Shoot for the Moon: Its Surface Contains a Pot of Gold

An astronaut standing on the Moon.
Here's a riddle: What do the Moon, nuclear weapons, clean energy of the future, terrorism, and lung disease all have in common?
One goal of India's upcoming space probe is to locate deposits of helium-3 that are worth trillions of dollars.
The answer is helium-3, a gas that's extremely rare on Earth but 100 million times more abundant on the Moon. This past October, the Lockheed Martin corporation announced a concept for a lunar landing craft that may return humans to the Moon in the coming decade, and yesterday China successfully landed the Change-4 probe on the far side of the Moon. Landing inside the Moon's deepest crater, the Chinese achieved a first in space exploration history.
Meanwhile, later this month, India's Chandrayaan-2 space probe will also land on the lunar surface. One of its goals is to locate deposits of helium-3 that are worth trillions of dollars, because it could be a fuel for nuclear fusion energy to generate electricity or propel a rocket.
The standard way that nuclear engineers are trying to achieve sustainable fusion uses fuels that are more plentiful on Earth: deuterium and tritium. But MIT researchers have found that adding small amounts of helium-3 to the mix could make it much more efficient, and thus a viable energy source much sooner that once thought.
Even if fusion is proven practical tomorrow, any kind of nuclear energy involves long waits for power plant construction measured in decades. However, mining helium-3 could be useful now, because of its non-energy applications. A major one is its ability to detect neutrons coming from plutonium that could be used in terrorist attacks. Here's how it works: a small amount of helium-3 is contained within a forensic instrument. When a neutron hits an atom of helium-3, the reaction produces tritium, a proton, and an electrical charge, alerting investigators to the possibility that plutonium is nearby.
Ironically, as global concern about a potential for hidden nuclear material increased in the early 2000s, so did the supply of helium-3 on Earth. That's because helium-3 comes from the decay of tritium, used in thermonuclear warheads (H-bombs). Thousands of such weapons have been dismantled from U.S. and Russian arsenals, making helium-3 available for plutonium detection, research, and other applications--including in the world of healthcare.
Helium-3 can help doctors diagnose lung diseases, since it enables imaging of the lungs in real time.
Helium-3 dramatically improves the ability of doctors to image the lungs in a range of diseases including asthma, chronic obstructive pulmonary disease and emphysema, cystic fibrosis, and bronchopulmonary dysplasia, which happens particularly in premature infants. Specifically, helium-3 is useful in magnetic resonance imaging (MRI), a procedure that creates images from within the body for diagnostic purposes.
But while a standard MRI allows doctors to visualize parts of the body like the heart or brain, it's useless for seeing the lungs. Because lungs are filled with air, which is much less dense than water or fat, effectively no signals are produced that would enable imaging.
To compensate for this problem, a patient can inhale gas that is hyperpolarized –meaning enhanced with special procedures so that the magnetic resonance signals from the lungs are finally readable. This gas is safe to breathe when mixed with enough oxygen to support life. Helium-3 is one such gas that can be hyperpolarized; since it produces such a strong signal, the MRI can literally see the air inside the lungs and in all of the airways, revealing intricate details of the bronchopulmonary tree. And it can do this in real time
The capability to show anatomic details of the lungs and airways, and the ability to display functional imaging as a patient breathes, makes helium-3 MRI far better than the standard method of testing lung function. Called spirometry, this method tells physicians how the lungs function overall, but does not home in on particular areas that may be causing a problem. Plus, spirometry requires patients to follow instructions and hold their breath, so it is not great for testing young children with pulmonary disease.
In recent years, the cost of helium-3 on Earth has skyrocketed.
Over the past several years, researchers have been developing MRI for lung testing using other hyperpolarized gases. The main alternative to helium-3 is xenon-129. Over the years, researchers have learned to overcome certain disadvantages of the latter, such as its potential to put patients to sleep. Since helium-3 provides the strongest signal, though, it is still the best gas for MRI studies in many lung conditions.
But the supply of helium-3 on Earth has been decreasing in recent years, due to the declining rate of dismantling of warheads, just as the Department of Homeland Security has required more and more of the gas for neutron detection. As a result, the cost of the gas has skyrocketed. Less is available now for medical uses – unless, of course, we begin mining it on the moon.
The question is: Are the benefits worth the 239,000-mile trip?
The future of non-hormonal birth control: Antibodies can stop sperm in their tracks
Many women want non-hormonal birth control. A 22-year-old's findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
Unwanted pregnancy can now be added to the list of preventions that antibodies may be fighting in the near future. For decades, really since the 1980s, engineered monoclonal antibodies have been knocking out invading germs — preventing everything from cancer to COVID. Sperm, which have some of the same properties as germs, may be next.
Not only is there an unmet need on the market for alternatives to hormonal contraceptives, the genesis for the original research was personal for the then 22-year-old scientist who led it. Her findings were used to launch a company that could, within the decade, bring a new kind of contraceptive to the marketplace.
The genesis
It’s Suruchi Shrestha’s research — published in Science Translational Medicine in August 2021 and conducted as part of her dissertation while she was a graduate student at the University of North Carolina at Chapel Hill — that could change the future of contraception for many women worldwide. According to a Guttmacher Institute report, in the U.S. alone, there were 46 million sexually active women of reproductive age (15–49) who did not want to get pregnant in 2018. With the overturning of Roe v. Wade this year, Shrestha’s research could, indeed, be life changing for millions of American women and their families.
Now a scientist with NextVivo, Shrestha is not directly involved in the development of the contraceptive that is based on her research. But, back in 2016 when she was going through her own problems with hormonal contraceptives, she “was very personally invested” in her research project, Shrestha says. She was coping with a long list of negative effects from an implanted hormonal IUD. According to the Mayo Clinic, those can include severe pelvic pain, headaches, acute acne, breast tenderness, irregular bleeding and mood swings. After a year, she had the IUD removed, but it took another full year before all the side effects finally subsided; she also watched her sister suffer the “same tribulations” after trying a hormonal IUD, she says.
For contraceptive use either daily or monthly, Shrestha says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
Shrestha unshelved antibody research that had been sitting idle for decades. It was in the late 80s that scientists in Japan first tried to develop anti-sperm antibodies for contraceptive use. But, 35 years ago, “Antibody production had not been streamlined as it is now, so antibodies were very expensive,” Shrestha explains. So, they shifted away from birth control, opting to focus on developing antibodies for vaccines.
Over the course of the last three decades, different teams of researchers have been working to make the antibody more effective, bringing the cost down, though it’s still expensive, according to Shrestha. For contraceptive use either daily or monthly, she says, “You want the antibody to be very potent and also cheap.” That was her goal when she launched her study.
The problem
The problem with contraceptives for women, Shrestha says, is that all but a few of them are hormone-based or have other negative side effects. In fact, some studies and reports show that millions of women risk unintended pregnancy because of medical contraindications with hormone-based contraceptives or to avoid the risks and side effects. While there are about a dozen contraceptive choices for women, there are two for men: the condom, considered 98% effective if used correctly, and vasectomy, 99% effective. Neither of these choices are hormone-based.
On the non-hormonal side for women, there is the diaphragm which is considered only 87 percent effective. It works better with the addition of spermicides — Nonoxynol-9, or N-9 — however, they are detergents; they not only kill the sperm, they also erode the vaginal epithelium. And, there’s the non-hormonal IUD which is 99% effective. However, the IUD needs to be inserted by a medical professional, and it has a number of negative side effects, including painful cramping at a higher frequency and extremely heavy or “abnormal” and unpredictable menstrual flows.
The hormonal version of the IUD, also considered 99% effective, is the one Shrestha used which caused her two years of pain. Of course, there’s the pill, which needs to be taken daily, and the birth control ring which is worn 24/7. Both cause side effects similar to the other hormonal contraceptives on the market. The ring is considered 93% effective mostly because of user error; the pill is considered 99% effective if taken correctly.
“That’s where we saw this opening or gap for women. We want a safe, non-hormonal contraceptive,” Shrestha says. Compounding the lack of good choices, is poor access to quality sex education and family planning information, according to the non-profit Urban Institute. A focus group survey suggested that the sex education women received “often lacked substance, leaving them feeling unprepared to make smart decisions about their sexual health and safety,” wrote the authors of the Urban Institute report. In fact, nearly half (45%, or 2.8 million) of the pregnancies that occur each year in the US are unintended, reports the Guttmacher Institute. Globally the numbers are similar. According to a new report by the United Nations, each year there are 121 million unintended pregnancies, worldwide.
The science
The early work on antibodies as a contraceptive had been inspired by women with infertility. It turns out that 9 to 12 percent of women who are treated for infertility have antibodies that develop naturally and work against sperm. Shrestha was encouraged that the antibodies were specific to the target — sperm — and therefore “very safe to use in women.” She aimed to make the antibodies more stable, more effective and less expensive so they could be more easily manufactured.
Since antibodies tend to stick to things that you tell them to stick to, the idea was, basically, to engineer antibodies to stick to sperm so they would stop swimming. Shrestha and her colleagues took the binding arm of an antibody that they’d isolated from an infertile woman. Then, targeting a unique surface antigen present on human sperm, they engineered a panel of antibodies with as many as six to 10 binding arms — “almost like tongs with prongs on the tongs, that bind the sperm,” explains Shrestha. “We decided to add those grabbers on top of it, behind it. So it went from having two prongs to almost 10. And the whole goal was to have so many arms binding the sperm that it clumps it” into a “dollop,” explains Shrestha, who earned a patent on her research.
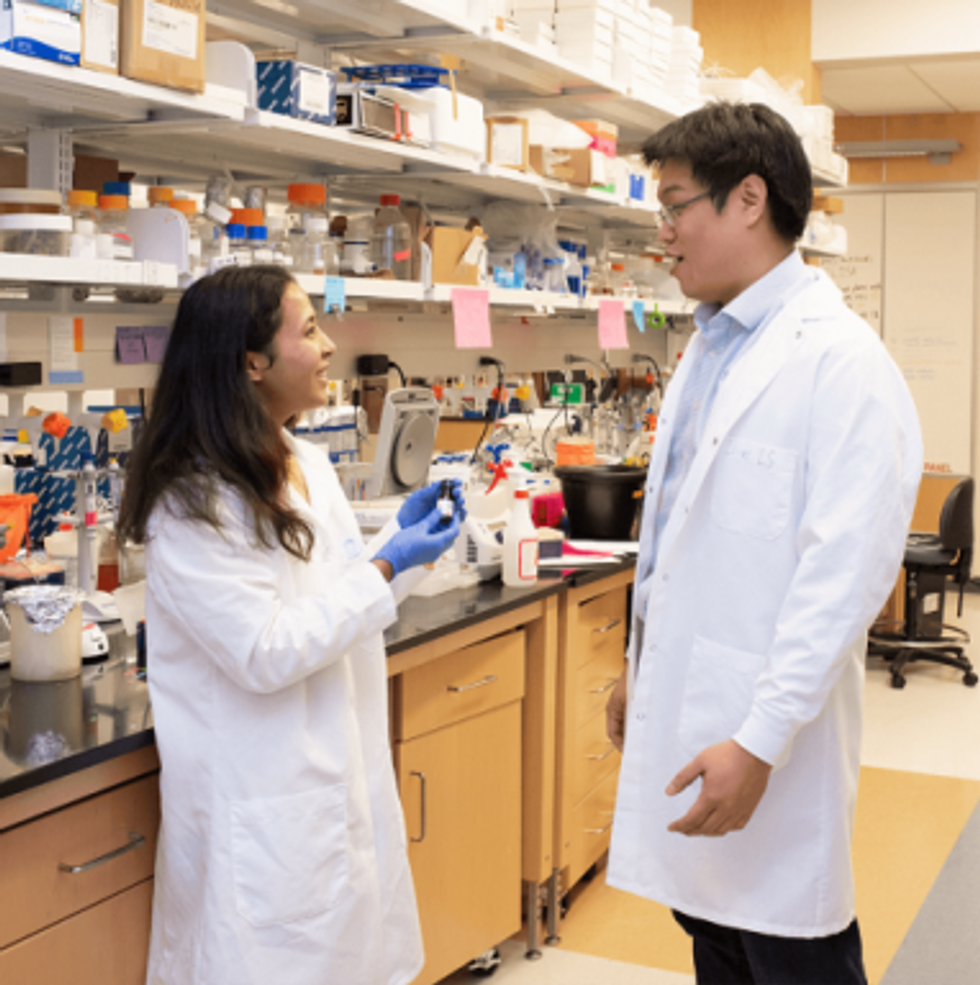
Suruchi Shrestha works in the lab with a colleague. In 2016, her research on antibodies for birth control was inspired by her own experience with side effects from an implanted hormonal IUD.
UNC - Chapel Hill
The sperm stays right where it met the antibody, never reaching the egg for fertilization. Eventually, and naturally, “Our vaginal system will just flush it out,” Shrestha explains.
“She showed in her early studies that [she] definitely got the sperm immotile, so they didn't move. And that was a really promising start,” says Jasmine Edelstein, a scientist with an expertise in antibody engineering who was not involved in this research. Shrestha’s team at UNC reproduced the effect in the sheep, notes Edelstein, who works at the startup Be Biopharma. In fact, Shrestha’s anti-sperm antibodies that caused the sperm to agglutinate, or clump together, were 99.9% effective when delivered topically to the sheep’s reproductive tracts.
The future
Going forward, Shrestha thinks the ideal approach would be delivering the antibodies through a vaginal ring. “We want to use it at the source of the spark,” Shrestha says, as opposed to less direct methods, such as taking a pill. The ring would dissolve after one month, she explains, “and then you get another one.”
Engineered to have a long shelf life, the anti-sperm antibody ring could be purchased without a prescription, and women could insert it themselves, without a doctor. “That's our hope, so that it is accessible,” Shrestha says. “Anybody can just go and grab it and not worry about pregnancy or unintended pregnancy.”
Her patented research has been licensed by several biotech companies for clinical trials. A number of Shrestha’s co-authors, including her lab advisor, Sam Lai, have launched a company, Mucommune, to continue developing the contraceptives based on these antibodies.
And, results from a small clinical trial run by researchers at Boston University Chobanian & Avedisian School of Medicine show that a dissolvable vaginal film with antibodies was safe when tested on healthy women of reproductive age. That same group of researchers earlier this year received a $7.2 million grant from the National Institute of Health for further research on monoclonal antibody-based contraceptives, which have also been shown to block transmission of viruses, like HIV.
“As the costs come down, this becomes a more realistic option potentially for women,” says Edelstein. “The impact could be tremendous.”
The Friday Five: An mRNA vaccine works against cancer, new research suggests
In this week's Friday Five, an mRNA vaccine works against cancer for the first time. Plus, these cameras inside the body have an unusual source of power, a new theory for what causes aging, bacteria that could get you excited to work out, and a reason for sex differences in Alzheimer's.
The Friday Five covers five stories in research that you may have missed this week. There are plenty of controversies and troubling ethical issues in science – and we get into many of them in our online magazine – but this news roundup focuses on scientific creativity and progress to give you a therapeutic dose of inspiration headed into the weekend.
Listen on Apple | Listen on Spotify | Listen on Stitcher | Listen on Amazon | Listen on Google
Here are the promising studies covered in this week's Friday Five:
- An mRNA vaccine that works against cancer
- These cameras inside the body have an unusual source of power
- A new theory for what causes aging
- Can bacteria make you excited to work out?
- Why women get Alzheimer's more often than men