Should You Bank Your Kid’s Teeth for Stem Cells?

When Karen Davis attended a presentation at a dental conference in 2013, she unexpectedly discovered a service that could help her daughter, Madeline: storing stem cells derived from her teeth that potentially could be used in the future to treat her Crohn's disease.
"Even though this isn't a viable option today, I know how rapidly things can change."
Throughout high school, Madeline suffered from the painful autoimmune disorder, which wreaks havoc on the gastrointestinal system and can lead to life-threatening complications.
"I leave no stone unturned when it comes to medical care and this resonated with me," says Davis, a Dallas-based dental hygienist who was encouraged by advances in stem cell research. Later that year, when Madeline got her wisdom teeth extracted, Davis shipped them off to the Store-A-Tooth company in Massachusetts, where they will be kept frozen until needed. "Even though this isn't a viable option today, I know how rapidly things can change," says Davis. "To me, this was a worthwhile investment—I didn't want to miss out on an opportunity that would provide a pathway to a cure."

Karen Davis pictured with her daughter Madeline.
(Courtesy of Karen Davis)
The process itself was straightforward. Madeline's newly extracted wisdom teeth--baby teeth can be saved, too—were bathed in a special solution, loaded into a Styrofoam container lined with cold packs and sent to the stem cell company. There, a team harvested the dental stem cells from the pulp, then grew them in culture and cryogenically preserved them. Store-A-Tooth charges $1500-1749 for tooth collection and $120 per year for storage, while other dental pulp stem cell tissue banks cost $500-$600 upfront and in the $120 range annually for storage.
The rationale here is that if you missed out on banking your baby's umbilical cord blood, this gives you another chance to harvest their stem cells. "If their child later develops an illness that could be managed or even cured with stem cell therapy, this is an insurance policy," says Amr Moursi, DDS, PhD, chair of the department of pediatric dentistry at New York University College of Dentistry.
But is there a genuine potential here for some effective treatments in the relatively near future—or is this just another trendy fad? Scientific opinion is decidedly mixed. Stem cells have been heralded as the next frontier in medicine because of their versatility: with a little chemical coaxing, they can be transformed into different cell types, such as heart, blood or brain cells, to create tissue that can mend damaged body parts. Because they're taken from your own body, there's little chance of rejection, which means patients don't have to take strong antirejection drugs that can have all sorts of unpleasant side effects for the rest of their lives.
However, while stem cells are immature cells found in different tissues, ranging from abdominal fat to bone marrow, there is a vast difference between the stem cells found in cord blood and in teeth. Cord blood, which is culled from the umbilical cord when a baby is born, contains what are called hematopoietic stem cells (HSCs), which can mature into other blood cells. These type of stem cells have already been approved by the U.S. Food and Drug Administration to treat patients—especially children--with blood cancers, such as leukemias and lymphomas, and certain blood disorders like sickle cell anemia.
In contrast, stem cells in teeth are called mesenchymal stem cells (MSCs), which are found in dental pulp, the tissue in the center of the tooth that's filled with nerves and blood vessels. MSCs are adult stem cells normally found in the bone marrow that can transform into bone, fat, and cartilage cells, and also aid in the formation of blood stem cells.
"Right now we just don't have rigorous evidence that they can be used in that fashion and have real benefit."
Small studies on lab animals suggest that MSCs secrete growth factors—hormonal steroids or proteins—that can nurture ailing cells, act as powerful anti-inflammatory agents that could tame autoimmune disorders like the one that plagues Karen Davis's daughter, and may even generate new nerve and muscle tissue. Preliminary research suggests they potentially could treat medical conditions as varied as heart disease, spinal cord injury and type 1 diabetes by generating new cells, which can replace damaged or dead cells.
But this is all very early research and there's a vast difference between how cells behave in the tightly controlled environment of a lab versus the real world in a diverse population of human patients. "Right now we just don't have rigorous evidence that they can be used in that fashion and have real benefit," says Pamela G. Robey, PhD, chief of the skeletal biology section at the National Institute of Dental and Craniofacial Research at the National Institutes of Health.
Robey should know—she headed the research team that discovered stem cells in human baby teeth and in wisdom teeth more than fifteen years ago. She believes prospects are better using these stem cells for tooth repair: research suggests they may be able to fix cracked teeth, repair bone defects caused by gum disease, or in root canal therapy, where they can be used to replace infected tissue with regenerated healthy pulp.
In the meantime, though, there are no clinical applications for MSCs. "These tooth banking companies aren't doing their own research," says Leigh Turner, a bioethicist at the University of Minnesota who monitors stem cell clinics. "They cobble together reports of early research in humans or from animal studies in an effort to provide a narrative to make it seem like it is evidence based."
Still, in all fairness, tooth banking companies aren't making the kind of extravagant claims made by stem cell clinics, which operate in a gray area of the law and purport to treat everything from chronic lung disease to Alzheimer's. "We don't know when therapies will be available using these cells because the pace of research is hard to predict," says Peter Verlander, PhD, a molecular geneticist and chief scientific officer of Provia Laboratories, the parent company of Store-A-Tooth. "But for parents who regretted not banking their child's cord blood, especially if they later develop a disease like diabetes, this is another opportunity."
But the jury is still out if this is truly a good investment. Moursi, a national spokesperson for the American Academy of Pediatric Dentistry who fields queries about this practice from a dozen or so families a year, concludes: "If you could afford it, and know the risks, benefits and current limitations, then it is something to consider."
Nobel Prize goes to technology for mRNA vaccines
Katalin Karikó, pictured, and Drew Weissman won the Nobel Prize for advances in mRNA research that led to the first Covid vaccines.
When Drew Weissman received a call from Katalin Karikó in the early morning hours this past Monday, he assumed his longtime research partner was calling to share a nascent, nagging idea. Weissman, a professor of medicine at the Perelman School of Medicine at the University of Pennsylvania, and Karikó, a professor at Szeged University and an adjunct professor at UPenn, both struggle with sleep disturbances. Thus, middle-of-the-night discourses between the two, often over email, has been a staple of their friendship. But this time, Karikó had something more pressing and exciting to share: They had won the 2023 Nobel Prize in Physiology or Medicine.
The work for which they garnered the illustrious award and its accompanying $1,000,000 cash windfall was completed about two decades ago, wrought through long hours in the lab over many arduous years. But humanity collectively benefited from its life-saving outcome three years ago, when both Moderna and Pfizer/BioNTech’s mRNA vaccines against COVID were found to be safe and highly effective at preventing severe disease. Billions of doses have since been given out to protect humans from the upstart viral scourge.
“I thought of going somewhere else, or doing something else,” said Katalin Karikó. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
Unlocking the power of mRNA
Weissman and Karikó unlocked mRNA vaccines for the world back in the early 2000s when they made a key breakthrough. Messenger RNA molecules are essentially instructions for cells’ ribosomes to make specific proteins, so in the 1980s and 1990s, researchers started wondering if sneaking mRNA into the body could trigger cells to manufacture antibodies, enzymes, or growth agents for protecting against infection, treating disease, or repairing tissues. But there was a big problem: injecting this synthetic mRNA triggered a dangerous, inflammatory immune response resulting in the mRNA’s destruction.
While most other researchers chose not to tackle this perplexing problem to instead pursue more lucrative and publishable exploits, Karikó stuck with it. The choice sent her academic career into depressing doldrums. Nobody would fund her work, publications dried up, and after six years as an assistant professor at the University of Pennsylvania, Karikó got demoted. She was going backward.
“I thought of going somewhere else, or doing something else,” Karikó told Stat in 2020. “I also thought maybe I’m not good enough, not smart enough. I tried to imagine: Everything is here, and I just have to do better experiments.”
A tale of tenacity
Collaborating with Drew Weissman, a new professor at the University of Pennsylvania, in the late 1990s helped provide Karikó with the tenacity to continue. Weissman nurtured a goal of developing a vaccine against HIV-1, and saw mRNA as a potential way to do it.
“For the 20 years that we’ve worked together before anybody knew what RNA is, or cared, it was the two of us literally side by side at a bench working together,” Weissman said in an interview with Adam Smith of the Nobel Foundation.
In 2005, the duo made their 2023 Nobel Prize-winning breakthrough, detailing it in a relatively small journal, Immunity. (Their paper was rejected by larger journals, including Science and Nature.) They figured out that chemically modifying the nucleoside bases that make up mRNA allowed the molecule to slip past the body’s immune defenses. Karikó and Weissman followed up that finding by creating mRNA that’s more efficiently translated within cells, greatly boosting protein production. In 2020, scientists at Moderna and BioNTech (where Karikó worked from 2013 to 2022) rushed to craft vaccines against COVID, putting their methods to life-saving use.
The future of vaccines
Buoyed by the resounding success of mRNA vaccines, scientists are now hurriedly researching ways to use mRNA medicine against other infectious diseases, cancer, and genetic disorders. The now ubiquitous efforts stand in stark contrast to Karikó and Weissman’s previously unheralded struggles years ago as they doggedly worked to realize a shared dream that so many others shied away from. Katalin Karikó and Drew Weissman were brave enough to walk a scientific path that very well could have ended in a dead end, and for that, they absolutely deserve their 2023 Nobel Prize.
This article originally appeared on Big Think, home of the brightest minds and biggest ideas of all time.
Scientists turn pee into power in Uganda
With conventional fuel cells as their model, researchers learned to use similar chemical reactions to make a fuel from microbes in pee.
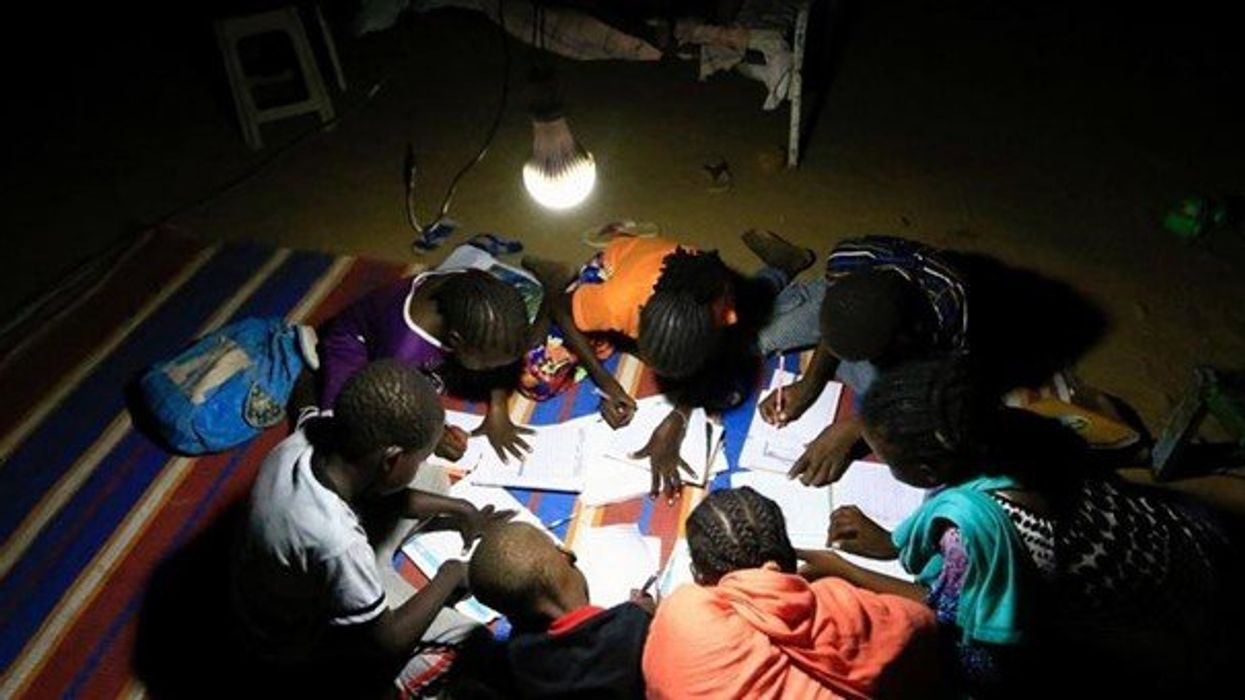
At the edge of a dirt road flanked by trees and green mountains outside the town of Kisoro, Uganda, sits the concrete building that houses Sesame Girls School, where girls aged 11 to 19 can live, learn and, at least for a while, safely use a toilet. In many developing regions, toileting at night is especially dangerous for children. Without electrical power for lighting, kids may fall into the deep pits of the latrines through broken or unsteady floorboards. Girls are sometimes assaulted by men who hide in the dark.
For the Sesame School girls, though, bright LED lights, connected to tiny gadgets, chased the fears away. They got to use new, clean toilets lit by the power of their own pee. Some girls even used the light provided by the latrines to study.
Urine, whether animal or human, is more than waste. It’s a cheap and abundant resource. Each day across the globe, 8.1 billion humans make 4 billion gallons of pee. Cows, pigs, deer, elephants and other animals add more. By spending money to get rid of it, we waste a renewable resource that can serve more than one purpose. Microorganisms that feed on nutrients in urine can be used in a microbial fuel cell that generates electricity – or "pee power," as the Sesame girls called it.
Plus, urine contains water, phosphorus, potassium and nitrogen, the key ingredients plants need to grow and survive. Human urine could replace about 25 percent of current nitrogen and phosphorous fertilizers worldwide and could save water for gardens and crops. The average U.S. resident flushes a toilet bowl containing only pee and paper about six to seven times a day, which adds up to about 3,500 gallons of water down per year. Plus cows in the U.S. produce 231 gallons of the stuff each year.
Pee power
A conventional fuel cell uses chemical reactions to produce energy, as electrons move from one electrode to another to power a lightbulb or phone. Ioannis Ieropoulos, a professor and chair of Environmental Engineering at the University of Southampton in England, realized the same type of reaction could be used to make a fuel from microbes in pee.
Bacterial species like Shewanella oneidensis and Pseudomonas aeruginosa can consume carbon and other nutrients in urine and pop out electrons as a result of their digestion. In a microbial fuel cell, one electrode is covered in microbes, immersed in urine and kept away from oxygen. Another electrode is in contact with oxygen. When the microbes feed on nutrients, they produce the electrons that flow through the circuit from one electrod to another to combine with oxygen on the other side. As long as the microbes have fresh pee to chomp on, electrons keep flowing. And after the microbes are done with the pee, it can be used as fertilizer.
These microbes are easily found in wastewater treatment plants, ponds, lakes, rivers or soil. Keeping them alive is the easy part, says Ieropoulos. Once the cells start producing stable power, his group sequences the microbes and keeps using them.
Like many promising technologies, scaling these devices for mass consumption won’t be easy, says Kevin Orner, a civil engineering professor at West Virginia University. But it’s moving in the right direction. Ieropoulos’s device has shrunk from the size of about three packs of cards to a large glue stick. It looks and works much like a AAA battery and produce about the same power. By itself, the device can barely power a light bulb, but when stacked together, they can do much more—just like photovoltaic cells in solar panels. His lab has produced 1760 fuel cells stacked together, and with manufacturing support, there’s no theoretical ceiling, he says.
Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofit into urban wastewater utilities.
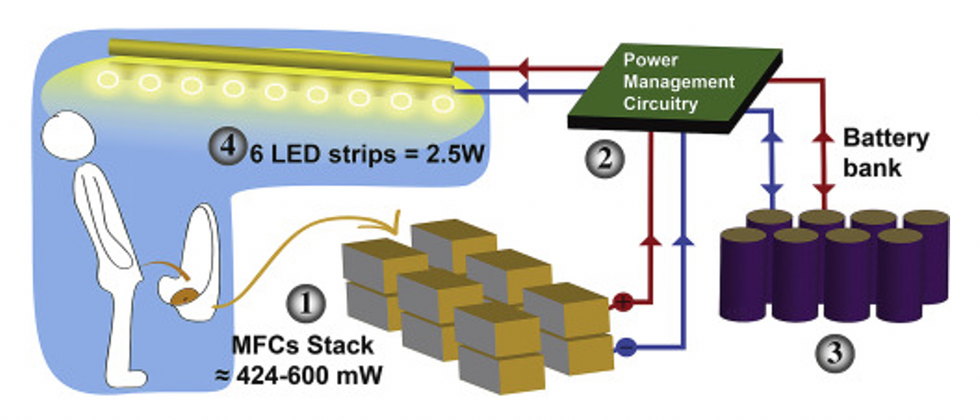
This image shows how the pee-powered system works. Pee feeds bacteria in the stack of fuel cells (1), which give off electrons (2) stored in parallel cylindrical cells (3). These cells are connected to a voltage regulator (4), which smooths out the electrical signal to ensure consistent power to the LED strips lighting the toilet.
Courtesy Ioannis Ieropoulos
Key to the long-term success of any urine reclamation effort, says Orner, is avoiding what he calls “parachute engineering”—when well-meaning scientists solve a problem with novel tech and then abandon it. “The way around that is to have either the need come from the community or to have an organization in a community that is committed to seeing a project operate and maintained,” he says.
Success with urine reclamation also depends on the economy. “If energy prices are low, it may not make sense to recover energy,” says Orner. “But right now, fertilizer prices worldwide are generally pretty high, so it may make sense to recover fertilizer and nutrients.” There are obstacles, too, such as few incentives for builders to incorporate urine recycling into new construction. And any hiccups like leaks or waste seepage will cost builders money and reputation. Right now, Orner says, the risks are just too high.
Despite the challenges, Ieropoulos envisions a future in which urine is passed through microbial fuel cells at wastewater treatment plants, retrofitted septic tanks, and building basements, and is then delivered to businesses to use as agricultural fertilizers. Although pure urine produces the most power, Ieropoulos’s devices also work with the mixed liquids of the wastewater treatment plants, so they can be retrofitted into urban wastewater utilities where they can make electricity from the effluent. And unlike solar cells, which are a common target of theft in some areas, nobody wants to steal a bunch of pee.
When Ieropoulos’s team returned to wrap up their pilot project 18 months later, the school’s director begged them to leave the fuel cells in place—because they made a major difference in students’ lives. “We replaced it with a substantial photovoltaic panel,” says Ieropoulos, They couldn’t leave the units forever, he explained, because of intellectual property reasons—their funders worried about theft of both the technology and the idea. But the photovoltaic replacement could be stolen, too, leaving the girls in the dark.
The story repeated itself at another school, in Nairobi, Kenya, as well as in an informal settlement in Durban, South Africa. Each time, Ieropoulos vowed to return. Though the pandemic has delayed his promise, he is resolute about continuing his work—it is a moral and legal obligation. “We've made a commitment to ourselves and to the pupils,” he says. “That's why we need to go back.”
Urine as fertilizer
Modern day industrial systems perpetuate the broken cycle of nutrients. When plants grow, they use up nutrients the soil. We eat the plans and excrete some of the nutrients we pass them into rivers and oceans. As a result, farmers must keep fertilizing the fields while our waste keeps fertilizing the waterways, where the algae, overfertilized with nitrogen, phosphorous and other nutrients grows out of control, sucking up oxygen that other marine species need to live. Few global communities remain untouched by the related challenges this broken chain create: insufficient clean water, food, and energy, and too much human and animal waste.
The Rich Earth Institute in Vermont runs a community-wide urine nutrient recovery program, which collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms.
One solution to this broken cycle is reclaiming urine and returning it back to the land. The Rich Earth Institute in Vermont is one of several organizations around the world working to divert and save urine for agricultural use. “The urine produced by an adult in one day contains enough fertilizer to grow all the wheat in one loaf of bread,” states their website.
Notably, while urine is not entirely sterile, it tends to harbor fewer pathogens than feces. That’s largely because urine has less organic matter and therefore less food for pathogens to feed on, but also because the urinary tract and the bladder have built-in antimicrobial defenses that kill many germs. In fact, the Rich Earth Institute says it’s safe to put your own urine onto crops grown for home consumption. Nonetheless, you’ll want to dilute it first because pee usually has too much nitrogen and can cause “fertilizer burn” if applied straight without dilution. Other projects to turn urine into fertilizer are in progress in Niger, South Africa, Kenya, Ethiopia, Sweden, Switzerland, The Netherlands, Australia, and France.
Eleven years ago, the Institute started a program that collects urine from homes and businesses, transports it for processing, and then supplies it as fertilizer to local farms. By 2021, the program included 180 donors producing over 12,000 gallons of urine each year. This urine is helping to fertilize hay fields at four partnering farms. Orner, the West Virginia professor, sees it as a success story. “They've shown how you can do this right--implementing it at a community level scale."