin's final days.
But Robin did something unexpected when he returned to the UK – just one of many things that would astonish doctors over the next several years: He survived. Diana gave birth to Jonathan in February 1959 and continued to visit Robin regularly in the hospital with the baby. Despite doctors warning that he would soon succumb to his illness, Robin kept living.
After a year in the hospital, Diana suggested something radical: She wanted Robin to leave the hospital and live at home in South Oxfordshire for as long as he possibly could, with her as his nurse. At the time, this suggestion was unheard of. People like Robin who depended on machinery to keep them breathing had only ever lived inside hospital walls, as the prevailing belief was that the machinery needed to keep them alive was too complicated for laypeople to operate. But Diana and Robin were up for the challenges – and the risks. Because his ventilator ran on electricity, if the house were to unexpectedly lose power, Diana would either need to restore power quickly or hand-pump air into his lungs to keep him alive.
Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
In an interview as an adult, Jonathan Cavendish reflected on his parents' decision to live outside the hospital on a ventilator: "My father's mantra was quality of life," he explained. "He could have stayed in the hospital, but he didn't think that was as good of a life as he could manage. He would rather be two minutes away from death and living a full life."
After a few years of living at home, however, Robin became tired of being confined to his bed. He longed to sit outside, to visit friends, to travel – but had no way of doing so without his ventilator. So together with his friend Teddy Hall, a professor and engineer at Oxford University, the two collaborated in 1962 to create an entirely new invention: a battery-operated wheelchair prototype with a ventilator built in. With this, Robin could now venture outside the house – and soon the Cavendish family became famous for taking vacations. It was something that, by all accounts, had never been done before by someone who was ventilator-dependent. Robin and Hall also designed a van so that the wheelchair could be plugged in and powered during travel. Jonathan Cavendish later recalled a particular family vacation that nearly ended in disaster when the van broke down outside of Barcelona, Spain:
"My poor old uncle [plugged] my father's chair into the wrong socket," Cavendish later recalled, causing the electricity to short. "There was fire and smoke, and both the van and the chair ground to a halt." Johnathan, who was eight or nine at the time, his mother, and his uncle took turns hand-pumping Robin's ventilator by the roadside for the next thirty-six hours, waiting for Professor Hall to arrive in town and repair the van. Rather than being panicked, the Cavendishes managed to turn the vigil into a party. Townspeople came to greet them, bringing food and music, and a local priest even stopped by to give his blessing.
Robin had become a pioneer, showing the world that a person with severe disabilities could still have mobility, access, and a fuller quality of life than anyone had imagined. His mission, along with Hall's, then became gifting this independence to others like himself. Robin and Hall raised money – first from the Ernest Kleinwort Charitable Trust, and then from the British Department of Health – to fund more ventilator chairs, which were then manufactured by Hall's company, Littlemore Scientific Engineering, and given to fellow patients who wanted to live full lives at home. Robin and Hall used themselves as guinea pigs, testing out different models of the chairs and collaborating with scientists to create other devices for those with disabilities. One invention, called the Possum, allowed paraplegics to control things like the telephone and television set with just a nod of the head. Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
Robin went on to enjoy a long and happy life with his family at their house in South Oxfordshire, surrounded by friends who would later attest to his "down-to-earth" personality, his sense of humor, and his "irresistible" charm. When he died peacefully at his home in 1994 at age 64, he was considered the world's oldest-living person who used a ventilator outside the hospital – breaking yet another barrier for what medical science thought was possible.
This Special Music Helped Preemie Babies’ Brains Develop
Listening to music helped preterm babies' brains develop, according to the results of a new Swiss study.
Move over, Baby Einstein: New research from Switzerland shows that listening to soothing music in the first weeks of life helps encourage brain development in preterm babies.
For the study, the scientists recruited a harpist and a new-age musician to compose three pieces of music.
The Lowdown
Children who are born prematurely, between 24 and 32 weeks of pregnancy, are far more likely to survive today than they used to be—but because their brains are less developed at birth, they're still at high risk for learning difficulties and emotional disorders later in life.
Researchers in Geneva thought that the unfamiliar and stressful noises in neonatal intensive care units might be partially responsible. After all, a hospital ward filled with alarms, other infants crying, and adults bustling in and out is far more disruptive than the quiet in-utero environment the babies are used to. They decided to test whether listening to pleasant music could have a positive, counterbalancing effect on the babies' brain development.
Led by Dr. Petra Hüppi at the University of Geneva, the scientists recruited Swiss harpist and new-age musician Andreas Vollenweider (who has collaborated with the likes of Carly Simon, Bryan Adams, and Bobby McFerrin). Vollenweider developed three pieces of music specifically for the NICU babies, which were played for them five times per week. Each track was used for specific purposes: To help the baby wake up; to stimulate a baby who was already awake; and to help the baby fall back asleep.
When they reached an age equivalent to a full-term baby, the infants underwent an MRI. The researchers focused on connections within the salience network, which determines how relevant information is, and then processes and acts on it—crucial components of healthy social behavior and emotional regulation. The neural networks of preemies who had listened to Vollenweider's pieces were stronger than preterm babies who had not received the intervention, and were instead much more similar to full-term babies.
Next Up
The first infants in the study are now 6 years old—the age when cognitive problems usually become diagnosable. Researchers plan to follow up with more cognitive and socio-emotional assessments, to determine whether the effects of the music intervention have lasted.
The first infants in the study are now 6 years old—the age when cognitive problems usually become diagnosable.
The scientists note in their paper that, while they saw strong results in the babies' primary auditory cortex and thalamus connections—suggesting that they had developed an ability to recognize and respond to familiar music—there was less reaction in the regions responsible for socioemotional processing. They hypothesize that more time spent listening to music during a NICU stay could improve those connections as well; but another study would be needed to know for sure.
Open Questions
Because this initial study had a fairly small sample size (only 20 preterm infants underwent the musical intervention, with another 19 studied as a control group), and they all listened to the same music for the same amount of time, it's still undetermined whether variations in the type and frequency of music would make a difference. Are Vollenweider's harps, bells, and punji the runaway favorite, or would other styles of music help, too? (Would "Baby Shark" help … or hurt?) There's also a chance that other types of repetitive sounds, like parents speaking or singing to their children, might have similar effects.
But the biggest question is still the one that the scientists plan to tackle next: Whether the intervention lasts as the children grow up. If it does, that's great news for any family with a preemie — and for the baby-sized headphone industry.
Couples Facing Fertility Treatments Should Beware of This
Couples facing infertility should be savvy about the add-on procedures offered by some fertility clinics.
When Jane Stein and her husband used in-vitro fertilization in 2001 to become pregnant with twins, her fertility clinic recommended using a supplemental procedure called intracytoplasmic sperm injection (ICSI), known in fertility lingo as "ix-see."
'Add-on' fertility procedures are increasingly coming under scrutiny for having a high cost and low efficacy rate.
During IVF, an egg and sperm are placed in a petri dish together with the hope that a sperm will seek out and fertilize the egg. With ICSI, doctors inject sperm directly into the egg.
Stein, whose name has been changed to protect her privacy, agreed to try it. Her twins are now 16, but while 17 years have gone by since that procedure, the efficacy of ICSI is still unclear. In other words, while Stein succeeded in having children, it may not have been because of ICSI. It may simply have been because she did IVF.
The American Society for Reproductive Medicine has concluded, "There are no data to support the routine use of ICSI for non-male factor infertility." That is, ICSI can help couples have a baby when the issue is male infertility. But when it's not, the evidence of its effectiveness is lacking. And yet the procedure is being used more and more, even when male infertility is not the issue. Some 40 percent of fertility treatments in Europe, Asia and the Middle East now use ICSI, according to a world report released in 2016 by the International Committee for Monitoring Assisted Reproductive Technologies. In the Middle East, the figure is actually 100 percent, the report said.
ICSI is just one of many supplemental procedures, or 'add-ons,' increasingly coming under scrutiny for having a high cost and low efficacy rate. They cost anywhere from a couple of hundred dollars to several thousand – ICSI costs $2,000 to $3,000 -- hiking up the price of what is already a very costly endeavor. And many don't even work. Worse, some actually cause harm.
It's no surprise couples use them. They promise to increase the chance of conceiving. For patients who desperately want a child, money is no object. The Human Fertilization and Embryology Authority (HFEA) in the U.K. found that some 74 percent of patients who received fertility treatments over the last two years were given at least one type of add-on. Now, fertility associations in the U.S. and abroad have begun issuing guidance about which add-ons are worth the extra cost and which are not.
"Many IVF add-ons have little in the way of conclusive evidence supporting their role in successful IVF treatment," said Professor Geeta Nargund, medical director of CREATE Fertility and Lead Consultant for reproductive medicine at St George's Hospital, London.
The HFEA has actually rated these add-ons, indicating which procedures are effective and safe. Some treatments were rated 'red' because they were considered to have insufficient evidence to justify their use. These include assisted hatching, which uses acid or lasers to make a hole in the surrounding layer of proteins to help the embryo hatch; intrauterine culture, where a device is inserted into the womb to collect and incubate the embryo; and reproductive immunology, which suppresses the body's natural immunity so that it accepts the embryo.
"Fertility care is a highly competitive market. In a private system, offering add-ons may discern you from your neighboring clinic."
For some treatments, the HFEA found there is evidence that they don't just fail to work, but can even be harmful. These procedures include ICSI used when male infertility is not at issue, as well as a procedure called endometrial scratching, where the uterus is scratched, not unlike what would happen with a biopsy, to stimulate the local uterine immune system.
And then for some treatments, there is conflicting evidence, warranting further research. These include artificial egg activation by calcium ionophore, elective freezing in all cycles, embryo glue, time-lapse imaging and pre-implantation genetic testing for abnormal chromosomes on day 5.
"Currently, there is very little evidence to suggest that many of the add-ons could increase success rates," Nargund said. "Indeed, the HFEA's assessment of add-on treatments concluded that none of the add-ons could be given a 'green' rating, due to a lack of conclusive supporting research."
So why do fertility clinics offer them?
"Fertility care is a highly competitive market," said Professor Hans Evers, editor-in-chief of the journal Human Reproduction. "In a private system, offering add-ons may discern you from your neighboring clinic. The more competition, the more add-ons. Hopefully the more reputable institutions will only offer add-ons (for free) in the context of a randomized clinical trial."
The only way for infertile couples to know which work and which don't is the guidance released by professional organizations like the ASRM, and through government regulation in countries that have a public health care system.
The problem is, infertile couples will sometimes do anything to achieve a pregnancy.
"They will stand on their heads if this is advocated as helpful. Someone has to protect them," Evers said.
In the Netherlands, where Evers is based, the national health care system tries to make the best use of the limited resources it has, so it makes sure the procedures it's funding actually work, Evers said.
"We have calculated that to serve a population of 17 million, we need 13 IVF clinics, and we have 13," he said. "We as professionals discuss and try to agree on the value of newly proposed add-ons, and we will implement only those that are proven effective and safe."
Likewise, in the U.K., there's been a lot of squawking about speculative add-ons because the government, or National Health Service, pays for them. In the U.S., it's private insurers or patients' own cash.
"The [U.K.] government takes a very close look at what therapies they are offering and what the evidence is around offering the therapy," said Alan Penzias, who chairs the Practice Committee of the ASRM. It wants to make sure the treatments it is funding are at least worth the money.
ICSI is a case in point. Originally intended for male infertility, it's now being applied across the board because fertility clinics didn't want couples to pay $10,000 to $15,000 and wind up with no embryos.
"It is so disastrous to have no fertilization whatsoever, clinics started to make this bargain with their patients, saying, 'Well, listen, even though it's not indicated, what we would like to do is to take half of your eggs and do the ICSI procedure, and half we'll do conventional insemination just to make sure,'" he said. "It's a disaster if you have no embryos, and now you're out 10 to 12 thousand dollars, so for a small added fee, we can do the injection just to guard against that."
In the Netherlands, the national health care system tries to make the best use of its limited resources, so it makes sure the procedures it's funding actually work.
Clinics offer it where they see lower rates of fertilization, such as with older women or in cases where induced ovulation results in just two or three eggs instead of, say, 13. Unfortunately, ICSI may result in a higher fertilization rate, but it doesn't result in a higher live birth rate, according to a study last year in Human Reproduction, so couples wind up paying for a procedure that doesn't even result in a child.
Private insurers in the U.S. are keen to it. Penzia, who is also an associate professor of obstetrics, gynecology and reproductive biology at Harvard Medical School and works as a reproductive endocrinology and infertility specialist at Boston IVF, said Massachusetts requires that insurers cover infertility treatments. But when he submits claims for ICSI, for instance, insurers now want to see two sperm counts and proof that the man has seen a urologist.
"They want to make sure we're doing it for male factor (infertility)," he said. "That's not unreasonable, because the insurance company is taking the burden of this."

