Alzheimer’s prevention may be less about new drugs, more about income, zip code and education

(Left to right) Vickie Naylor, Bernadine Clay, and Donna Maxey read a memory prompt as they take part in the Sharing History through Active Reminiscence and Photo-Imagery (SHARP) study, September 20, 2017.
That your risk of Alzheimer’s disease depends on your salary, what you ate as a child, or the block where you live may seem implausible. But researchers are discovering that social determinants of health (SDOH) play an outsized role in Alzheimer’s disease and related dementias, possibly more than age, and new strategies are emerging for how to address these factors.
At the 2022 Alzheimer’s Association International Conference, a series of presentations offered evidence that a string of socioeconomic factors—such as employment status, social support networks, education and home ownership—significantly affected dementia risk, even when adjusting data for genetic risk. What’s more, memory declined more rapidly in people who earned lower wages and slower in people who had parents of higher socioeconomic status.
In 2020, a first-of-its kind study in JAMA linked Alzheimer’s incidence to “neighborhood disadvantage,” which is based on SDOH indicators. Through autopsies, researchers analyzed brain tissue markers related to Alzheimer’s and found an association with these indicators. In 2022, Ryan Powell, the lead author of that study, published further findings that neighborhood disadvantage was connected with having more neurofibrillary tangles and amyloid plaques, the main pathological features of Alzheimer's disease.
As of yet, little is known about the biological processes behind this, says Powell, director of data science at the Center for Health Disparities Research at the University of Wisconsin School of Medicine and Public Health. “We know the association but not the direct causal pathway.”
The corroborative findings keep coming. In a Nature study published a few months after Powell’s study, every social determinant investigated affected Alzheimer’s risk except for marital status. The links were highest for income, education, and occupational status.
Clinical trials on new Alzheimer’s medications get all the headlines but preventing dementia through policy and public health interventions should not be underestimated.
The potential for prevention is significant. One in three older adults dies with Alzheimer's or another dementia—more than breast and prostate cancers combined. Further, a 2020 report from the Lancet Commission determined that about 40 percent of dementia cases could theoretically be prevented or delayed by managing the risk factors that people can modify.
Take inactivity. Older adults who took 9,800 steps daily were half as likely to develop dementia over the next 7 years, in a 2022 JAMA study. Hearing loss, another risk factor that can be managed, accounts for about 9 percent of dementia cases.
Clinical trials on new Alzheimer’s medications get all the headlines but preventing dementia through policy and public health interventions should not be underestimated. Simply slowing the course of Alzheimer’s or delaying its onset by five years would cut the incidence in half, according to the Global Council on Brain Health.
Minorities Hit the Hardest
The World Health Organization defines SDOH as “conditions in which people are born, work, live, and age, and the wider set of forces and systems shaping the conditions of daily life.”
Anyone who exists on processed food, smokes cigarettes, or skimps on sleep has heightened risks for dementia. But minority groups get hit harder. Older Black Americans are twice as likely to have Alzheimer’s or another form of dementia as white Americans; older Hispanics are about one and a half times more likely.
This is due in part to higher rates of diabetes, obesity, and high blood pressure within these communities. These diseases are linked to Alzheimer’s, and SDOH factors multiply the risks. Blacks and Hispanics earn less income on average than white people. This means they are more likely to live in neighborhoods with limited access to healthy food, medical care, and good schools, and suffer greater exposure to noise (which impairs hearing) and air pollution—additional risk factors for dementia.
Related Reading: The Toxic Effects of Noise and What We're Not Doing About it
Plus, when Black people are diagnosed with dementia, their cognitive impairment and neuropsychiatric symptom are more advanced than in white patients. Why? Some African-Americans delay seeing a doctor because of perceived discrimination and a sense they will not be heard, says Carl V. Hill, chief diversity, equity, and inclusion officer at the Alzheimer’s Association.
Misinformation about dementia is another issue in Black communities. The thinking is that Alzheimer’s is genetic or age-related, not realizing that diet and physical activity can improve brain health, Hill says.
African Americans are severely underrepresented in clinical trials for Alzheimer’s, too. So, researchers miss the opportunity to learn more about health disparities. “It’s a bioethical issue,” Hill says. “The people most likely to have Alzheimer’s aren’t included in the trials.”
The Cure: Systemic Change
People think of lifestyle as a choice but there are limitations, says Muniza Anum Majoka, a geriatric psychiatrist and assistant professor of psychiatry at Yale University, who published an overview of SDOH factors that impact dementia. “For a lot of people, those choices [to improve brain health] are not available,” she says. If you don’t live in a safe neighborhood, for example, walking for exercise is not an option.
Hill wants to see the focus of prevention shift from individual behavior change to ensuring everyone has access to the same resources. Advice about healthy eating only goes so far if someone lives in a food desert. Systemic change also means increasing the number of minority physicians and recruiting minorities in clinical drug trials so studies will be relevant to these communities, Hill says.
Based on SDOH impact research, raising education levels has the most potential to prevent dementia. One theory is that highly educated people have a greater brain reserve that enables them to tolerate pathological changes in the brain, thus delaying dementia, says Majoka. Being curious, learning new things and problem-solving also contribute to brain health, she adds. Plus, having more education may be associated with higher socioeconomic status, more access to accurate information and healthier lifestyle choices.
New Strategies
The chasm between what researchers know about brain health and how the knowledge is being applied is huge. “There’s an explosion of interest in this area. We’re just in the first steps,” says Powell. One day, he predicts that physicians will manage Alzheimer’s through precision medicine customized to the patient’s specific risk factors and needs.
Raina Croff, assistant professor of neurology at Oregon Health & Science University School of Medicine, created the SHARP (Sharing History through Active Reminiscence and Photo-imagery) walking program to forestall memory loss in African Americans with mild cognitive impairment or early dementia.
Participants and their caregivers walk in historically black neighborhoods three times a week over six months. A smart tablet provides information about “Memory Markers” they pass, such as the route of a civil rights march. People celebrate their community and culture while “brain health is running in the background,” Croff says.

Photos and memory prompts engage participants in the SHARP program.
OHSU/Kristyna Wentz-Graff
The project began in 2015 as a pilot study in Croff’s hometown of Portland, Ore., expanded to Seattle, and will soon start in Oakland, Calif. “Walking is good for slowing [brain] decline,” she says. A post-study assessment of 40 participants in 2017 showed that half had higher cognitive scores after the program; 78 percent had lower blood pressure; and 44 percent lost weight. Those with mild cognitive impairment showed the most gains. The walkers also reported improved mood and energy along with increased involvement in other activities.
It’s never too late to reap the benefits of working your brain and being socially engaged, Majoka says.
In Milwaukee, the Wisconsin Alzheimer’s Institute launched the The Amazing Grace Chorus® to stave off cognitive decline in seniors. People in early stages of Alzheimer’s practice and perform six concerts each year. The activity provides opportunities for social engagement, mental stimulation, and a support network. Among the benefits, 55 percent reported better communication at home and nearly half of participants said they got involved with more activities after participating in the chorus.
Private companies are offering intervention services to healthcare providers and insurers to manage SDOH, too. One such service, MyHello, makes calls to at-risk people to assess their needs—be it food, transportation or simply a friendly voice. Having a social support network is critical for seniors, says Majoka, noting there was a steep decline in cognitive function among isolated elders during Covid lockdowns.
About 1 in 9 Americans age 65 or older live with Alzheimer’s today. With a surge in people with the disease predicted, public health professionals have to think more broadly about resource targets and effective intervention points, Powell says.
Beyond breakthrough pills, that is. Like Dorothy in Kansas discovering happiness was always in her own backyard, we are beginning to learn that preventing Alzheimer’s is in our reach if only we recognized it.
Kirstie Ennis, an Afghanistan veteran who survived a helicopter crash but lost a limb, pictured in May 2021 at Two Rivers Park in Colorado.
In June 2012, Kirstie Ennis was six months into her second deployment to Afghanistan and recently promoted to sergeant. The helicopter gunner and seven others were three hours into a routine mission of combat resupplies and troop transport when their CH-53D helicopter went down hard.
Miraculously, all eight people onboard survived, but Ennis' injuries were many and severe. She had a torn rotator cuff, torn labrum, crushed cervical discs, facial fractures, deep lacerations and traumatic brain injury. Despite a severely fractured ankle, doctors managed to save her foot, for a while at least.
In November 2015, after three years of constant pain and too many surgeries to count, Ennis relented. She elected to undergo a lower leg amputation but only after she completed the 1,000-mile, 72-day Walking with the Wounded journey across the UK.
On Veteran's Day of that year, on the other side of the country, orthopedic surgeon Cato Laurencin announced a moonshot challenge he was setting out to achieve on behalf of wounded warriors like Ennis: the Hartford Engineering A Limb (HEAL) Project.
Laurencin, who is a University of Connecticut professor of chemical, materials and biomedical engineering, teamed up with experts in tissue bioengineering and regenerative medicine from Harvard, Columbia, UC Irvine and SASTRA University in India. Laurencin and his colleagues at the Connecticut Convergence Institute for Translation in Regenerative Engineering made a bold commitment to regenerate an entire limb within 15 years – by the year 2030.
Dr. Cato Laurencin pictured in his office at UConn.
Photo Credit: UConn
Regenerative Engineering -- A Whole New Field
Limb regeneration in humans has been a medical and scientific fascination for decades, with little to show for the effort. However, Laurencin believes that if we are to reach the next level of 21st century medical advances, this puzzle must be solved.
An estimated 185,000 people undergo upper or lower limb amputation every year. Despite the significant advances in electromechanical prosthetics, these individuals still lack the ability to perform complex functions such as sensation for tactile input, normal gait and movement feedback. As far as Laurencin is concerned, the only clinical answer that makes sense is to regenerate a whole functional limb.
Laurencin feels other regeneration efforts were hampered by their siloed research methods with chemists, surgeons, engineers all working separately. Success, he argues, requires a paradigm shift to a trans-disciplinary approach that brings together cutting-edge technologies from disparate fields such as biology, material sciences, physical, chemical and engineering sciences.
As the only surgeon ever inducted into the academies of Science, Medicine and Innovation, Laurencin is uniquely suited for the challenge. He is regarded as the founder of Regenerative Engineering, defined as the convergence of advanced materials sciences, stem cell sciences, physics, developmental biology and clinical translation for the regeneration of complex tissues and organ systems.
But none of this is achievable without early clinician participation across scientific fields to develop new technologies and a deeper understanding of how to harness the body's innate regenerative capabilities. "When I perform a surgical procedure or something is torn or needs to be repaired, I count on the body being involved in regenerating tissue," he says. "So, understanding how the body works to regenerate itself and harnessing that ability is an important factor for the regeneration process."
The Birth of the Vision
Laurencin's passion for regeneration began when he was a sports medicine fellow at Cornell University Medical Center in the early 1990s. There he saw a significant number of injuries to the anterior cruciate ligament (ACL), the major ligament that stabilizes the knee. He believed he could develop a better way to address those injuries using biomaterials to regenerate the ligament. He sketched out a preliminary drawing on a napkin one night over dinner. He has spent the next 30 years regenerating tissues, including the patented L-C ligament.
As chair of Orthopaedic Surgery at the University of Virginia during the peak of the wars in Iraq and Afghanistan, Laurencin treated military personnel who survived because of improved helmets, body armor and battlefield medicine but were left with more devastating injuries, including traumatic brain injuries and limb loss.
"I was so honored to care for them and I so admired their steadfast courage that I became determined to do something big for them," says Laurencin.
When he tells people about his plans to regrow a limb, he gets a lot of eye rolls, which he finds amusing but not discouraging. Growing bone cells was relatively new when he was first focused on regenerating bone in 1987 at MIT; in 2007 he was well on his way to regenerating ligaments at UVA when many still doubted that ligaments could even be reconstructed. He and his team have already regenerated torn rotator cuff tendons and ACL ligaments using a nano-textured fabric seeded with stem cells.
Even as a finalist for the $4 million NIH Pioneer Award for high-risk/high-reward research, he faced a skeptical scientific audience in 2014. "They said, 'Well what do you plan to do?' I said 'I plan to regenerate a whole limb in people.' There was a lot of incredulousness. They stared at me and asked a lot of questions. About three days later, I received probably the best score I've ever gotten on an NIH grant."
In the Thick of the Science
Humans are born with regenerative abilities--two-year-olds have regrown fingertips--but lose that ability with age. Salamanders are the only vertebrates that can regenerate lost body parts as adults; axolotl, the rare Mexican salamander, can grow extra limbs.
The axolotl is important as a model organism because it is a four-footed vertebrate with a similar body plan to humans. Mapping the axolotl genome in 2018 enhanced scientists' genetic understanding of their evolution, development, and regeneration. Being easy to breed in captivity allowed the HEAL team to closely study these amphibians and discover a new cell type they believe may shed light on how to mimic the process in humans.
"Whenever limb regeneration takes place in the salamander, there is a huge amount of something called heparan sulfate around that area," explains Laurencin. "We thought, 'What if this heparan sulfate is the key ingredient to allowing regeneration to take place?' We found these groups of cells that were interspersed in tissues during the time of regeneration that seemed to have connections to each other that expressed this heparan sulfate."
Called GRID (Groups that are Regenerative, Interspersed and Dendritic), these cells were also recently discovered in mice. While GRID cells don't regenerate as well in mice as in salamanders, finding them in mammals was significant.
"If they're found in mice. we might be able to find these in humans in some form," Laurencin says. "We think maybe it will help us figure out regeneration or we can create cells that mimic what grid cells do and create an artificial grid cell."
What Comes Next?
Laurencin and his team have individually engineered and made every single tissue in the lower limb, including bone, cartilage, ligament, skin, nerve, blood vessels. Regenerating joints and joint tissue is the next big mile marker, which Laurencin sees as essential to regenerating a limb that functions and performs in the way he envisions.
"Using stem cells and amnion tissue, we can regenerate joints that are damaged, and have severe arthritis," he says. "We're making progress on all fronts, and making discoveries we believe are going to be helping people along the way."
That focus and advancement is vital to Ennis. After laboring over the decision to have her leg amputated below the knee, she contracted MRSA two weeks post-surgery. In less than a month, she went from a below-the-knee-amputee to a through-the-knee amputee to an above-the-knee amputee.
"A below-the-knee amputation is night-and-day from above-the-knee," she said. "You have to relearn everything. You're basically a toddler."

Kirstie Ennis pictured in July 2020.
Photo Credit: Ennis' Instagram
The clock is ticking on the timeline Laurencin set for himself. Nine years might seem like forever if you're doing time but it might appear fleeting when you're trying to create something that's never been done before. But Laurencin isn't worried. He's convinced time is on his side.
"Every week, I receive an email or a call from someone, maybe a mother whose child has lost a finger or I'm in communication with a disabled American veteran who wants to know how the progress is going. That energizes me to continue to work hard to try to create these sorts of solutions because we're talking about people and their lives."
He devotes about 60 hours a week to the project and the roughly 100 students, faculty and staff who make up the HEAL team at the Convergence Institute seem acutely aware of what's at stake and appear equally dedicated.
"We're in the thick of the science in terms of making this happen," says Laurencin. "We've moved from making the impossible possible to making the possible a reality. That's what science is all about."
7 Reasons Why We Should Not Need Boosters for COVID-19
A top infectious disease physician explains why immunity derived from natural infection and the vaccines should be long-lasting.
There are at least 7 reasons why immunity after vaccination or infection with COVID-19 should likely be long-lived. If durable, I do not think boosters will be necessary in the future, despite CEOs of pharmaceutical companies (who stand to profit from boosters) messaging that they may and readying such boosters. To explain these reasons, let's orient ourselves to the main components of the immune system.
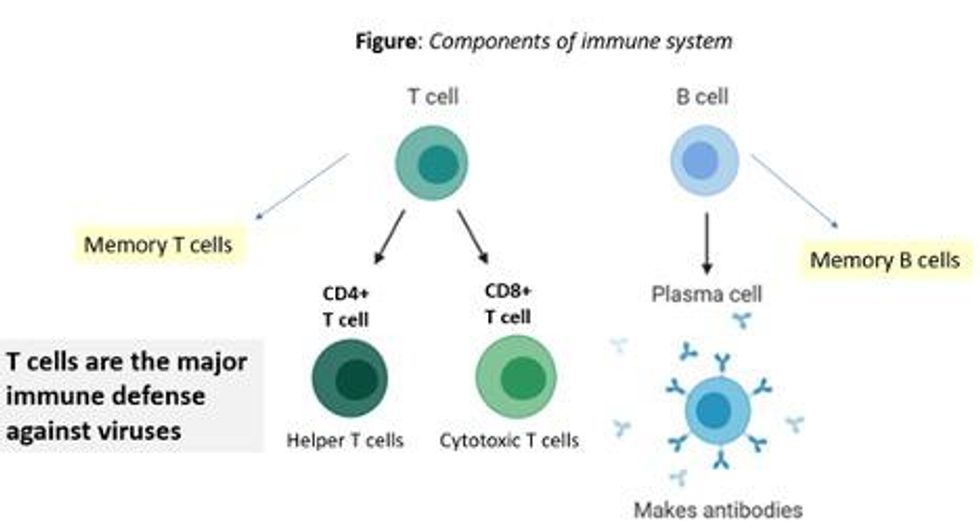
There are two major arms of the immune system: B cells (which produce antibodies) and T cells (which are formed specifically to attack and kill pathogens). T cells are divided into two types, CD4 cells ("helper" T cells) and CD8 cells ("cytotoxic" T cells).
Each arm, once stimulated by infection or vaccine, should hopefully make "memory" banks. So if the body sees the pathogen in the future, these defenses should come roaring back to attack the virus and protect you from getting sick. Plenty of research in COVID-19 indicates a likely long-lasting response to the vaccine or infection. Here are seven of the most compelling reasons:
REASON 1: Memory B Cells Are Produced By Vaccines and Natural Infection
In one study, 12 volunteers who had never had Covid-19--and were fully vaccinated with two Pfizer/BioNTech shots-- underwent biopsies of their lymph nodes. This is where memory B cells are stored in places called "germinal centers". The biopsies were performed three, four, six, and seven weeks after the first mRNA vaccine shot, and were stained to reveal that germinal center memory B cells in the lymph nodes increased in concentration over time.
Natural infection also generates memory B cells. Even after antibody levels wane over time, strong memory B cells were detected in the blood of individuals six and eight months after infection in different studies. Indeed, the half-lives of the memory B cells seen in the study examining patients 8 months after COVID-19 led the authors to conclude that "B cell memory to SARS-CoV-2 was robust and is likely long-lasting." Reason #2 tells us that memory B cells can be active for a very long time indeed.
REASON #2: Memory B Cells Can Produce Neutralizing Antibodies If They See Infection Again Decades Later
Demonstrated production of memory B cells after vaccination or natural infection with COVID-19 is so important because memory B cells, once generated, can be activated to produce high levels of neutralizing antibodies against the pathogen even if encountered many years after the initial exposure. In one amazing study (published in 2008), researchers isolated memory B cells against the 1918 flu strain from the blood of 32 individuals aged 91-101 years. These people had been born on or before 1915 and had survived that pandemic.
Their memory B cells, when exposed to the 1918 flu strain in a test tube, generated high levels of neutralizing antibodies against the virus -- antibodies that then protected mice from lethal infection with this deadly strain. The ability of memory B cells to produce complex antibody responses against an infection nine decades after exposure speaks to their durability.
REASON #3: Vaccines or Natural Infection Trigger Strong Memory T Cell Immunity
All of the trials of the major COVID-19 vaccine candidates measured strong T cell immunity following vaccination, most often assessed by measuring SARS-CoV-2 specific T cells in the phase I/II safety and immunogenicity studies. There are a number of studies that demonstrate the production of strong T cell immunity to COVID-19 after natural infection as well, even when the infection was mild or asymptomatic.
The same study that showed us robust memory B cell production 8 months after natural infection also demonstrated strong and sustained memory T cell production. In fact, the half-lives of the memory T cells in this cohort were long (~125-225 days for CD8+ and ~94-153 days for CD4+ T cells), comparable to the 123-day half-life observed for memory CD8+ T cells after yellow fever immunization (a vaccine usually given once over a lifetime).
A recent study of individuals recovered from COVID-19 show that the initial T cells generated by natural infection mature and differentiate over time into memory T cells that will be "put in the bank" for sustained periods.
REASON #4: T Cell Immunity Following Vaccinations for Other Infections Is Long-Lasting
Last year, we were fortunate to be able to measure how T cell immunity is generated by COVID-19 vaccines, which was not possible in earlier eras when vaccine trials were done for other infections (such as measles, mumps, rubella, pertussis, diphtheria). Antibodies are just the "tip of the iceberg" when assessing the response to vaccination, but were the only arm of the immune response that could be measured following vaccination in the past.
Measuring pathogen-specific T cell responses takes sophisticated technology. However, T cell responses, when assessed years after vaccination for other pathogens, has been shown to be long-lasting. For example, in one study of 56 volunteers who had undergone measles vaccination when they were much younger, strong CD8 and CD4 cell responses to vaccination could be detected up to 34 years later.
REASON #5: T Cell Immunity to Related Coronaviruses That Caused Severe Disease is Long-Lasting
SARS-CoV-2 is a coronavirus that causes severe disease, unlike coronaviruses that cause the common cold. Two other coronaviruses in the recent past caused severe disease, specifically Severely Acute Respiratory Distress Syndrome (SARS) in late 2002-2003 and Middle East Respiratory Syndrome (MERS) in 2011.
A study performed in 2020 demonstrated that the blood of 23 recovered SARS patients possess long-lasting memory T cells that were still reactive to SARS 17 years after the outbreak in 2003. Many scientists expect that T cell immunity to SARS-CoV-2 will be equally durable to that of its cousin.
REASON #6: T Cell Responses from Vaccination and Natural Infection With the Ancestral Strain of COVID-19 Are Robust Against Variants
Even though antibody responses from vaccination may be slightly lower against various COVID-19 variants of concern that have emerged in recent months, T cell immunity after vaccination has been shown to be unperturbed by mutations in the spike protein (in the variants). For instance, T cell responses after mRNA vaccines maintained strong activity against different variants (including P.1 Brazil variant, B.1.1.7 UK variant, B.1.351 South Africa variant and the CA.20.C California variant) in a recent study.
Another study showed that the vaccines generated robust T cell immunity that was unfazed by different variants, including B.1.351 and B.1.1.7. The CD4 and CD8 responses generated after natural infection are equally robust, showing activity against multiple "epitopes" (little segments) of the spike protein of the virus. For instance, CD8 cells responds to 52 epitopes and CD4 cells respond to 57 epitopes across the spike protein, so that a few mutations in the variants cannot knock out such a robust and in-breadth T cell response. Indeed, a recent paper showed that mRNA vaccines were 97.4 percent effective against severe COVID-19 disease in Qatar, even when the majority of circulating virus there was from variants of concern (B.1.351 and B.1.1.7).
REASON #7: Coronaviruses Don't Mutate Quickly Like Influenza, Which Requires Annual Booster Shots
Coronaviruses are RNA viruses, like influenza and HIV (which is actually a retrovirus), but do not mutate as quickly as either one. The reason that coronaviruses don't mutate very rapidly is that their replicating mechanism (polymerase) has a strong proofreading mechanism: If the virus mutates, it usually goes back and self-corrects. Mutations can arise with high rates of replication when transmission is very frequent -- as has been seen in recent months with the emergence of SARS-CoV-2 variants during surges. However, the COVID-19 virus will not be mutating like this when we tamp down transmission with mass vaccination.
In conclusion, I and many of my infectious disease colleagues expect the immunity from natural infection or vaccination to COVID-19 to be durable. Let's put discussion of boosters aside and work hard on global vaccine equity and distribution since the pandemic is not over until it is over for us all.

