Paralyzed By Polio, This British Tea Broker Changed the Course Of Medical History Forever
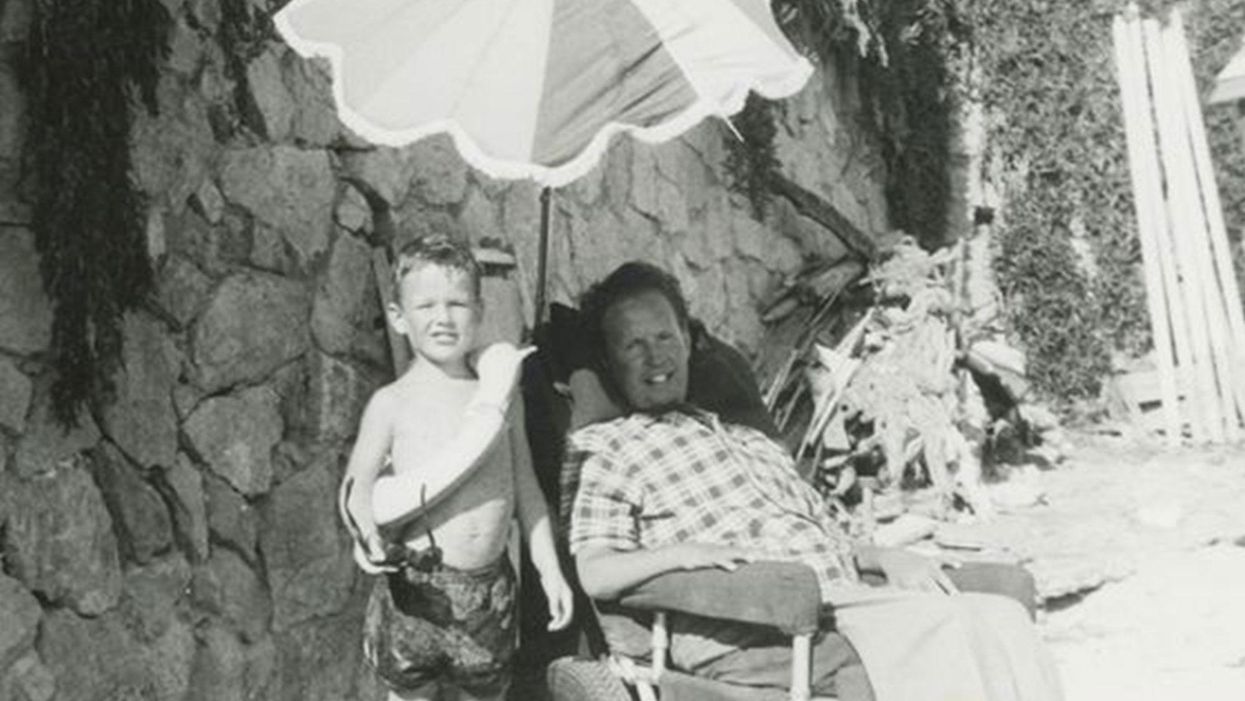
Robin Cavendish in his special wheelchair with his son Jonathan in the 1960s.
In December 1958, on a vacation with his wife in Kenya, a 28-year-old British tea broker named Robin Cavendish became suddenly ill. Neither he nor his wife Diana knew it at the time, but Robin's illness would change the course of medical history forever.
Robin was rushed to a nearby hospital in Kenya where the medical staff delivered the crushing news: Robin had contracted polio, and the paralysis creeping up his body was almost certainly permanent. The doctors placed Robin on a ventilator through a tracheotomy in his neck, as the paralysis from his polio infection had rendered him unable to breathe on his own – and going off the average life expectancy at the time, they gave him only three months to live. Robin and Diana (who was pregnant at the time with their first child, Jonathan) flew back to England so he could be admitted to a hospital. They mentally prepared to wait out Robin's final days.
But Robin did something unexpected when he returned to the UK – just one of many things that would astonish doctors over the next several years: He survived. Diana gave birth to Jonathan in February 1959 and continued to visit Robin regularly in the hospital with the baby. Despite doctors warning that he would soon succumb to his illness, Robin kept living.
After a year in the hospital, Diana suggested something radical: She wanted Robin to leave the hospital and live at home in South Oxfordshire for as long as he possibly could, with her as his nurse. At the time, this suggestion was unheard of. People like Robin who depended on machinery to keep them breathing had only ever lived inside hospital walls, as the prevailing belief was that the machinery needed to keep them alive was too complicated for laypeople to operate. But Diana and Robin were up for the challenges – and the risks. Because his ventilator ran on electricity, if the house were to unexpectedly lose power, Diana would either need to restore power quickly or hand-pump air into his lungs to keep him alive.
Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
In an interview as an adult, Jonathan Cavendish reflected on his parents' decision to live outside the hospital on a ventilator: "My father's mantra was quality of life," he explained. "He could have stayed in the hospital, but he didn't think that was as good of a life as he could manage. He would rather be two minutes away from death and living a full life."
After a few years of living at home, however, Robin became tired of being confined to his bed. He longed to sit outside, to visit friends, to travel – but had no way of doing so without his ventilator. So together with his friend Teddy Hall, a professor and engineer at Oxford University, the two collaborated in 1962 to create an entirely new invention: a battery-operated wheelchair prototype with a ventilator built in. With this, Robin could now venture outside the house – and soon the Cavendish family became famous for taking vacations. It was something that, by all accounts, had never been done before by someone who was ventilator-dependent. Robin and Hall also designed a van so that the wheelchair could be plugged in and powered during travel. Jonathan Cavendish later recalled a particular family vacation that nearly ended in disaster when the van broke down outside of Barcelona, Spain:
"My poor old uncle [plugged] my father's chair into the wrong socket," Cavendish later recalled, causing the electricity to short. "There was fire and smoke, and both the van and the chair ground to a halt." Johnathan, who was eight or nine at the time, his mother, and his uncle took turns hand-pumping Robin's ventilator by the roadside for the next thirty-six hours, waiting for Professor Hall to arrive in town and repair the van. Rather than being panicked, the Cavendishes managed to turn the vigil into a party. Townspeople came to greet them, bringing food and music, and a local priest even stopped by to give his blessing.
Robin had become a pioneer, showing the world that a person with severe disabilities could still have mobility, access, and a fuller quality of life than anyone had imagined. His mission, along with Hall's, then became gifting this independence to others like himself. Robin and Hall raised money – first from the Ernest Kleinwort Charitable Trust, and then from the British Department of Health – to fund more ventilator chairs, which were then manufactured by Hall's company, Littlemore Scientific Engineering, and given to fellow patients who wanted to live full lives at home. Robin and Hall used themselves as guinea pigs, testing out different models of the chairs and collaborating with scientists to create other devices for those with disabilities. One invention, called the Possum, allowed paraplegics to control things like the telephone and television set with just a nod of the head. Robin's wheelchair was not only the first of its kind; it became the model for the respiratory wheelchairs that people still use today.
Robin went on to enjoy a long and happy life with his family at their house in South Oxfordshire, surrounded by friends who would later attest to his "down-to-earth" personality, his sense of humor, and his "irresistible" charm. When he died peacefully at his home in 1994 at age 64, he was considered the world's oldest-living person who used a ventilator outside the hospital – breaking yet another barrier for what medical science thought was possible.
Shoot for the Moon: Its Surface Contains a Pot of Gold
An astronaut standing on the Moon.
Here's a riddle: What do the Moon, nuclear weapons, clean energy of the future, terrorism, and lung disease all have in common?
One goal of India's upcoming space probe is to locate deposits of helium-3 that are worth trillions of dollars.
The answer is helium-3, a gas that's extremely rare on Earth but 100 million times more abundant on the Moon. This past October, the Lockheed Martin corporation announced a concept for a lunar landing craft that may return humans to the Moon in the coming decade, and yesterday China successfully landed the Change-4 probe on the far side of the Moon. Landing inside the Moon's deepest crater, the Chinese achieved a first in space exploration history.
Meanwhile, later this month, India's Chandrayaan-2 space probe will also land on the lunar surface. One of its goals is to locate deposits of helium-3 that are worth trillions of dollars, because it could be a fuel for nuclear fusion energy to generate electricity or propel a rocket.
The standard way that nuclear engineers are trying to achieve sustainable fusion uses fuels that are more plentiful on Earth: deuterium and tritium. But MIT researchers have found that adding small amounts of helium-3 to the mix could make it much more efficient, and thus a viable energy source much sooner that once thought.
Even if fusion is proven practical tomorrow, any kind of nuclear energy involves long waits for power plant construction measured in decades. However, mining helium-3 could be useful now, because of its non-energy applications. A major one is its ability to detect neutrons coming from plutonium that could be used in terrorist attacks. Here's how it works: a small amount of helium-3 is contained within a forensic instrument. When a neutron hits an atom of helium-3, the reaction produces tritium, a proton, and an electrical charge, alerting investigators to the possibility that plutonium is nearby.
Ironically, as global concern about a potential for hidden nuclear material increased in the early 2000s, so did the supply of helium-3 on Earth. That's because helium-3 comes from the decay of tritium, used in thermonuclear warheads (H-bombs). Thousands of such weapons have been dismantled from U.S. and Russian arsenals, making helium-3 available for plutonium detection, research, and other applications--including in the world of healthcare.
Helium-3 can help doctors diagnose lung diseases, since it enables imaging of the lungs in real time.
Helium-3 dramatically improves the ability of doctors to image the lungs in a range of diseases including asthma, chronic obstructive pulmonary disease and emphysema, cystic fibrosis, and bronchopulmonary dysplasia, which happens particularly in premature infants. Specifically, helium-3 is useful in magnetic resonance imaging (MRI), a procedure that creates images from within the body for diagnostic purposes.
But while a standard MRI allows doctors to visualize parts of the body like the heart or brain, it's useless for seeing the lungs. Because lungs are filled with air, which is much less dense than water or fat, effectively no signals are produced that would enable imaging.
To compensate for this problem, a patient can inhale gas that is hyperpolarized –meaning enhanced with special procedures so that the magnetic resonance signals from the lungs are finally readable. This gas is safe to breathe when mixed with enough oxygen to support life. Helium-3 is one such gas that can be hyperpolarized; since it produces such a strong signal, the MRI can literally see the air inside the lungs and in all of the airways, revealing intricate details of the bronchopulmonary tree. And it can do this in real time
The capability to show anatomic details of the lungs and airways, and the ability to display functional imaging as a patient breathes, makes helium-3 MRI far better than the standard method of testing lung function. Called spirometry, this method tells physicians how the lungs function overall, but does not home in on particular areas that may be causing a problem. Plus, spirometry requires patients to follow instructions and hold their breath, so it is not great for testing young children with pulmonary disease.
In recent years, the cost of helium-3 on Earth has skyrocketed.
Over the past several years, researchers have been developing MRI for lung testing using other hyperpolarized gases. The main alternative to helium-3 is xenon-129. Over the years, researchers have learned to overcome certain disadvantages of the latter, such as its potential to put patients to sleep. Since helium-3 provides the strongest signal, though, it is still the best gas for MRI studies in many lung conditions.
But the supply of helium-3 on Earth has been decreasing in recent years, due to the declining rate of dismantling of warheads, just as the Department of Homeland Security has required more and more of the gas for neutron detection. As a result, the cost of the gas has skyrocketed. Less is available now for medical uses – unless, of course, we begin mining it on the moon.
The question is: Are the benefits worth the 239,000-mile trip?
Should Organ Donors Be Paid?
A depiction of selling a human heart for cash.
Deanna Santana had assumed that people on organ transplant lists received matches. She didn't know some died while waiting. But in May 2011, after her 17-year-old son, Scott, was killed in a car accident, she learned what a precious gift organ and tissue donation can be.
"I would estimate it cost our family about $4,000 for me to donate a kidney to a stranger."
His heart, lungs, kidneys, liver and pancreas saved five people. His corneas enabled two others to see. And his bones, connective tissues and veins helped 73 individuals.
The donation's impact had a profound effect on his mother as well. In September 2016, she agreed to donate a kidney in a paired exchange of four people making the same sacrifice for four compatible strangers.
She gave up two weeks' worth of paid vacation to recuperate and covered lodging costs for loved ones during her transplant. Eventually, she qualified for state disability for part of her leave, but the compensation was less than her salary as public education and relations manager at Sierra Donor Services, an organ procurement organization in West Sacramento, California.
"I would estimate it cost our family about $4,000 for me to donate a kidney to a stranger," says Santana, 51. Despite the monetary hardship, she "would do it again in a heartbeat."
While some contend it's exploitative to entice organ donors and their families with compensation, others maintain they should be rewarded for extending their generosity while risking complications and recovering from donation surgery. But many agree on one point: The focus should be less on paying donors and more on removing financial barriers that may discourage interested prospects from doing a good deed.
"There's significant potential risk associated with donating a kidney, some of which we're continuing to learn," says transplant surgeon Matthew Cooper, a board member of the National Kidney Foundation and co-chair of its Transplant Task Force.
Although most kidneys are removed laparoscopically, reducing hospitalization and recuperation time, complications can occur. The risks include wound and urinary tract infections, pneumonia, blood clots, injury to local nerves causing decreased sensation in the hip or thigh, acute blood loss requiring transfusion and even death, Cooper says.
"We think that donation is a cost-neutral opportunity. It, in fact, is not."
Meanwhile, from a financial standpoint, estimates have found it costs a kidney donor in the United States an average of $3,000 to navigate the entire transplant process, which may include time off from work, travel to and from the hospital, accommodations, food and child care expenses.
"We think that donation is a cost-neutral opportunity. It, in fact, is not," says Cooper, who is also Director of Kidney and Pancreas Transplantation at MedStar Georgetown Transplant Institute in Washington, D.C.
The National Organ Transplant Act of 1984 makes it illegal to sell human organs but did not prohibit payment for the donation of human plasma, sperm and egg cells.
Unlike plasma, sperm and eggs cells—which are "renewable resources"—a kidney is irreplaceable, says John J. Friedewald, a nephrologist who is medical director of kidney transplantation at Northwestern Memorial Hospital in Chicago.
Offering some sort of incentives could lessen the overall burden on donors while benefiting many more potential recipients. "We can eliminate the people waiting on the list and dying, at least for kidneys," Friedewald says.
On the other hand, incentives may influence an individual to the point that the donation is made purely for monetary gain. "It's a delicate balance," he explains, "because so much of the transplant system has been built on altruism."
That's where doing away with the "disincentives" comes into the equation. Compensating donors for the costs they endure would be a reasonable compromise, Friedewald says.
Depending on the state, living donors may deduct up to $10,000 from their adjusted gross income under the Organ Donation Tax Deduction Act for the year in which the transplantation occurs. "Human organ" applies to all or part of a liver, pancreas, kidney, intestine, lung or bone marrow. The subtracted modification may be claimed for only unreimbursed travel and lodging expenses and lost wages.
For some or many donors, the tax credit doesn't go far enough in offsetting their losses, but they often take it in stride, says Chaya Lipschutz, a Brooklyn, N.Y.-based matchmaker for donors and recipients, who launched the website KidneyMitzvah.com in 2009.
Seeking compensation for lost wages "is extremely rare" in her experience. "In all the years of doing this," she recalls, "I only had two people who donated a kidney who needed to get paid for lost wages." She finds it "pretty amazing that mostly all who contact don't ask."
Lipschutz, an Orthodox Jew, has walked in a donor's shoes. In September 2005, at age 48, she donated a kidney to a stranger after coming across an ad in a weekly Jewish newspaper. The ad stated: "Please help save a Jewish life—New Jersey mother of two in dire need of kidney—Whoever saves one life from Israel it is as if they saved an entire nation."
To make matches, Lipschutz posts in various online groups in the United States and Israel. Donors in Israel may receive "refunds" for loss of earnings, travel expenses, psychological treatment, recovery leave, and insurance. They also qualify for visits to national parks and nature reserves without entrance fees, Lipschutz says.
"There has been an attempt to figure out what would constitute fair compensation without the appearance that people are selling their organs or their loved ones' organs."
Kidneys can be procured from healthy living donors or patients who have undergone circulatory or brain death.
"The real dilemma arises with payment for living donation, which would favor poorer individuals to donate who would not necessarily do so," says Dr. Cheryl L. Kunis, a New York-based nephrologist whose practice consists primarily of kidney transplant recipients. "In addition, such payment for living donation has not demonstrated to improve a donor's socioeconomic status globally."
Living kidney donation has the highest success rate. But organs from young and previously healthy individuals who die in accidents or from overdoses, especially in the opioid epidemic, often work just as well as kidneys from cadaveric donors who succumb to trauma, Kunis says.
In these tragic circumstances, she notes that the decision to donate is often left to an individual's grieving family members when a living will isn't available. A payment toward funeral expenses, for instance, could tip their decision in favor of organ donation.
A similar scenario presents when a patient with a beating heart is on the verge of dying, and the family is unsure about consenting to organ donation, says Jonathan D. Moreno, a professor in the department of medical ethics and health policy at the University of Pennsylvania.
"There has been an attempt to figure out what would constitute fair compensation," he says, "without the appearance that people are selling their organs or their loved ones' organs."
The overarching concern remains the same: Compensating organ donors could lead to exploitation of socioeconomically disadvantaged groups. "What's likely to finally resolve" this bioethics debate, Moreno foresees, "is patient-compatible organs grown in pigs as the basic science of xenotransplants (between species) seems to be progressing."
Cooper, the transplant surgeon at Georgetown, believes more potential donors would come forward if financial barriers weren't an issue. Of the ones who end up giving a part of themselves, with or without reimbursement, "the overwhelming majority look back upon it as an extremely positive experience," he says. After all, "they're lifesavers. They should be celebrated."

