Why Are Scientists and Patients Visiting This Island Paradise?
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.

An inviting beach in Nassau, Bahamas.
Dr. Conville Brown, a cardiologist-researcher in The Bahamas, is at the helm of a fascinating worldwide project: He's leading a movement to help accelerate innovation by providing scientists and patients from around the globe with a legal, cost-effective, and ethically rigorous place to conduct medical research, as well as to offer commercial therapies that are already approved in some jurisdictions, but not others. He recently spoke with Editor-In-Chief Kira Peikoff about The Bahamas' emerging ascendance in the scientific world. This interview has been edited and condensed for brevity.
"You don't want to take shortcuts from the perspective of not giving proper due diligence to the process, but you also don't want it to be overwhelmed with red tape."
Tell me about the work you do in the Bahamas – what is the research focus?
We have a couple research opportunities here. Several years ago, we established the Partners Clinical Research Centre, the idea being that we can partner with different people in different territories in the world, including the United States, and be able to perform ethical research as would be defined and adjudicated by an institutional review board and a properly constituted ethics committee. We do all of this with FDA rigor, but in a non-FDA jurisdiction.
By doing this, we want to look for the science behind the research, and want to know that there is a sound clinical hypothesis that's going to be tested. We also want to know that the safety of the human subjects is assured as much as possible, and of course, assess the efficacy of that which you're testing. We want to do this in the same manner as the FDA, except in a more accelerated and probably less bureaucratic manner. You don't want to take shortcuts from the perspective of not giving proper due diligence to the process, but you also don't want it to be overwhelmed with red tape, so that what could be 3 months takes 3 years. A jet ski turns around a lot faster than the Queen Mary.
Why do you think the clinical research process in other countries like the U.S. has become burdened with red tape?
The litigious nature of society is a contributing factor. If people are negligent, they deserve to be sued. Unfortunately, all too often, some things get taken too far, and sometimes, the pendulum swings too far in the wrong direction and then it's counterproductive, so the whole process then becomes so very heavily regulated and financially burdensome. A lot of American companies have gone outside the country to get their clinical trials and/or device testing done because it's too phenomenally expensive and time-consuming. We seek to make sure the same degree of diligence is exercised but in a lesser time frame, and of course, at a much lower cost.
The other aspect, of course, is that there are certain opportunities where we have major jurisdictions, as in Europe, that have determined that a therapy or device is safe. Those services and devices we can utilize in the Bahamas--not as a clinical research tool, but as a therapy, which of course, the United States is not able to do without FDA approval. That could easily take another five years. So there is an opportunity for us in that window to make available such therapies and devices to the North American community. I like to call this "Advanced Medical Tourism" or "Advanced TransNational Medical Care." Instead of somebody flying nine hours to Europe, they can also now fly to the Bahamas, as little as half an hour away, and as long as we are satisfied that the science is sound and the approvals are in place from a senior jurisdiction, then we can legally serve any patient that is eligible for that particular therapy.

Dr. Conville Brown
(Courtesy)
Are you seeing an influx of patients for that kind of medical tourism?
The numbers are increasing. The stem cell legislation has now been in place for two to three years, so we have a number of entities including some large international companies coming to the shores of the Bahamas to provide some therapies here, and others for research. The vast majority of our clientele are from abroad, particularly the U.S. We fully plan to increase the traffic flow to the Bahamas for medical tourism, or preferably, TransNational Medical Care, Advanced and Conventional.
How do patients find out about available therapies and trials happening there?
Advertising in the international arena for something that is perfectly legal within the confines of Bahamas is par for the course. But the marketing efforts have not been that heavy while all the processes and procedures are being fine-tuned and the various entities are set up to handle more than 100 people at a time.
"We were able to accelerate those programs, and do it a lot less expensively than can be done in continental countries, but just as well."
What kind of research is being done by companies who have come to the Bahamas?
We've been involved in first-in-man procedures for neuromodulation of the cardiovascular system, where we inserted a device into the blood vessels and stimulated the autonomic nervous system with a view to controlling patients' blood pressure and heart rate in conditions such as congestive heart failure. We have also looked at injectable glucose sensors, to continually monitor the blood glucose, and via a chip, can send the blood glucose measurement back to the patient's cell phone. So the patient looks at his phone for his blood sugar. That was phenomenally exciting, the clinical trial was very positive, and the company is now developing a final prototype to commercialize the product. We were able to accelerate those programs, and do it a lot less expensively than can be done in continental countries, but just as well. The Bahamas has also crafted legislation specifically for regenerative medicine and stem cell research, so that becomes an additional major attraction.
Do you ever find that there is skepticism around going to the Caribbean to do science?
When it comes to clinical research and new medical devices, one might be skeptical about the level of medical/scientific expertise that is resident here. We're here to show that we do in fact have that expertise resident within The Partners Clinical Research Centre, within The Partners Stem Cell Centre, and we have formed our partnerships accordingly so that when prudent and necessary, we bring in additional expertise from the very territories that are seeking to accelerate.
Have you seen a trend toward increasing interest from researchers around the world?
Absolutely. One company, for example, is interested not only in the clinical side, but also the preclinical side--where you can have animal lab experiments done in the Bahamas, and being able to bridge that more readily with the clinical side. That presents a major opportunity for parties involved because again, the financial savings are exponential without compromising standards.
"A person who is 75 and frail, he doesn't want to wait to see if he will make it to 80 to benefit from the agent if it's approved in five years. Instead he can come to our center."
Where are some of these researchers from?
The United States, the Czech Republic, Russia, Canada, and South America. I expect significantly more interest once we promote the idea of European products having a welcome niche in the Bahamas, because we accept federal approvals from the U.S., Canada, and the European Union.
What do you think will be the first medical breakthrough to come out of research there?
One of the biggest killers in the world is heart disease, and we have the opportunity to implement a number of cardiac protocols utilizing stem cell therapy, particularly for those with no options. We just completed a state-of-the art medical center that we fashioned after the University of Miami that is getting ready for prime time. The sky will be the limit for the cardiac patient with respect to stem cell medicine.
Second, we are extremely pleased to be involved with a company called Longeveron, which is looking at how one might age better, and age more slowly, particularly with the administration of young blood and mesenchymal stem cells to frail, elderly candidates. Healthy young men have their mesenchymal stem cells harvested, expanded, and then administered to frail, elderly individuals with a view to improving their Frailty Index and functionality (feeling younger). There is a lot of interest in this arena, as one could imagine.
And herein lies the classical scenario for the Bahamas: Longeveron is now recruiting patients for its phase IIB double blind, placebo-controlled clinical trial at multiple sites across the U.S., which will add some two to three years to its data collection. Originally this work was done with NIH support at the University of Miami's Interdisciplinary Stem Cell Institute by Dr. Joshua Hare, and published in the Journal of Gerontology. So now, during the ongoing and expanded clinical trial, with those positive signals, we are able to have a commercially available clinical registry in the Bahamas. This has been approved by the ethics committee here, which is comprised of international luminaries in regenerative medicine. Longeveron will also be conducting an additional randomized clinical trial arm of same at our Centre in The Bahamas, The Partners Stem Cell Centre.
Can you clarify what you mean by "registry"?
In other words, you still have to fit the eligibility criteria to receive the active agent, but the difference is that in a placebo-controlled double-blind clinical trial, the physician/researcher and the patient don't know if they are getting the active agent or placebo. In the registry, there is no placebo, and you know you're getting the active agent, what we call "open label." You're participating because of the previous information on efficacy and safety.
A person who is 75 and frail, he doesn't want to wait to see if he will make it to 80 to benefit from the agent if it's approved in five years. Instead he can come to our center, one of the designated centers, and as long as he meets the inclusion criteria, may participate in said registry. The additional data from our patients can bolster the numbers in the clinical trial, which can contribute to the FDA approval process. One can see how this could accelerate the process of discovery and acceptance, as well as prove if the agent was not as good as it was made out to be. It goes both ways.
"We would love to be known as a place that facilitates the acceleration of ethical science and ethical therapies, and therefore brings global relief to those in need."
Do you think one day the Bahamas will be more well-known for its science than its beaches?
I doubt that. What I would like to say is that the Bahamas would love to always be known for its beautiful beaches, but we would also like to be known for diversity and innovation. Apart from all that beauty, we can still play a welcoming role to the rest of the scientific world. We would love to be known as a place that facilitates the acceleration of ethical science and ethical therapies, and therefore brings global relief to those in need.
Kira Peikoff was the editor-in-chief of Leaps.org from 2017 to 2021. As a journalist, her work has appeared in The New York Times, Newsweek, Nautilus, Popular Mechanics, The New York Academy of Sciences, and other outlets. She is also the author of four suspense novels that explore controversial issues arising from scientific innovation: Living Proof, No Time to Die, Die Again Tomorrow, and Mother Knows Best. Peikoff holds a B.A. in Journalism from New York University and an M.S. in Bioethics from Columbia University. She lives in New Jersey with her husband and two young sons. Follow her on Twitter @KiraPeikoff.
Dr. May Edward Chinn, Kizzmekia Corbett, PhD., and Alice Ball, among others, have been behind some of the most important scientific work of the last century.
If you look back on the last century of scientific achievements, you might notice that most of the scientists we celebrate are overwhelmingly white, while scientists of color take a backseat. Since the Nobel Prize was introduced in 1901, for example, no black scientists have landed this prestigious award.
The work of black women scientists has gone unrecognized in particular. Their work uncredited and often stolen, black women have nevertheless contributed to some of the most important advancements of the last 100 years, from the polio vaccine to GPS.
Here are five black women who have changed science forever.
Dr. May Edward Chinn
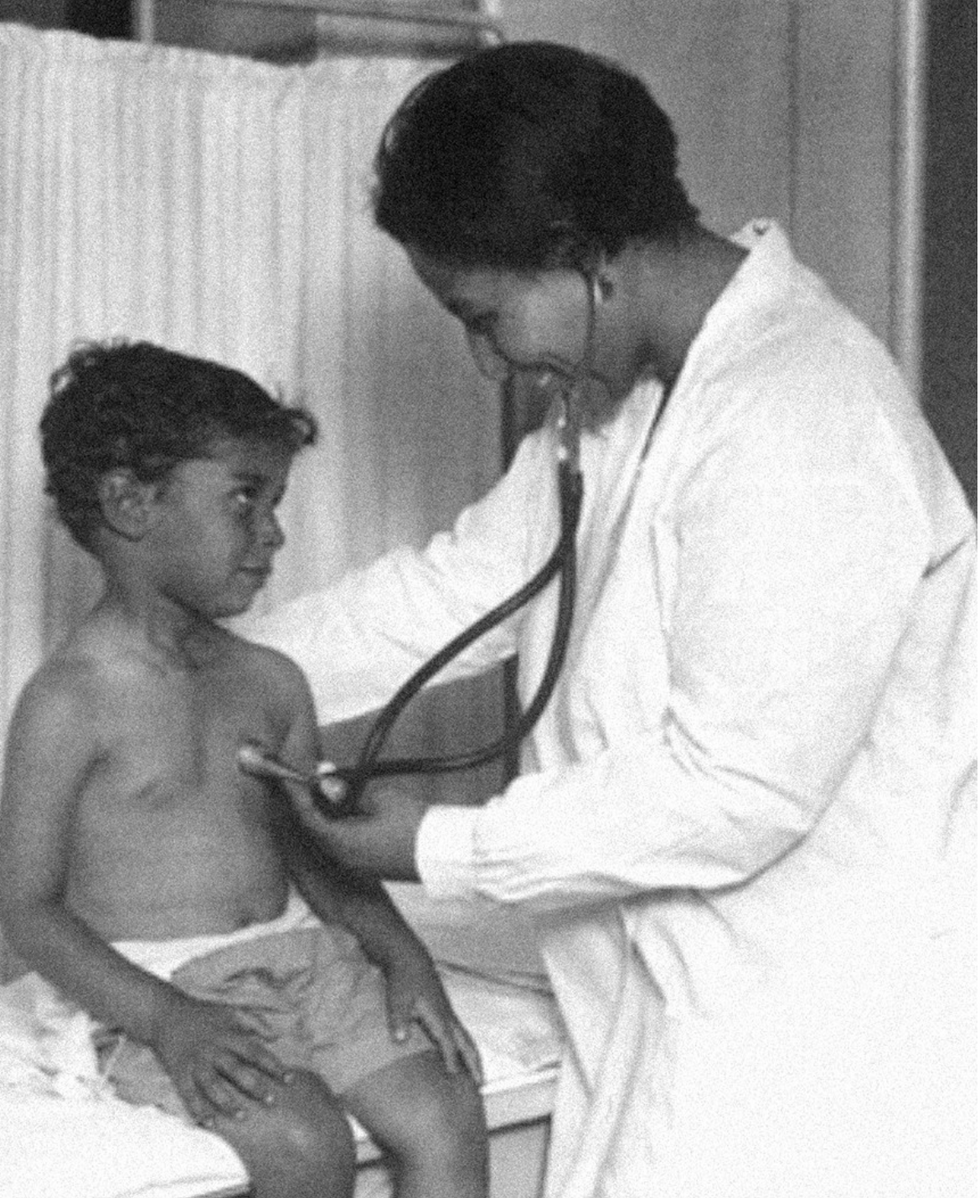
Dr. May Edward Chinn practicing medicine in Harlem
George B. Davis, PhD.
Chinn was born to poor parents in New York City just before the start of the 20th century. Although she showed great promise as a pianist, playing with the legendary musician Paul Robeson throughout the 1920s, she decided to study medicine instead. Chinn, like other black doctors of the time, were barred from studying or practicing in New York hospitals. So Chinn formed a private practice and made house calls, sometimes operating in patients’ living rooms, using an ironing board as a makeshift operating table.
Chinn worked among the city’s poor, and in doing this, started to notice her patients had late-stage cancers that often had gone undetected or untreated for years. To learn more about cancer and its prevention, Chinn begged information off white doctors who were willing to share with her, and even accompanied her patients to other clinic appointments in the city, claiming to be the family physician. Chinn took this information and integrated it into her own practice, creating guidelines for early cancer detection that were revolutionary at the time—for instance, checking patient health histories, checking family histories, performing routine pap smears, and screening patients for cancer even before they showed symptoms. For years, Chinn was the only black female doctor working in Harlem, and she continued to work closely with the poor and advocate for early cancer screenings until she retired at age 81.
Alice Ball

Pictorial Press Ltd/Alamy
Alice Ball was a chemist best known for her groundbreaking work on the development of the “Ball Method,” the first successful treatment for those suffering from leprosy during the early 20th century.
In 1916, while she was an undergraduate student at the University of Hawaii, Ball studied the effects of Chaulmoogra oil in treating leprosy. This oil was a well-established therapy in Asian countries, but it had such a foul taste and led to such unpleasant side effects that many patients refused to take it.
So Ball developed a method to isolate and extract the active compounds from Chaulmoogra oil to create an injectable medicine. This marked a significant breakthrough in leprosy treatment and became the standard of care for several decades afterward.
Unfortunately, Ball died before she could publish her results, and credit for this discovery was given to another scientist. One of her colleagues, however, was able to properly credit her in a publication in 1922.
Henrietta Lacks

onathan Newton/The Washington Post/Getty
The person who arguably contributed the most to scientific research in the last century, surprisingly, wasn’t even a scientist. Henrietta Lacks was a tobacco farmer and mother of five children who lived in Maryland during the 1940s. In 1951, Lacks visited Johns Hopkins Hospital where doctors found a cancerous tumor on her cervix. Before treating the tumor, the doctor who examined Lacks clipped two small samples of tissue from Lacks’ cervix without her knowledge or consent—something unthinkable today thanks to informed consent practices, but commonplace back then.
As Lacks underwent treatment for her cancer, her tissue samples made their way to the desk of George Otto Gey, a cancer researcher at Johns Hopkins. He noticed that unlike the other cell cultures that came into his lab, Lacks’ cells grew and multiplied instead of dying out. Lacks’ cells were “immortal,” meaning that because of a genetic defect, they were able to reproduce indefinitely as long as certain conditions were kept stable inside the lab.
Gey started shipping Lacks’ cells to other researchers across the globe, and scientists were thrilled to have an unlimited amount of sturdy human cells with which to experiment. Long after Lacks died of cervical cancer in 1951, her cells continued to multiply and scientists continued to use them to develop cancer treatments, to learn more about HIV/AIDS, to pioneer fertility treatments like in vitro fertilization, and to develop the polio vaccine. To this day, Lacks’ cells have saved an estimated 10 million lives, and her family is beginning to get the compensation and recognition that Henrietta deserved.
Dr. Gladys West

Andre West
Gladys West was a mathematician who helped invent something nearly everyone uses today. West started her career in the 1950s at the Naval Surface Warfare Center Dahlgren Division in Virginia, and took data from satellites to create a mathematical model of the Earth’s shape and gravitational field. This important work would lay the groundwork for the technology that would later become the Global Positioning System, or GPS. West’s work was not widely recognized until she was honored by the US Air Force in 2018.
Dr. Kizzmekia "Kizzy" Corbett

TIME Magazine
At just 35 years old, immunologist Kizzmekia “Kizzy” Corbett has already made history. A viral immunologist by training, Corbett studied coronaviruses at the National Institutes of Health (NIH) and researched possible vaccines for coronaviruses such as SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome).
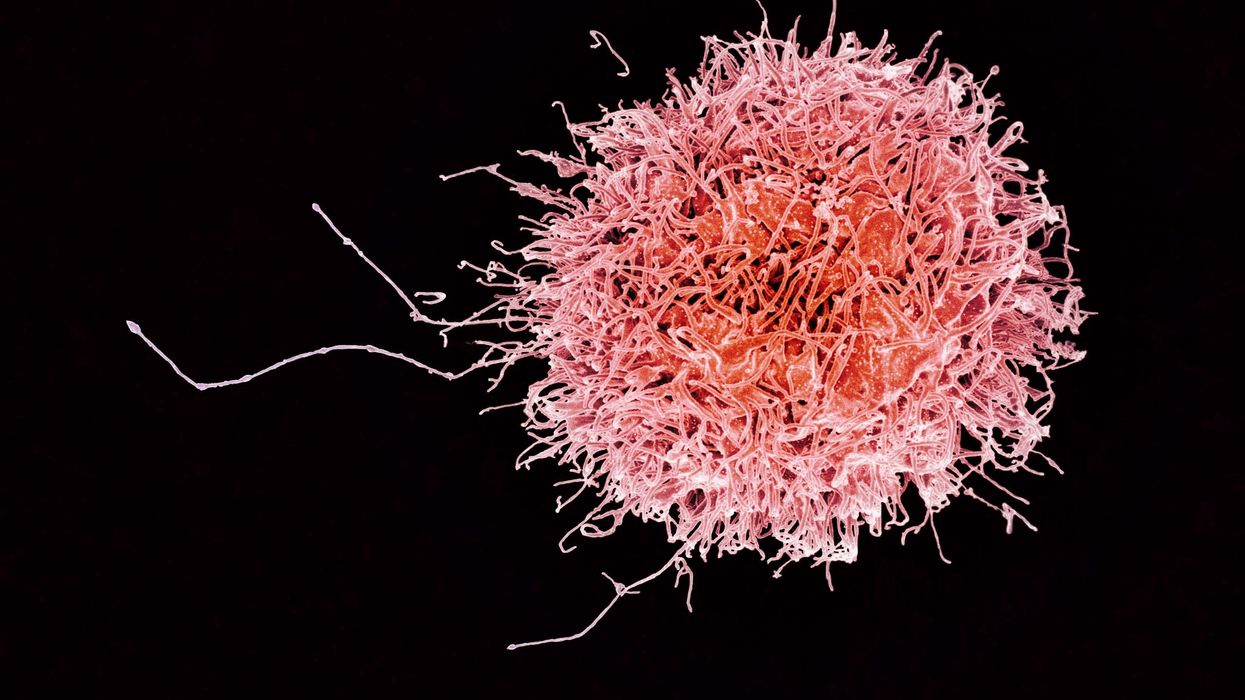
At the start of the COVID pandemic, Corbett and her team at the NIH partnered with pharmaceutical giant Moderna to develop an mRNA-based vaccine against the virus. Corbett’s previous work with mRNA and coronaviruses was vital in developing the vaccine, which became one of the first to be authorized for emergency use in the United States. The vaccine, along with others, is responsible for saving an estimated 14 million lives.On today’s episode of Making Sense of Science, I’m honored to be joined by Dr. Paul Song, a physician, oncologist, progressive activist and biotech chief medical officer. Through his company, NKGen Biotech, Dr. Song is leveraging the power of patients’ own immune systems by supercharging the body’s natural killer cells to make new treatments for Alzheimer’s and cancer.
Whereas other treatments for Alzheimer’s focus directly on reducing the build-up of proteins in the brain such as amyloid and tau in patients will mild cognitive impairment, NKGen is seeking to help patients that much of the rest of the medical community has written off as hopeless cases, those with late stage Alzheimer’s. And in small studies, NKGen has shown remarkable results, even improvement in the symptoms of people with these very progressed forms of Alzheimer’s, above and beyond slowing down the disease.
In the realm of cancer, Dr. Song is similarly setting his sights on another group of patients for whom treatment options are few and far between: people with solid tumors. Whereas some gradual progress has been made in treating blood cancers such as certain leukemias in past few decades, solid tumors have been even more of a challenge. But Dr. Song’s approach of using natural killer cells to treat solid tumors is promising. You may have heard of CAR-T, which uses genetic engineering to introduce cells into the body that have a particular function to help treat a disease. NKGen focuses on other means to enhance the 40 plus receptors of natural killer cells, making them more receptive and sensitive to picking out cancer cells.
Paul Y. Song, MD is currently CEO and Vice Chairman of NKGen Biotech. Dr. Song’s last clinical role was Asst. Professor at the Samuel Oschin Cancer Center at Cedars Sinai Medical Center.
Dr. Song served as the very first visiting fellow on healthcare policy in the California Department of Insurance in 2013. He is currently on the advisory board of the Pritzker School of Molecular Engineering at the University of Chicago and a board member of Mercy Corps, The Center for Health and Democracy, and Gideon’s Promise.
Dr. Song graduated with honors from the University of Chicago and received his MD from George Washington University. He completed his residency in radiation oncology at the University of Chicago where he served as Chief Resident and did a brachytherapy fellowship at the Institute Gustave Roussy in Villejuif, France. He was also awarded an ASTRO research fellowship in 1995 for his research in radiation inducible gene therapy.
With Dr. Song’s leadership, NKGen Biotech’s work on natural killer cells represents cutting-edge science leading to key findings and important pieces of the puzzle for treating two of humanity’s most intractable diseases.
Show links
- Paul Song LinkedIn
- NKGen Biotech on Twitter - @NKGenBiotech
- NKGen Website: https://nkgenbiotech.com/
- NKGen appoints Paul Song
- Patient Story: https://pix11.com/news/local-news/long-island/promising-new-treatment-for-advanced-alzheimers-patients/
- FDA Clearance: https://nkgenbiotech.com/nkgen-biotech-receives-ind-clearance-from-fda-for-snk02-allogeneic-natural-killer-cell-therapy-for-solid-tumors/Q3 earnings data: https://www.nasdaq.com/press-release/nkgen-biotech-inc.-reports-third-quarter-2023-financial-results-and-business